A growing number of states and counties are using managed care to provide mental health services to individuals who receive public funding (
1). As the number of public managed care plans increases, so does the need for information about how municipalities engage, enroll, and manage care for patients who are mentally ill. It can be argued that the need for emergency psychiatric care can serve as a proxy for either insufficient access to outpatient treatment or inadequate outpatient care. Thus understanding the characteristics of patients in these plans who need emergency care provides a perspective on the kinds of patients for whom publicly funded managed care plans have increased or decreased access to care.
Many factors are associated with the use of psychiatric emergency room services, including homelessness (
2), substance abuse (
3), ethnicity (
4), disability benefits (
5), aggressive behavior (
6), and psychosocial issues, such as unmet needs for safety, money, and employment (
7). The results of two studies (
8,
9) indicate that patients' current involvement in outpatient treatment usually can serve as a predictor of their future use of emergency services. However, few studies have examined emergency psychiatric patients in public managed care plans, and no published study has examined a cohort of such patients to determine what proportion are already in treatment and whether those who are in treatment have different service needs than those who are not in treatment.
Our study took place at Harborview Medical Center, a large public hospital in Seattle that is owned by King County and managed and staffed by the University of Washington. Patients who present with psychiatric emergencies are seen in the hospital's crisis triage unit, which has 24-hour in-house coverage by attending or resident psychiatrists, nurses, social workers, and addiction professionals. Although the Seattle metropolitan area has a number of other hospitals, this unit handles the majority of acute and emergency psychiatric care.
The Harborview crisis triage unit was designed to be a single portal to multiple programs in the regional support network prepaid managed mental health care plan that provide mental health and substance abuse services. The mission of the regional support network plan is to provide, within the constraints of limited funding, care for individuals who have acute and chronic mental illnesses. Therefore, examining the proportion of crisis triage unit patients who are already enrolled in the managed care network—as well as the characteristics of the entire population presenting to the unit—offered a unique opportunity to understand what kinds of patients are being reached by the regional support network plan and what kinds may be "falling through the cracks."
The regional support network plan in King County is directed by the county mental health department and administered on contract by a private managed behavioral health care company. The plan pays for outpatient treatment on a yearly risk-adjusted case rate basis for enrolled clients, such that individuals with the most severe illnesses are paid for at about three times the rate of those with illnesses of moderate severity and ten times the rate of those with illnesses of milder severity.
We were interested in determining what proportions of patients who visited the crisis triage unit were currently enrolled in the regional support network plan, had been previously enrolled (enrolled during the past five years but not currently enrolled), and had never been enrolled. We also examined the demographic, psychiatric, and substance use characteristics of patients at admission to the unit.
Methods
Subjects
Data were obtained from 2,419 consecutive patients who visited the crisis triage unit between July 1998 and February 1999. Patients were considered to have received outpatient treatment if they were currently enrolled in the regional support network plan, as enrollment occurs only if patients receive care. To be eligible for enrollment, patients must either be receiving or be eligible for Medicaid funding or be severely mentally ill and have a very low income. Although many patients seen in the crisis triage unit receive Medicaid benefits, many others do not because of a short duration of economic needs or low severity of illness.
Patients who are enrolled in the regional support network plan are assigned a severity level or tier according to a structured evaluation of symptoms and function. Tier rankings are 1B, 2, 3A, and 3B (
10). These tiers also require a certain level of service to determine the annual payment. We compared the proportion of enrolled patients in the four tiers to determine whether certain kinds of enrolled patients were disproportionately represented among those who were seen in the crisis triage unit.
Assessments
The 2,419 patients had a
DSM-IV psychiatric diagnosis, as determined by a semistructured interview. The Emergency Trauma Center Assessment Form, which has been found to be valid and reliable (
11), was completed during each patient's evaluation and provided scaled ratings for 11 variables. Clinical psychiatric variables included psychosis, depression, anxiety, hostility, uncooperativeness, and suicidality. Substance use ratings included patient intoxication at presentation to the crisis triage unit, current intravenous drug use, severity of substance abuse, and readiness for change. Disability ratings included comorbidity of medical illness, dysfunction in activities of daily living, social role dysfunction, lack of social supports, and functional status based on the Global Assessment of Functioning (GAF).
