Clinical guidelines for the treatment of persons with severe mental illness recommend provider-consumer-family collaboration in all phases of the treatment process (
1,
2,
3). In such collaboration, providers engage consumers and families in the process of treatment planning and share information with families about their relative's mental illness and treatment.
Recommendations encouraging collaboration were recently developed in response to evidence that sharing information with families reduces the frequency of relapse and thereby reduces rehospitalization for persons with severe mental illness (
4,
5,
6). Families who receive information are able to support their ill relative more effectively (
7,
8,
9,
10,
11,
12). Information on the diagnosis, treatment, and prognosis of the relative's illness allows family members to assist their relative in monitoring symptoms and managing medication (
13). Although evidence indicates that collaborative treatment benefits consumers by increasing treatment effectiveness, collaboration is not currently part of routine clinical practice (
14,
15).
Research indicates that attitudes may affect collaboration. Families who have been excluded from the treatment process may be skeptical of building collaborative relationships with providers. Families have reported encountering uncaring staff who leave them feeling frustrated and dissatisfied with the treatment process (
16,
17,
18,
19,
20,
21). When they have voiced their dissatisfaction to providers, the providers have misinterpreted their expressions as reflecting an unwillingness to become involved in their relative's treatment, thus creating a cyclical dynamic of noninvolvement.
Collaboration may also be influenced by consumers' attitudes toward family involvement. Providers may be less likely to discuss family involvement and less likely to ask for permission to release information to families of clients who express negative attitudes toward their family.
However, many mental health agencies do not have clear procedures for releasing information to families. In most states, providing even the most basic information about a client's condition or treatment without the client's consent is technically a breach of confidentiality statutes (personal communication, Ulan H, Sept 1998). Nonetheless, the consent forms in use in many mental health agencies may not be appropriate for obtaining consumers' authorization to release information to their families (
25).
This study examined how mental health care providers discussed confidentiality with consumers and their families. The purpose of the study was to understand the types of information shared and the process by which information was released to families of persons with severe mental illness.
