Violent behavior by psychiatric patients poses a considerable challenge to psychiatric staff and health planners because of the risks to the individuals involved in violent incidents and the implications of those risks for the organization of services (
1). Estimates of violence in inpatient settings have varied widely, from .07 to 7.9 violent incidents per patient per year (
2,
3), and some evidence has suggested that inpatient violence is increasing (
4,
5). Violence in psychiatric settings causes a considerable drain on resources. The yearly cost of assaults on staff in the United Kingdom's National Health Service has been estimated to exceed $45 million (
6).
Prediction of violence has been shown repeatedly to be a difficult clinical task, and the accuracy of such predictions has usually been deemed poor (
7,
8), although a recent study reported more accurate prediction by clinicians in a forensic unit (
9). Some researchers have proposed that actuarial methods—risk assessment based on statistical data—can enhance clinical assessments of potential for violence, which have traditionally been based on reviews by multidisciplinary staff (
8,
10).
Because there is no generally accepted definition of violence in psychiatric settings, comparison of previous studies' findings is difficult. Previous studies have focused on verbal abuse or threatening behavior (
9,
11), damage to property (
12), self-harm (
2), physical attacks on others (
13,
14), and attacks on health care staff (
15,
16). Difficulties in comparing research findings also arise from differences in study populations (
2,
14,
17,
18,
19) and settings (
2,
9,
17). An additional problem is that most studies have not compared the characteristics of violent patients with those of nonviolent patients (
2,
12,
15). Thus it is not surprising that an earlier study found more patients with schizophrenia among the violent patients in a hospital where schizophrenia was the most common diagnosis (
15).
In the retrospective case-controlled study reported here, we compared patients who committed violence in an acute adult psychiatric inpatient setting with all patients admitted during the study period as well as with a randomly selected sample of nonviolent patients. The goal of the study was to identify risk factors and correlates of violence in this acute care setting.
Methods
The study was done on an acute adult psychiatric unit in a district general hospital in Dartford, England. The hospital served a well-defined catchment area with a population of 220,000. The unit consisted of three open wards with 53 beds and a locked intensive care ward with eight beds. Patients were admitted to the unit from the hospital's accident and emergency department or were referred by one of three community mental health teams serving the catchment area or by the hospital's outpatient mental health clinics. Only patients who posed a significant risk to themselves or others were confined to the locked ward.
For this study, violence was operationally defined as any incident in which a patient attempted to physically harm others, such as hospital staff members, other patients, or visitors, or attempted to damage property. Incidents of verbal hostility and self-harm were excluded unless concomitant physical violence toward others or toward property also took place.
Details of violent incidents were extracted from standard forms that were completed by nursing staff for every incident on the unit that involved potential harm to the violent patient, to others, or to property. Hospital policy required completion of these forms for every violent incident. Data for this study were based on forms completed from April 1, 1997, to March 31, 1998.
We rated the severity of violence with the Staff Observation Aggression Scale (
20). In first-degree violence, property that was the object of violence showed no visible damage and could still be used. Persons who were the object of violence felt threatened or had physical pain but had no visible injury. In second-degree violence, property needed to be replaced. Persons sustained visible injuries but did not require treatment. In third-degree violence, persons sustained injuries that required treatment.
The data analysis had three stages. First, we determined the characteristics of the violent incidents, including the date, time, and place the incident occurred; whether the target of violence was a staff member, another patient, or property; and the incident's degree of severity. We found that information about the immediate precipitants of or provocation for violent incidents was not regularly or reliably recorded on the incident forms, and therefore these data were not analyzed.
Second, we screened the case notes for all patients admitted to the hospital during the study period (N=474) to identify any evidence that the patient showed violent or aggressive behavior during the index admission. As a result, two patients were added to the group of violent patients identified through the incident forms, for a total of 49 violent patients. A group of 280 nonviolent patients was identified by excluding patients who committed any type of aggressive behavior, such as suicide attempts or verbal abuse, and by excluding all patients who were readmitted during the study period. The violent group was compared with the group of all admissions and with the nonviolent group on age, sex, ICD-10 diagnosis, and length of stay. In the comparison of the violent and nonviolent groups, for patients who had been readmitted during the study period, the longest admission was used for comparison of length of stay.