All of the ratings except the GAF were made on scales running from 0 to 6 that were modeled after items used in the Psychiatric Symptom Assessment Scale (
12) and the Psychiatric Assessment Form (
13), in which 0 indicates no problem; 1 to 2, mild symptoms; 3 to 4, moderate symptoms; and 5 to 6, severe symptoms. Each severity rating includes a behaviorally anchored set of descriptors.
Administrative and service variables included the source of the patient's referral to the crisis triage unit, concurrent participation in public substance abuse treatment programs, involvement in outpatient mental health treatment, referral for inpatient hospitalization, a crisis intervention visit within 19 days after the initial visit, time spent in the crisis triage unit, and a discharge against medical advice from the unit. Services history—lifetime and past year—included the number of previous psychiatric hospitalizations, involuntary psychiatric hospitalizations, incarcerations, and episodes of substance abuse treatment.
Statistical analyses
To describe differences among the three groups—currently, previously, or never enrolled in the prepaid health plan—univariate statistical tests were performed on all variables, with an alpha level of .001 or less for statistical significance after a Bonferroni correction. In the event of a significant test result, post hoc t tests were performed to determine which group differences were responsible for the statistical significance. The other p values are presented for descriptive purposes only. Chi square tests were used for discrete variables, and one-way analysis of variance was used for continuous variables. In the event of a significant finding, three planned comparisons were performed to determine which group differences produced the statistical significance, with a Bonferroni correction (p<.001) also applied.
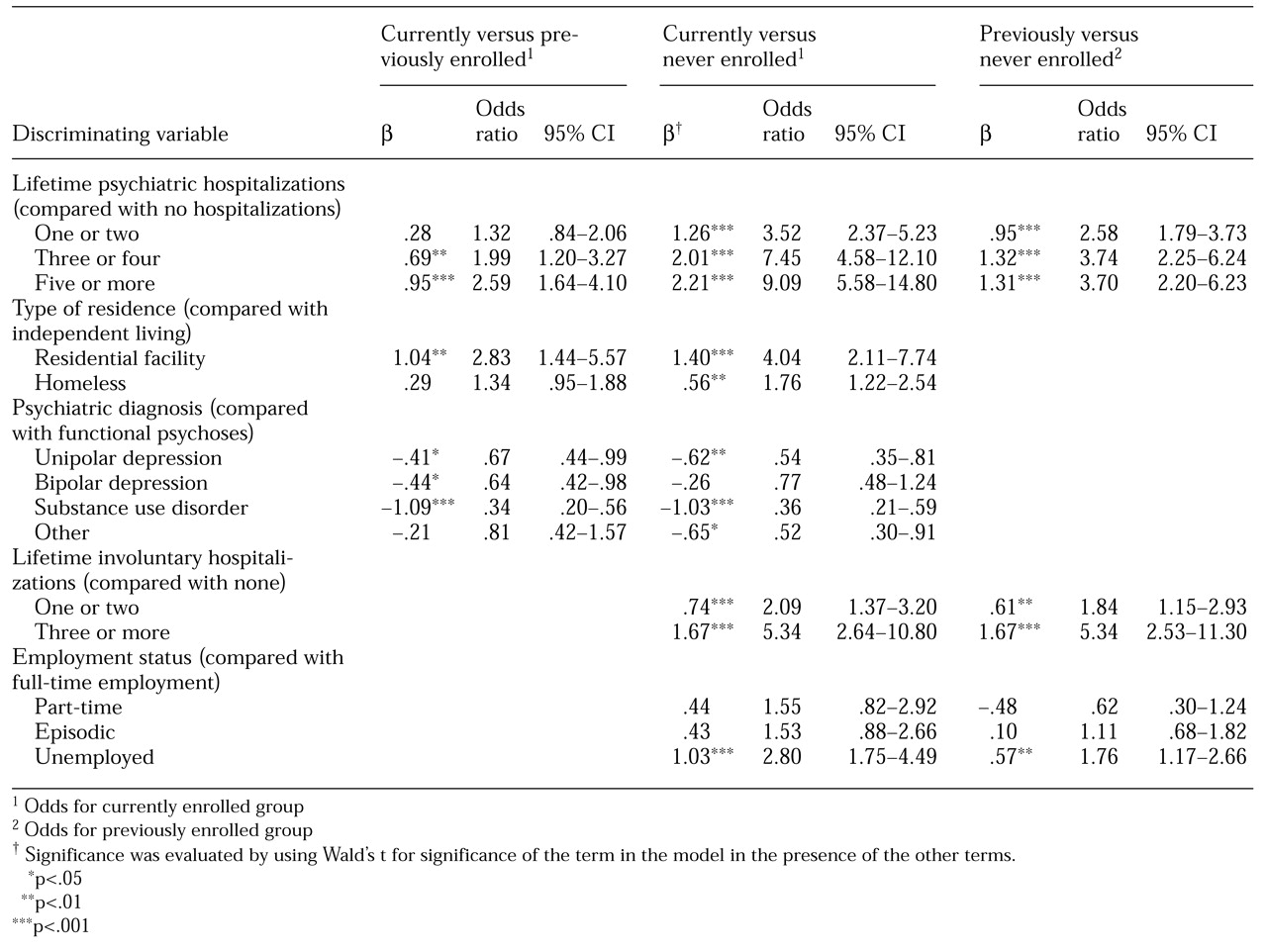
Three logistic regression models were developed to determine the most salient and independent factors that differentiated three pairs of groups: currently enrolled versus previously enrolled, currently enrolled versus never enrolled, and previously enrolled versus never enrolled. The models were created by using both stepwise and backward elimination techniques. For each model, only the variables that differed between the three paired groups at a significance level of .001 or less were included as potential discriminators. The final models for each pair of groups contained only significant variables. The purpose of these analyses was not to predict group membership but rather to determine the factors that independently differentiated the three groups.