Methods
Sample
Self-administered surveys were distributed at the 1998 annual convention of the National Alliance for the Mentally Ill (NAMI). An additional mailing was sent to 50 NAMI state offices five months later. NAMI members distributed the surveys during support group and educational meetings and also included the survey in NAMI newsletters.
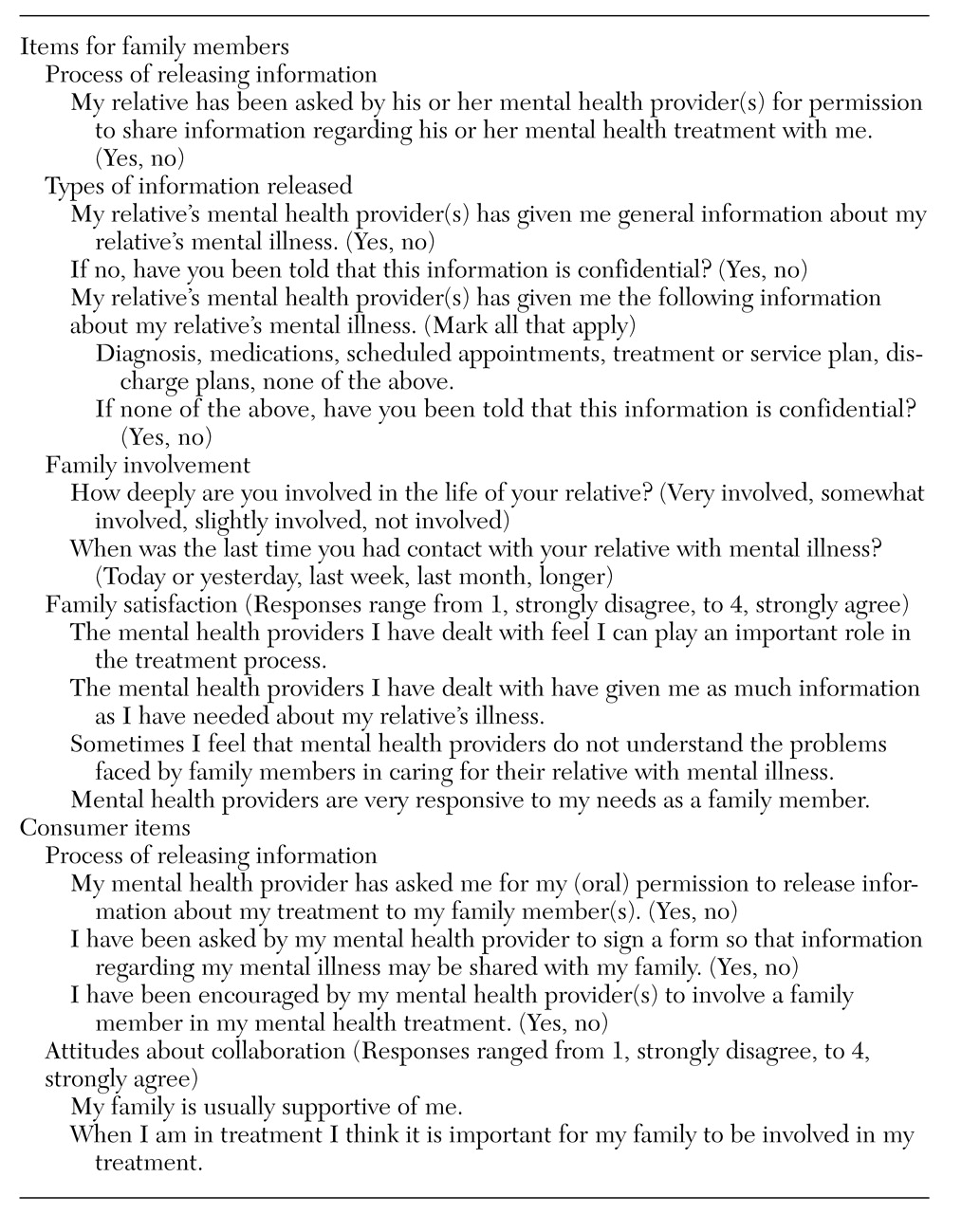
The survey was divided into three sections. Both consumers and family members completed the first section. The next two sections, shown in
Table 1, included questions specifically for either consumers or family members. Respondents who were both consumers and family members were asked to complete all three sections. Data analyses were conducted with and without this subgroup, and no differences were found. For this reason, the subgroup was included in all data analyses.
Measures
Because of the lack of standardized instruments appropriate for this study, the survey items in
Table 1 were developed by the authors. Items to which consumers responded measured the process of releasing information to families and consumers' attitudes toward collaboration. Items to which families responded measured the process for releasing information, the types of information released, and family involvement and satisfaction with providers.
Family satisfaction was measured using four items. Principal-components factor analysis indicated that the four items loaded as a single factor, which was interpreted as measuring family satisfaction with providers. The factor explained 56 percent of the variance. Therefore, responses to the four items were summed to create a satisfaction scale. The Cronbach's alpha for the satisfaction scale was .73.
Measures were pretested with ten families and five consumers. Frequency distributions for the measures indicated sufficient variability within the variables.
Analysis
Descriptive analysis was conducted using SPSS-PC software. Linear regression models were developed to test the hypothesis that when the analysis controlled for race, gender, education, and level of involvement with the ill relative, families who received general or specific information about their relative's mental illness were more likely to be satisfied with mental health providers. Logistic regression models were used to examine the association between consumers' attitudes toward family involvement and whether providers asked for written or oral permission to release information to their families or encouraged consumers to involve a family member in their treatment. Race, gender, and education were included as control variables. Missing data were handled through a process of pairwise deletion.