During this stage of the analysis, the first author reviewed the case notes for all inpatients and discussed selected patients' cases with clinical team members in order to verify all psychiatric diagnoses according to ICD-10 criteria. To determine the reliability of the clinical records, he also interviewed 30 patients and compared information from the interviews with information recorded in the case notes about history of violence, self-harm, alcohol abuse or dependence, and drug abuse or dependence. The kappa coefficients for comparison of data on the four clinical variables were .66, .92, .82, and .67, respectively, indicating the reliability of clinical records.
In the third stage of the analysis, the violent group was compared with a computer-identified random sample of nonviolent patients (N=140) on type and cause of admission and history of violence, alcohol or drug abuse, and self-harm. Data on patients' histories were extracted from clinical records by a nurse colleague who was blind to patients' allocation to the violent or nonviolent group.
Data on medication received by the two groups of patients at discharge were also compared. These data included regular and as-needed (p.r.n.) antipsychotic medications in chlorpromazine-equivalent daily dosages, daily dosage of antidepressants and the percentage of the maximum daily dosage for antidepressants established by the British National Formulary (
21), and p.r.n. diazepam-equivalent daily dosages of benzodiazepines. Data on the use of augmentation therapy such as lithium or anticonvulsants, the number of medication changes during the last six months before discharge, and the number of drugs from the medication class received by the patients (for example, two or more antipsychotic medications) were also compared.
Data were analyzed with the SPSS statistical package, version 9. Differences between groups were tested for statistical significance by using chi square tests for categorical variables. The Mann-Whitney U test and Kruskal-Wallis test were used for continuous variables because these tests are more appropriate for skewed data. Logistic regression analysis with forward and backward stepwise methods was used to test the predictive power of related variables.
We found a high correlation between p.r.n. daily doses of antipsychotic medications and benzodiazepines in the violent and nonviolent patient groups (N=189; r=.81). Therefore, these data were factor analyzed, and a single component encompassing these two variables was entered into the regression model.
Results
Forty-nine patients committed 104 violent incidents during the study period, resulting in an incidence rate of .22 violent incidents per admission per year. Seven patients (14.3 percent of the violent patients) committed 50 incidents (48.1 percent of the violent incidents). Male patients committed 59 incidents (56.7 percent of the incidents). The majority of incidents were directed against property (67 incidents, or 64.4 percent), followed by incidents against staff members (29, or 27.8 percent) and against other patients (15, or 14.4 percent). Some incidents involved more than one target.
The vast majority of incidents were of minor severity. Forty-five incidents (43.2 percent) were of the first degree of severity, and 52 incidents (50 percent) were of the second degree. Only seven incidents (6.7 percent) were of the third degree of severity. Most incidents occurred in sitting rooms (52, or 50 percent) or ward corridors (24, or 23.1 percent). Peak times for occurrence of violent incidents were during the night hours of 5 p.m. to midnight (57 incidents, or 54.8 percent) and on weekends (38, or 36.5 percent).
Male patients made up 57.1 percent (N=28) of the violent group, compared with 50.4 percent (N=239) of the 474 total admissions and 54.3 percent (N=152) of the 280 nonviolent patients, but the difference was not statistically significant. The mean ±SD age of the violent patients was 34.4±10 years, compared with 39.6± 13 years for all admissions and 40± 13.2 years for the nonviolent patients (Kruskal-Wallis, χ2=7.52, df=2, p= .02). The mean±SD length of hospital stay for the three groups was 104.5± 83.6 days, 36.4±12.9 days, and 31.2± 35 days, respectively (Kruskal-Wallis χ2=58.3, df=2, p<.001). The mean± SD time from admission to the first violent incident was 38±41 days (median=25 days, 70th percentile=39 days).