Results
Of the 2,419 patients seen in the crisis triage unit during the study period, 640 (26 percent) were currently enrolled in the regional support network plan, 378 (16 percent) were previously enrolled, and 1,401 (58 percent) were never enrolled. Significantly more 3A and 3B patients—that is, more seriously ill patients—were seen (χ2=256, df=6, p<.001).
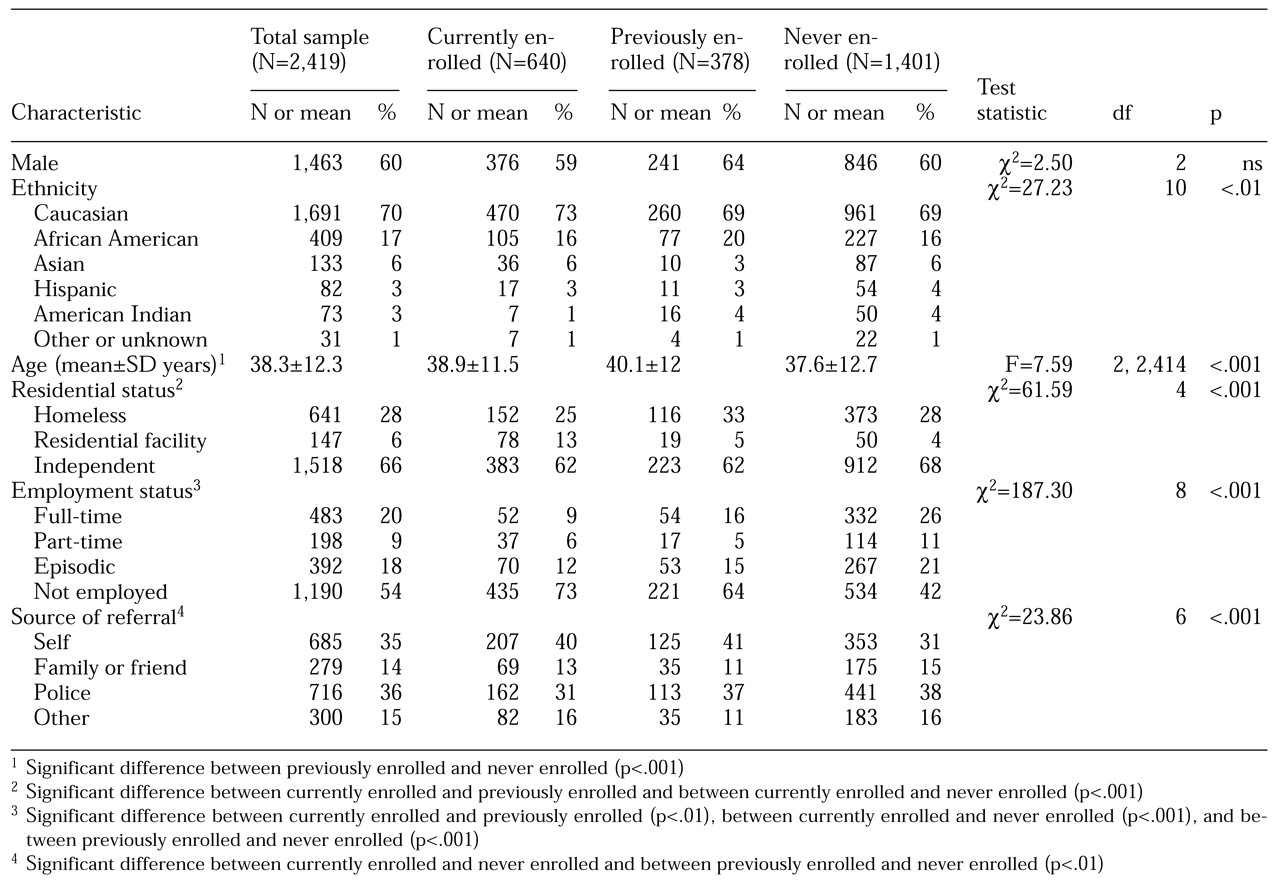
The sociodemographic characteristics of the three patient groups and the associations between characteristics and groups are summarized in
Table 1. The previously enrolled group was older on average than the never enrolled group. Because enrollment in the prepaid health plan is required for placement in residential treatment, patients in the currently enrolled group were more likely than those in the other two groups to live in a residential facility. Patients in the never-enrolled group were more likely than those in the other groups to be employed, again reflecting the requirements for enrollment in the prepaid health plan—that is, receipt of Medicaid benefits and a very low income.
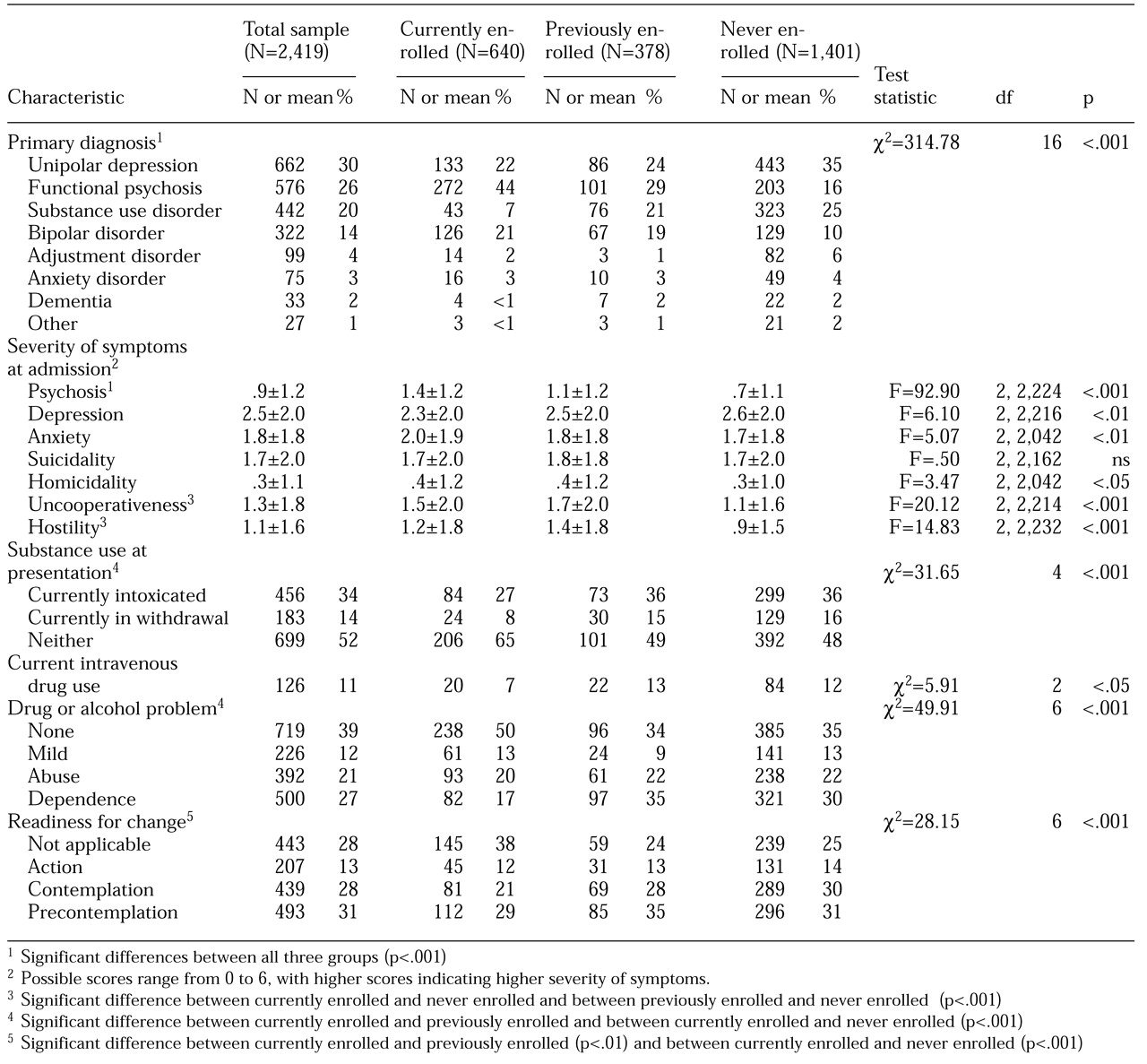
The three groups differed significantly in the proportion of patients with various primary psychiatric diagnoses (
Table 2). The currently enrolled group had the greatest proportion of patients with psychotic disorders—schizophrenia, schizoaffective disorder, or psychosis not otherwise specified—and bipolar disorders (65 percent combined) and the lowest proportion of patients with substance use disorders (7 percent). Conversely, the never-enrolled group had the greatest proportion of patients with unipolar depression and substance use disorders (60 percent combined) and the lowest proportion of patients with psychotic or bipolar disorders (26 percent combined). Patients in the previously enrolled group occupied an intermediate position, with 48 percent having psychotic and bipolar disorders and 45 percent having unipolar depression and substance use disorders.
On the basis of patients' severity of symptoms on admission and substance use (
Table 2), those in the currently enrolled group were rated as most psychotic, followed by those in the previously enrolled and never-enrolled groups. Patients in both the currently and previously enrolled groups were more uncooperative and hostile. Those in the currently enrolled group were less likely to have been intoxicated or in withdrawal on admission, less likely to have severe drug or alcohol problems, and more ready for change.