Results
Sample characteristics
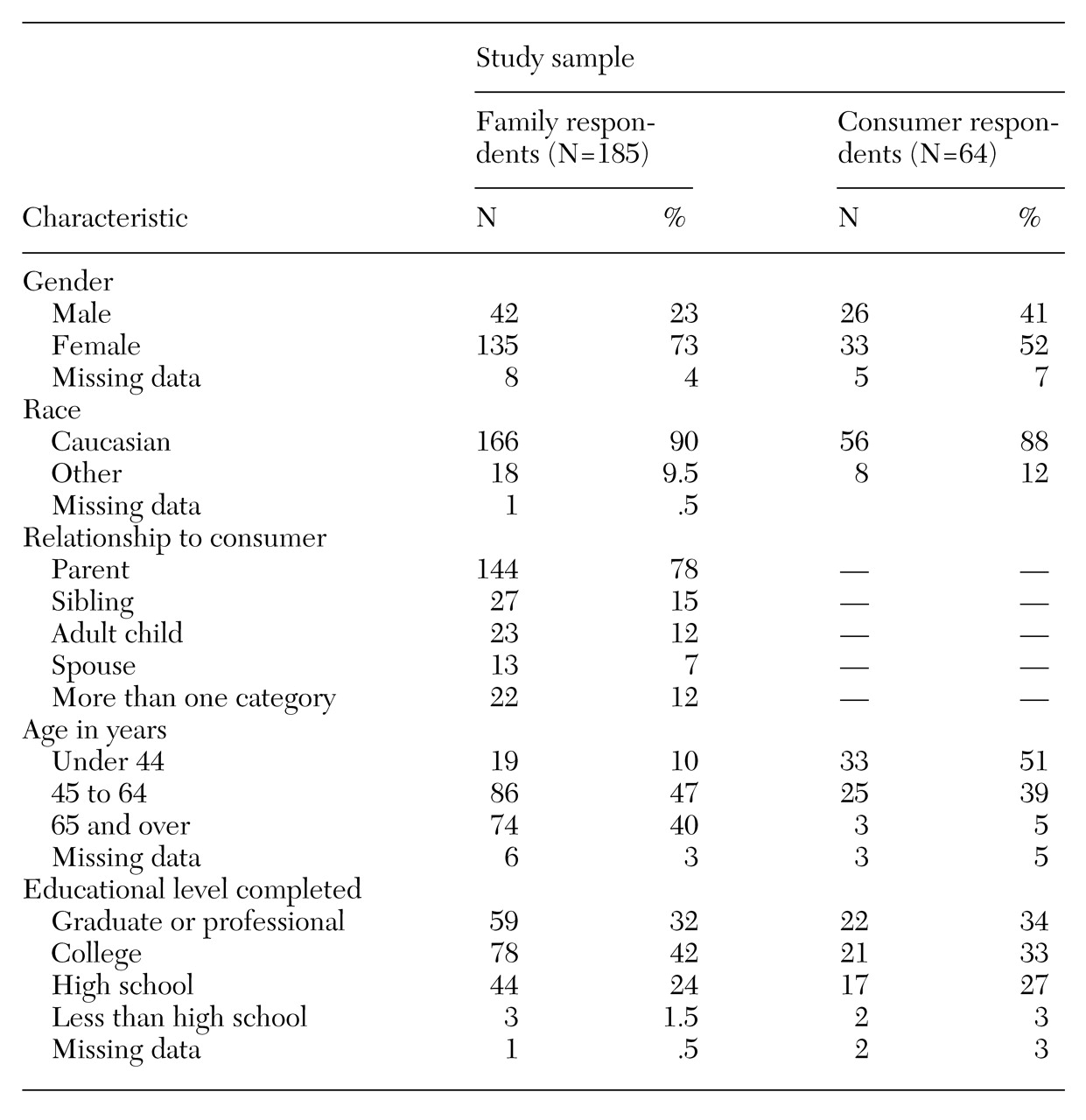
A total of 219 surveys were returned from 185 NAMI family members and 64 NAMI consumers; 30 respondents (14 percent) reported that they were both a family member and a consumer. Thirty states and the District of Columbia were represented in the sample. Most of the respondents were well educated; 90 respondents (41 percent) had finished college, and 72 (33 percent) had earned a graduate or professional degree. The majority of survey respondents were Caucasian (197 respondents, or 90 percent) and female (147 respondents, or 67 percent).
Most of the family respondents (144 respondents, or 78 percent) were parents of adults with severe mental illness. A total of 139 family respondents (75 percent) reported that they were very involved in their ill relative's life; 150 (81 percent) reported having contact with their relative within the past day.
Table 2 presents demographic characteristics of the consumer and family respondents. The sample was similar to the sample in a nationwide study of 1,401 NAMI members (
31). In that study, most respondents were women, most were Caucasian (92 percent), and most were the parent of a person with mental illness (73 percent). In addition, a majority (70 percent) had completed college or graduate school.