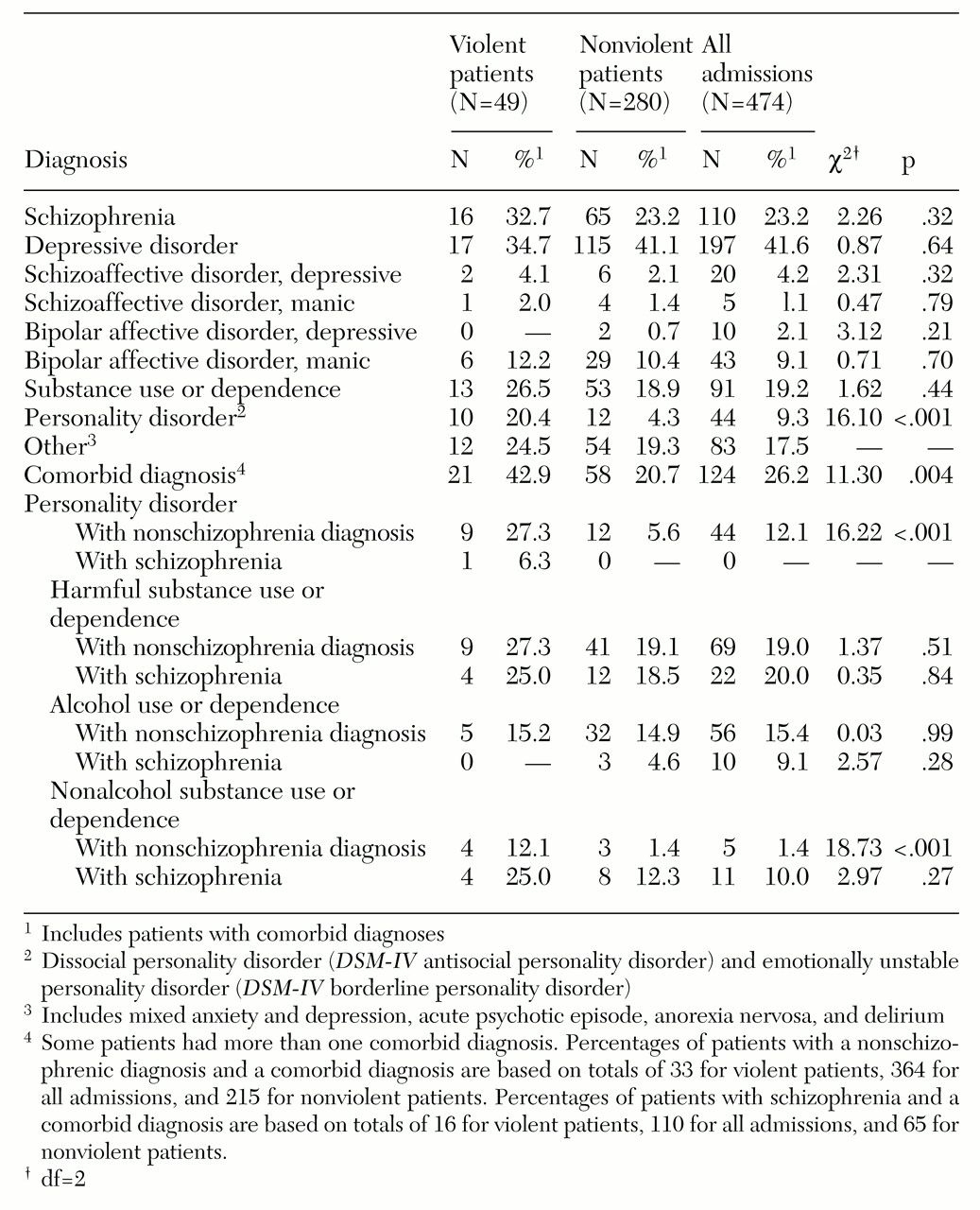
Table 1 shows that only dissocial and emotionally unstable personality disorders (equivalent to
DSM-IV antisocial and borderline personality disorders) and comorbid diagnoses were significantly more likely to occur in the group of 49 violent patients than in the group of 280 nonviolent patients. Comorbid personality disorder or nonalcohol substance abuse were significantly more likely to occur among violent patients with nonschizophrenia disorders than among nonviolent patients with nonschizophrenia disorders, but these comorbid disorders were similarly likely to occur among violent and nonviolent patients with schizophrenia.