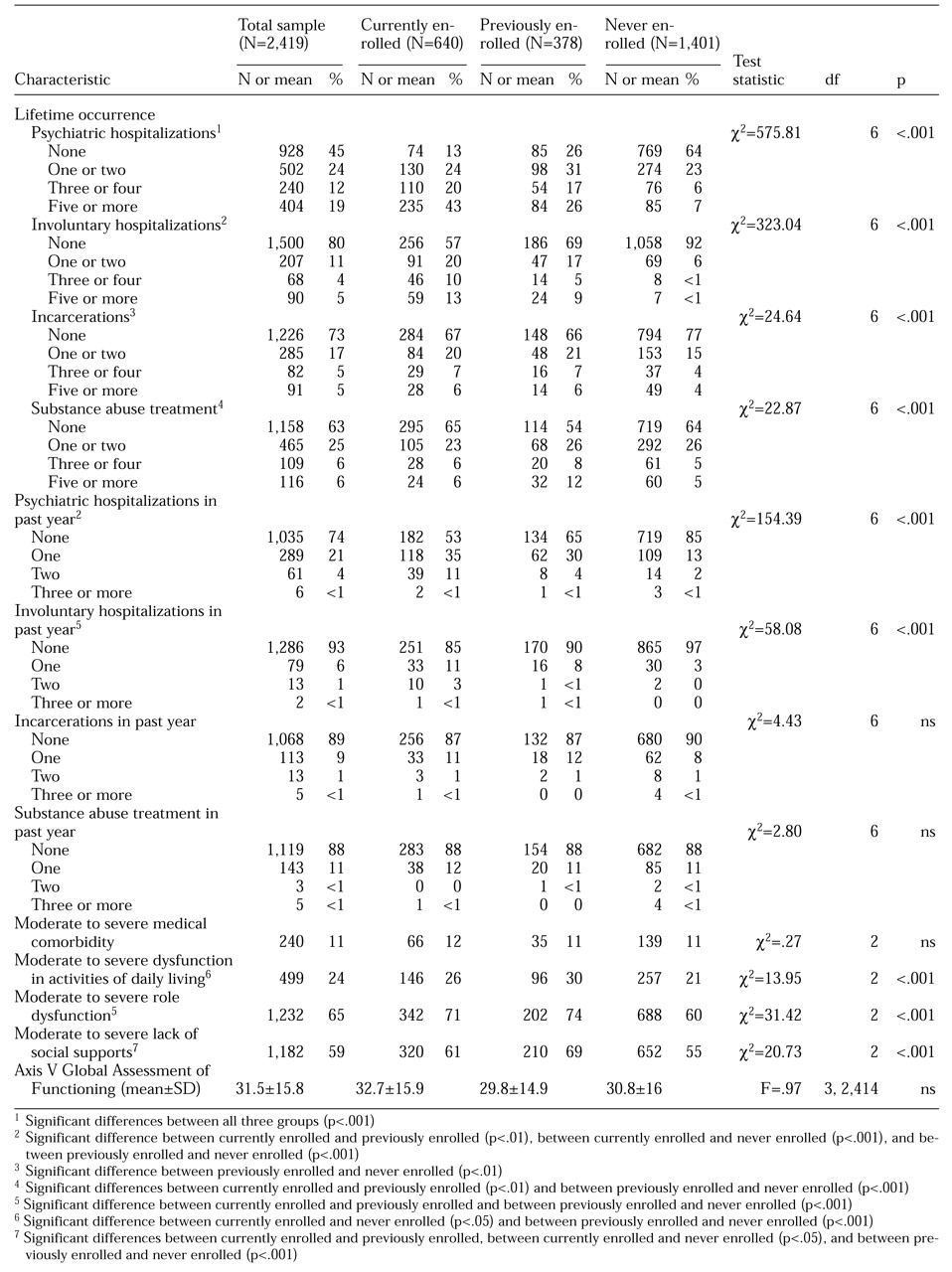
The groups also differed in number of lifetime psychiatric hospitalizations and incarcerations and in disability (
Table 3). The lifetime number of psychiatric hospitalizations and involuntary hospitalizations decreased linearly from the currently to the previously to the never-enrolled groups; for the previous year, patients in both the current and the previously enrolled groups had more inpatient psychiatric hospitalizations and involuntary hospitalizations. In contrast, the previously enrolled group had the greatest proportion of patients with three or more episodes of substance abuse treatment.
In terms of disability, patients in both the currently enrolled group and the previously enrolled group were rated as significantly more dysfunctional than those in the never-enrolled group in terms of activities of daily living, role functioning, and social supports.