Releasing information
Sixteen consumer respondents (25 percent) reported that providers asked for their written permission to disclose information to their family. Thirteen consumers (20 percent) reported that they were asked for their oral permission. Eighty-nine family respondents (48 percent) reported that their relative was asked by his or her mental health provider for permission to share information about treatment. Thirty-eight family respondents (21 percent) said their relative was not asked, and 20 (11 percent) were unsure.
Types of information families receive
A total of 109 family respondents (59 percent) indicated that they received general information from providers about their relative's mental illness. Of the 71 family respondents who did not receive general information, 48 (68 percent) were told that this information was confidential. Most family respondents (133 respondents, or 72 percent) received some specific information about their relative's mental illness. The majority of these respondents reported receiving information about their relative's diagnosis (110 respondents, or 83 percent) and medications (112 respondents, or 84 percent). Forty-three of the 133 family respondents who received information (32 percent) indicated that they received information about their relative's treatment or service plan. Thirty-five of the 52 family respondents who did not receive specific information (67 percent) were told that this information was confidential.
Consumers' attitudes toward collaboration
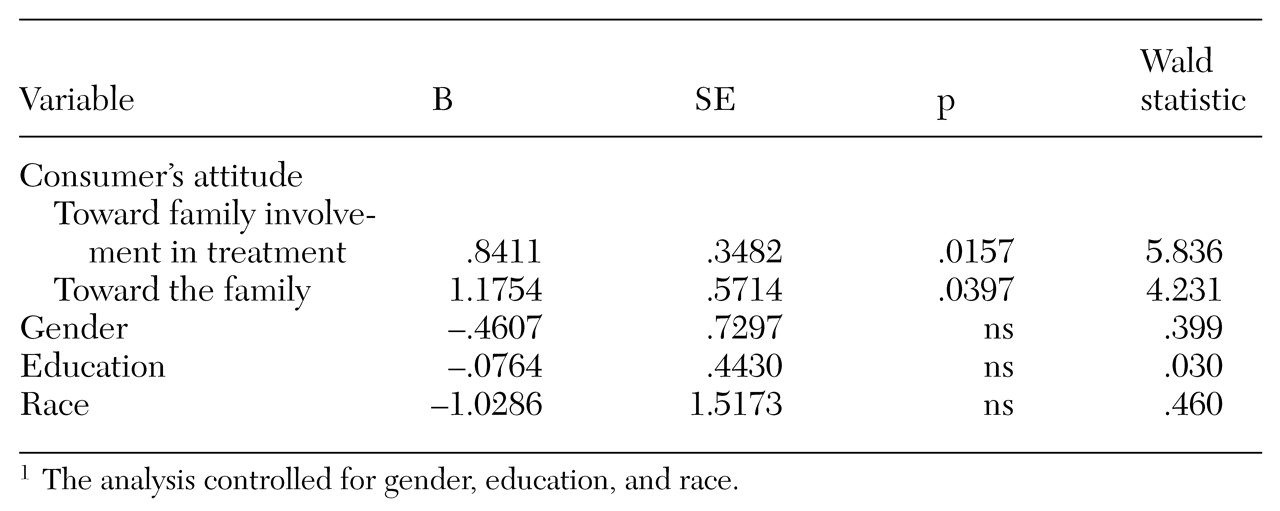
Fifty-one of the consumer respondents (80 percent) reported feeling supported by their family. Thirty-nine consumers (61 percent) reported that they thought it was important for their family to be involved in their treatment. However, only 23 consumers (36 percent) were encouraged by providers to involve a family member in their mental health treatment. A logistic regression model that controlled for race, gender, and education indicated that consumers' attitudes toward their family and toward family involvement were significantly associated with whether consumers were encouraged by their provider to involve a family member in their treatment (χ
2=24.25, df=5, p=.001). Results of this model are summarized in
Table 3.
No significant associations were found between consumers' attitudes toward their family and consumers' attitudes toward family involvement and whether providers asked consumers for their written or oral permission to release information to their family.