As
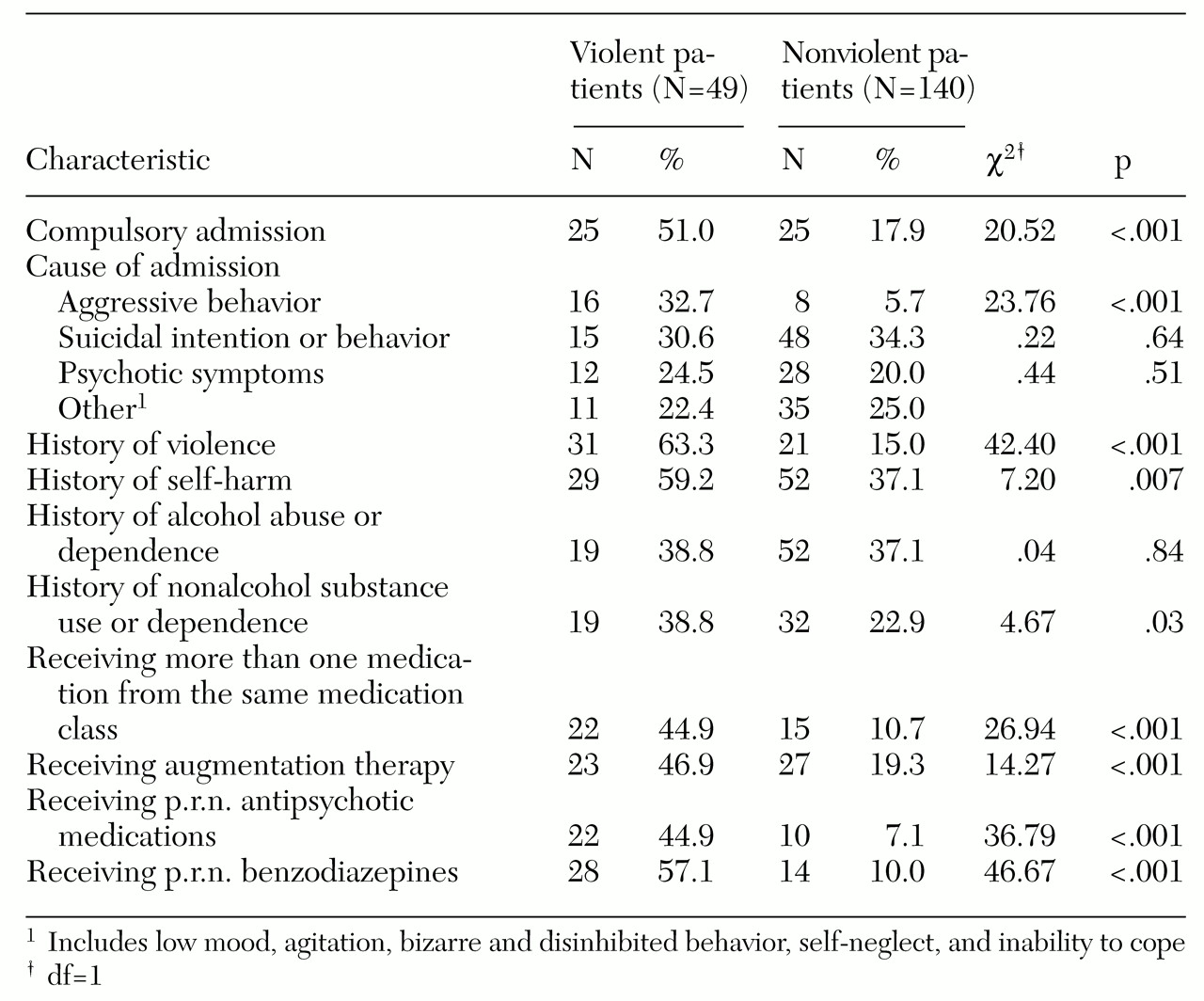
Table 2 shows, compared with the 140 nonviolent patients in the randomly selected comparison group, the 49 violent patients were significantly more likely to have a history of violence and nonalcohol substance abuse, to have behaved aggressively before admission, and to have had a compulsory admission. The violent group was also significantly more likely to have a history of self-harm, to be receiving augmentation therapy and more than one drug from a class of medication, and to have prescriptions for p.r.n. antipsychotic medications and p.r.n. benzodiazepines.