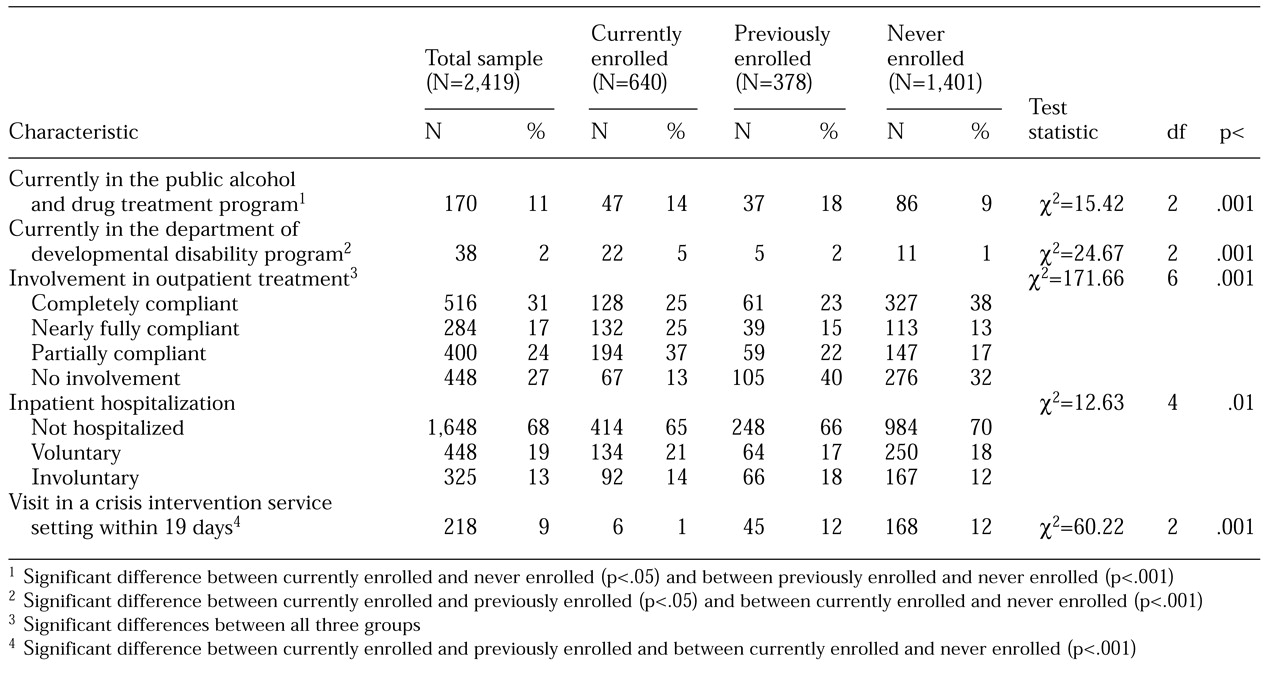
Table 4 lists the service use variables for the three groups. Patients in the never-enrolled group were less likely than those in the previously enrolled group to be enrolled in the state's public alcohol and drug treatment program. The currently enrolled group had the greatest proportion of patients participating in the state's department of developmental disability program. Patients in this group were highly unlikely to have had an appointment for outpatient crisis intervention service at a mental health center in the 19 days after their visit to the crisis triage unit, again reflecting their involvement in ongoing treatment in the regional support network plan.
Table 5 presents the results of the logistic regression analyses. The three groups differed significantly on five variables: lifetime number of psychiatric inpatient hospitalizations, type of residence, psychiatric diagnosis, lifetime number of involuntary inpatient hospitalizations, and employment status. In all three models, the odds of being enrolled in the regional support network plan increased with the number of inpatient psychiatric hospitalizations. Currently enrolled patients were more likely to live in residential facilities and less likely to be homeless. Compared with patients who had functional psychoses, patients with substance use disorders were less likely to be enrolled in the plan. The probability of being in the plan greatly increased with the number of lifetime involuntary hospitalizations. Currently enrolled patients were more likely to be unemployed. We noted with interest that the three groups did not differ significantly in the symptom severity or disability factors that were measured on presentation at the crisis triage unit.
Discussion
During the seven-month study period, only a quarter of the visits to the crisis triage unit were by patients who were currently enrolled in the regional support network plan. Indeed, on an average monthly basis, these 640 patients represented less than 1 percent of the more than 14,000 adults who were served by the county plan. These patients accounted for about 90 visits a month to the unit. They had greater levels of illness severity, as defined by diagnostic criteria (schizophrenia and bipolar disorder) and symptom severity (psychosis), and greater levels of service use, as defined by their tier level.
Because these patients would be expected to have more severe and chronic symptoms, it is probably unrealistic to expect that outpatient treatment could fully prevent periodic decompensation and the need for emergency care. However, a comparison of the characteristics of these patients with those of patients who were currently enrolled in the regional support network plan but who did not present to the crisis triage unit would be required to guide decisions about how to identify, prevent, or better manage outpatient crises and reduce the need for emergency care. The absence of data for the latter patient group is a limitation of this study.