Family satisfaction
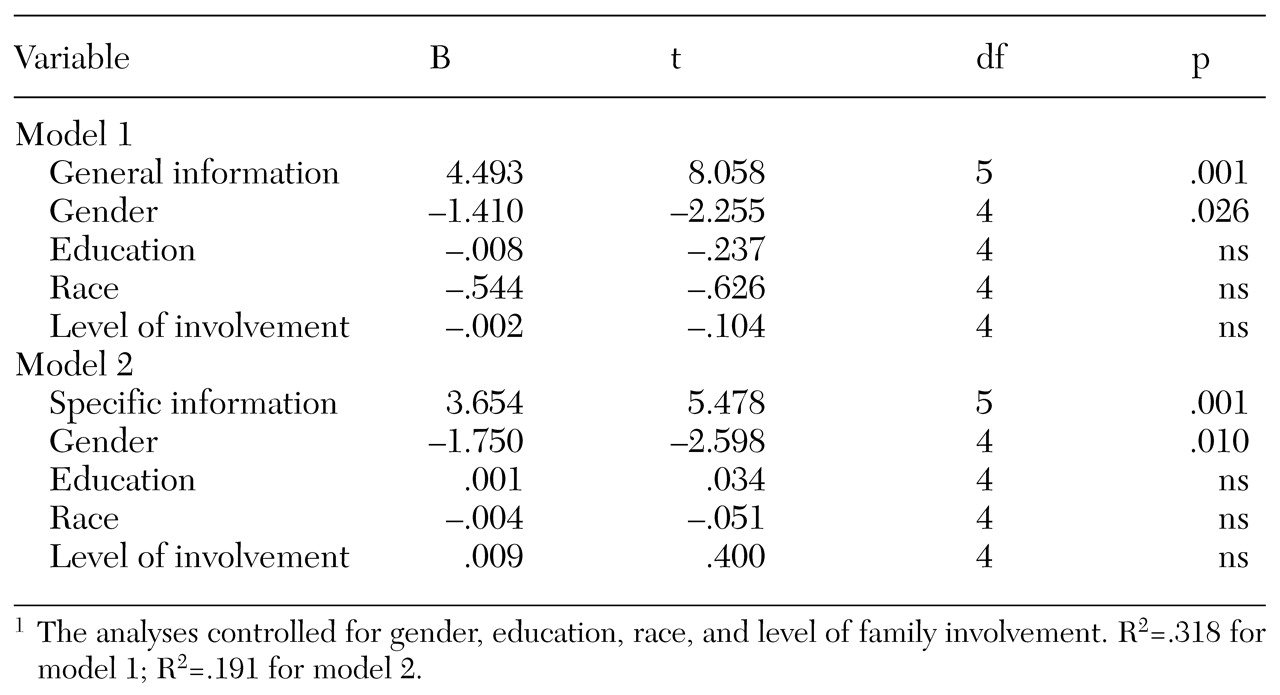
The results of the linear regression models shown in
Table 4 indicated that families who received general or specific information about their relative's mental illness were significantly more likely to report that they were satisfied with mental health providers than those who did not receive information. Males were more likely than females to be satisfied with mental health providers.
Discussion and conclusions
The study was based on a nationwide sample of NAMI members. Like other samples of NAMI members (
31), the study respondents were mostly parents of adults with mental illness, white, and well educated. Because NAMI is a support and education organization, NAMI members have more access to information about mental illness and are more likely to understand the mental health system. Consequently, NAMI members are significantly more likely to report contacts with professionals than are other family members (
32). For these reasons, the study findings are not generalizable to all consumers and family members.
The sample was self-selected and the data were self-reported—two additional limitations of the study. The survey was anonymous, and thus it was not possible to determine whether consumer and family respondents were from the same family in order to assess discrepancies in the data. Future research would be strengthened by adding a provider sample and matching provider, family, and consumer responses.
Because of the exploratory nature of the study, the instrument was kept brief. Other variables that might be included in a more in-depth analysis of this issue are consumer diagnosis, severity of illness, and length of time since onset of the illness. Each of these variables may affect the process of releasing information to families.
What types of information are released?