Compared with the nonviolent patients, the violent patients were prescribed a significantly higher mean± SD daily dosage of antipsychotic medication (1,074.4±1,038 mg chlorpromazine equivalents, compared with 484±516.9 mg for the nonviolent patients; Mann-Whitney U=607.5, p=.002). They received a nonsignificantly higher percentage of the maximum antidepressant dosage established by the British National Formulary (60.7 percent±30.5 percent, compared with 49.4 percent±24 percent for the nonviolent patients).
The violent group were prescribed a significantly higher mean±SD daily dosage of p.r.n. antipsychotic medication (671±528.5 mg chlorpromazine equivalents, compared with 347.5± 347 mg for the nonviolent patients; U=53, p=.02) and of p.r.n. benzodiazepines (56.1±41.1 mg diazepam equivalents, compared with 19.6± 20.9 mg for the nonviolent patients; U=79, p=.001). The violent group also had a significantly higher number of medication changes (.7±.9, compared with .02±.57 for the nonviolent patients; U=2018.5, p<.001).
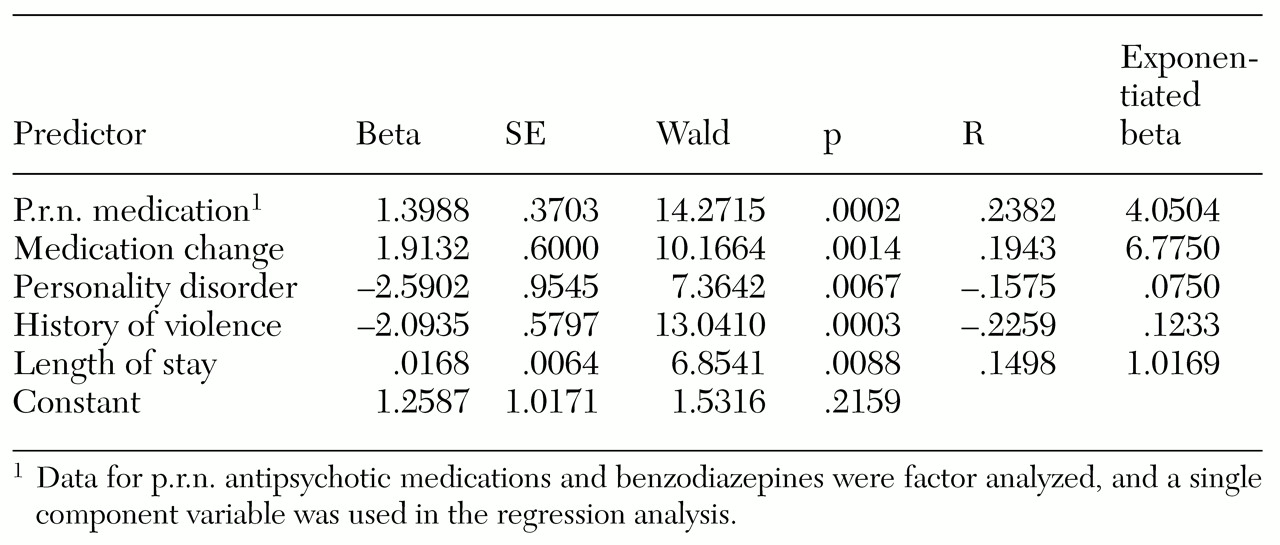
As shown in
Table 3, stepwise logistic regression analysis identified the following predictors of violence: medication changes, use of p.r.n. medication, past violent behavior, personality disorder, and length of hospital stay. Prediction of violence using these variables together had a sensitivity of 76 percent, a specificity of 97 percent, an accuracy of 92 percent, and a positive predictive value of 90 percent. Prediction that used medication changes and use of p.r.n. medication together had a sensitivity of 61 percent, a specificity of 96 percent, and a positive predictive value of 86 percent. Prediction of violence based on past violence alone had a 63 percent sensitivity, an 85 percent specificity, and a 60 percent positive predictive value.