A relatively small proportion of our sample (16 percent) had been previously enrolled in the regional support network plan. Patients in this group were found to be highly dysfunctional in multiple areas, with high rates of unemployment, involvement with the criminal justice system, substance use problems, lack of social support, and homelessness—characteristics that are often associated with treatment noncompliance and that may have caused these patients to discontinue outpatient treatment on their own. It is also possible that these patients were discharged from the regional support network plan because of loss of Medicaid funding. They may have earned higher incomes, obtained private insurance, or experienced transient improvement in their symptoms. Nonetheless, they were by no means relieved of their mental illness or their symptoms, as evidenced by their emergency presentation to the crisis triage unit.
The findings for this group of patients have implications for the planning and development of mental health treatment programs and financial mechanisms. Although the previously enrolled patients might be viewed as treatment failures, they did represent the smallest patient group in the study (16 percent), and although they demonstrated significant symptom severity and levels of dysfunction, they were less likely to have a diagnosis of a psychotic disorder, they had fewer lifetime or past-year psychiatric hospitalizations, and they were somewhat more likely to be employed than patients in the currently enrolled group. Thus, despite their high rate of homelessness and substance abuse, at least some of them were either less ill in the first place or had been at least partially stabilized. Nonetheless, many of these patients need at least episodic care, if not ongoing care, especially for symptoms and behavior that lead to social dysfunction.
King County sponsors many programs that target patients who are not enrolled in the regional support network plan (
14,
15). Other programs in the county serve mentally ill persons who are homeless, and the county also has a mental health court. However, the prominent social dysfunction, legal problems, substance use, and uncooperativeness of patients who previously have dropped out of care may prevent them from using these resources.
The largest proportion of patients in our study (58 percent) had never been enrolled in the regional support network plan. Although some of these patients may have had private insurance, their relatively low rate of full-time employment suggests that this would not have been the norm. Furthermore, many of those who were employed may represent the "working poor," who often have no insurance but because they are not eligible for Medicaid would probably not have been financially eligible for network plan services. Hence the psychiatric emergency room may have been their only treatment option.
Although never-enrolled patients were less compromised psychiatrically and less disabled than patients in the other two groups, their significant rates of substance abuse suggests that many—perhaps half—may have needed primary addiction or dual diagnosis services rather than primary mental health services. In fact, their lower rates of psychiatric hospitalization and the types of symptoms they were most likely to experience—depression, anxiety, and suicidality—indicate that many of their mental health problems may have been substance induced. Furthermore, among those with mild to moderate comorbid psychiatric illness, substance use may have impaired insight about the need for mental health treatment and reduced follow-through for the treatment opportunities that were available.
Although there has been research in the area of mental health Medicaid managed care penetration (
1,
16,
17,
18,
19,
20,
21), direct comparisons of the performance of the regional support network plan in our study and other similar programs are problematic because of organizational, regional, and methodological issues. Despite the lack of comparative data, our results indicate that the plan is succeeding in identifying high users of inpatient treatment, obtaining Medicaid coverage for them when they are eligible, enrolling them in outpatient programs, and keeping most of them—99 percent—out of emergency care, except for those with the most severe conditions. However, behavior and clinical history rather than symptom severity were the best predictors of whether a patient who presented to the crisis triage unit was currently, previously, or never involved in the regional support network plan.
Conclusions
Although the regional support network plan appeared to be doing a good job with the patients it was directed to enroll—that is, moderately to severely mentally ill individuals who qualify for Medicaid—almost three-quarters of the patients who sought emergency psychiatric services were not currently enrolled in the plan. A huge gap exists between people who are insured or can afford to pay out of pocket and people who qualify for Medicaid—primarily the working poor—and those whose symptoms are primarily substance induced and who do not qualify for Medicaid or have insurance. The latter patient group could be better served by increasing the availability of primary substance abuse services and integrated dual diagnosis service systems and by facilitating access to clinical care (
22,
23). In the meantime, emergency psychiatric services are the only available care for this group.