The finding that the majority of family members in this study had received information about their ill relative's diagnosis and medications is encouraging and reflects progress toward more widespread provider-consumer-family collaboration. However, considering that the sample consisted of NAMI members, it is surprising that few families had received information about their ill relative's treatment plan. NAMI members have been shown to be significantly more likely than other families to have contact with their relatives' providers. One possible explanation for the finding is that information about diagnosis and medications may be shared with families at the time of the relative's intake into the mental health system; however, providers may not establish an ongoing collaborative relationship. Giving information about the treatment plan to families may require a deeper level of involvement between providers, consumers, and families.
These findings raise important questions about the current process of provider-consumer-family collaboration. At what point or points in the process do families typically receive information? Are there gender differences associated with the way that providers and families interact? Are mental health programs designed so that it is possible to include families in treatment planning? Are providers compensated (either reimbursed or allotted time) for collaborating with families? Further research is needed to explore these questions.
Who initiates the process?
Even though a large number of family respondents reported that they received some information from providers, many were not satisfied with their contact with providers. Unsolicited comments on the surveys suggested that the process of obtaining information was often initiated by consumers or family members and required much personal effort. In unsolicited comments, six respondents described the burden of having to learn the types of questions to ask in order to understand the mental health system and the treatment that their relative was receiving. Because information about most physical health problems may be released to a person's next of kin without his or her consent, consumers and families entering the mental health system are not likely to be aware of the need to initiate the release process to receive essential treatment information.
The following comments from a family respondent suggest that because a consumer's consent is needed to release information, families expect providers to initiate the release process. "My daughter was a patient at Hospital X three times in 1998. Twice when I inquired about her condition or asked to speak with her, I was told that I wasn't even supposed to know if my daughter was a patient. When a patient is interviewed on admittance, during the interview did anyone ask my daughter's permission to advise me, her mother, of her whereabouts? Whatever happened to common sense? Suppose, heaven forbid, something tragic had happened, then they would have told me—too late!"
Current treatment guidelines for severe mental illness recommend involving family members in all aspects of the treatment process. However, these findings suggest that even NAMI family members may be having a hard time becoming involved in their relative's treatment on an ongoing basis.
Whose decision is it to release information?
Even though the consumers in this study were affiliated with NAMI and reported a high degree of family support, few indicated that they were asked for permission to release information to their families. The data from family respondents supported the idea that many consumers are not asked for their permission before specific information about their illness is released to family members. These findings suggest that providers, consumers, and families are not working together as collaboratively as they could. The results also raise questions about how state statutes on confidentiality are interpreted by local agencies in regard to the release of information to families.
Variations within agencies may be promoting the perception among family members that providers hide behind a veil of confidentiality to avoid collaborating with family members (
26,
27,
33). Although the majority of family respondents who did not receive specific information were correctly told that this information—diagnosis, medications, and the treatment or service plan—is confidential, most family respondents who did not receive general information about mental illness were told that general information was confidential. The findings suggest that confusion exists among providers, consumers, and families about the types of information that are confidential and those that are not.
Unsolicited comments received from 11 family respondents suggest that the release process may vary according to providers' interpretation of confidentiality policies. These family respondents reported that some providers released information to them while others did not. Some family members explained that their ill relative changed providers until he or she found a provider who allowed family involvement. Some of this variation in the release of information may be due to the absence of clear procedures and consent forms in many mental health systems (
19).
Two hypotheses were tested to examine factors that may influence the process of collaboration and release of information to families. It was hypothesized that providers may be more likely to ask permission (oral or written) for releasing information to families from consumers who express more positive attitudes toward family collaboration. The results did not support this hypothesis. However, the findings showed that consumers' attitudes toward family involvement were positively associated with whether providers encouraged consumers to involve a family member in their treatment.
Research and practice implications
Research is needed to understand the current process used to release information to families, including how the process is initiated, how state statutes are interpreted, and how agency policies on confidentiality are implemented. The processes that are currently employed should be evaluated for their effectiveness in meeting the recommendations for provider-consumer-family collaboration that are outlined as best practices for the treatment of persons with severe mental illness.
Training for providers, consumers, and families is needed to clarify the types of information that are confidential and nonconfidential and the process for releasing confidential information. Training should emphasize that the choice to protect or release confidential information should be the consumer's decision and that collaborative treatment involves providers, consumers, and families working together.