Discussion
This study of violence in an inpatient setting differs from previous work in comparing violent patients with all admissions during the study period. The study's findings replicate some findings of earlier studies and also show some important differences.
A major result of this study is its failure to replicate previous findings of a positive association between schizophrenia and violence (
15,
22,
23,
24). Although some earlier research failed to find this association (
3,
25), the study reported here lends considerable weight to this observation because the violent patients were compared with the entire inpatient population. We also found no evidence of a negative association between depression and violence, as observed earlier (
5). In our study, depression was the most prevalent diagnosis in both the violent and the nonviolent groups.
Suicidal behavior as a reason for admission did not predict violence during the hospital stay. However, inpatient violence was associated with past suicide attempts and past violent behavior. These associations suggest that violence, or aggression directed outward, may be a good predictor of suicidal behavior, or aggression directed inward, although the reverse association does not appear to hold true. This observation has implications for the ongoing debate about the social and biological correlates of impulsivity and aggressive behavior (
26). People who already exhibit poor impulse control for violence toward others, as suggested by their history of violence, may also show poor impulse control for suicidal behavior, although those with a history of suicidal behavior may be able to control impulses for violence toward others. Unfortunately, our understanding of the serotonergic and other biological mechanisms underlying the relationship between impulsivity and aggression is not sophisticated enough to clarify this apparent selectivity in the link between violence and suicidal behavior (
26,
27).
Another important finding was the strong association between violent incidents and a prolonged hospital stay. This association can be explained in several ways. For example, the length of hospital stay may be determined by the level of disturbance that patients show (
13,
28), and violence may have reflected a high level of disturbance in the violent group. The presence of a high level of disturbance among the violent patients was also supported by their significantly higher rates of comorbid diagnoses and may also explain their poor response to treatment, as reflected in the higher doses and use of a greater number of regular and p.r.n. medications, greater likelihood of augmentation therapy, and greater number of medication changes in the violent group.
Alternatively, long hospitalization itself might have contributed to violence in a substantial minority of patients. However, more than 70 percent of violent patients had been hospitalized less than six weeks before the first violent incident, which suggests that for the majority of violent patients, length of hospitalization did not contribute to violent behavior. In any case, a prolonged hospital stay has serious implications for allocation of treatment resources.
Frequent medication changes and the need for p.r.n. medication were powerful correlates of violence in this study. These variables reflect high levels of aggression and anxiety. High levels of aggression and anxiety assessed on referral have been recognized as predictors of subsequent inpatient violence (
29). Although these symptoms are most likely consequences of violence, they can serve as useful predictors of subsequent episodes of violence if other sources of information are not available.
Our results support previous observations that a history of violence remains the most consistent predictor of violence (
11,
29,
30,
31,
32). The fact that a minority of inpatients committed a large proportion of the violent incidents has also been a consistent finding (
2,
12,
17,
22,
24,
33).
As in earlier research (
14,
32,
34), gender was not significantly associated with violence in our study. However, several studies have reported a higher rate of violence among female patients than among male patients (
17,
22,
35), and others have found a higher rate among male patients (
11,
16,
36). It is possible that gender itself is not an important risk factor for violence among inpatients and that other factors, such as type of patient population, study setting, patients' underlying psychopathology, and situational variables, may be more crucial determinants. Association of younger age with a higher rate of violence has been consistently reported (
5,
11,
22).
The finding that personality disorders were more prevalent among violent inpatients is consistent with other reports (
19,
37). The higher prevalence of nonalcohol substance abuse among the violent patients supports an earlier suggestion by Palmstierna and Wistedt (
38) that abuse of drugs other than alcohol was significantly correlated with aggressive behavior during the first 28 days of admission.
We found higher rates of comorbid personality disorder and substance abuse among violent patients without schizophrenia, but not among violent patients with schizophrenia. In earlier studies, patients with schizophrenia who showed violent behavior had higher levels of psychopathy (
19), and patients with schizophrenia and substance abuse showed higher rates of violence (
39,
40). Fewer incidents of personality disorder and substance abuse among the patients with schizophrenia in this study may partly explain the lower occurrence of violence in this group. The possibility that factors other than schizophrenia itself may be important determinants of violence in this group is supported by a previous finding that early onset of substance abuse was associated with violence among chronically mentally ill patients (
41). This finding suggests that at least some causal factors of violence may precede the onset of adult mental illness.
The finding that violent patients were more likely to be compulsorily admitted has also been reported (
5,
11,
32). It is important to note that violence may be a consequence as well as a cause of compulsory detention.
The estimated rate of violence of .22 violent incidents per admission per year is not a true reflection of potentially violent incidents, as our study design did not include aggression preempted by staff vigilance and early intervention. The peak times for occurrences of violent incidents in our study—evenings and weekends—contradict earlier observations (
17,
42). This difference may largely reflect the practice culture of our service, in which the number of staff and the amount of staff-patient interaction are decreased during the evenings and the weekends.
The findings that most incidents were minor and that serious incidents were rare are in keeping with other reports (
20,
22). However, many potentially serious incidents may lead to minor outcomes when they miss the target. Taking this possibility into consideration, other studies have interpreted incidents such as touching in a threatening way as serious and have consequently reported a higher rate of violent incidents (
11). From this perspective, the majority of incidents in our study would be considered quite serious.
The retrospective design of this study may have resulted in underreporting of violence, as suggested in earlier research (
43), but our extensive search of clinical records added only two more patients to the violent group originally identified through the incident reports, suggesting a very small possibility of underreporting in both sources. Another potential problem was the accuracy of the retrospective data, but the high kappa coefficient values in the comparison of interview-based and record-based information suggested that the records were reliable. Data were not collected on immediate precipitants and antecedents of violence.
The possibility of underreporting also implies that some violent patients might have been erroneously included in our comparison group. However, we restricted the definition of a violent incident to an actual attempt to physically harm others or damage property and left out threatening behavior or verbal abuse. In this way we avoided taking into account the kind of aggression that is most likely to go unrecorded in hospital documents. The restricted definition also focused on the characteristics of more seriously violent patients. Furthermore, erroneous inclusion of violent patients in the nonviolent group would tend to obscure the differences between groups. Therefore, the differences we have found should be considered reliable, although possibly of a smaller magnitude than those actually present in the study group.
Conclusions
The findings of this study suggest four conclusions. First, a high risk of inpatient violence is associated with previous violence, underlying dissocial or emotionally unstable personality disorder (antisocial or borderline personality disorder), comorbid diagnoses, compulsory admission, past self-harm, and nonalcohol drug abuse. Second, violence is correlated with longer hospitalization, greater need for sedative medication, and frequent medication changes, all of which have serious cost implications. Medication variables could be useful predictors of inpatient violence, especially when no information about risk factors is available.
Third, case-control observation does not support a positive association of inpatient violence with schizophrenia or a negative association with depression. Factors other than mental illness may be more crucial determinants of violence in acute inpatient settings. Finally, the reasons for repeated acts of violence by a small group of inpatients remain poorly understood. Further quantitative and qualitative research involving these challenging patients is needed.
Acknowledgments
The authors thank Anna-Maria Killeen for help with data collection and database entries and Linda Atkinson, Pamela Merser, Pauline Page, and Lynne Byfield of the medical records department of the Thames Gateway National Health Service Trust.