Optimal psychiatric rehabilitative treatment for individuals who have a dual diagnosis of severe mental illness and a substance use disorder requires implementation of an array of biopsychosocial modalities (
1). Ideally, these modalities consist of pharmacotherapy, skills training, drug treatment, case management, material incentives, money management, and family interventions. Structurally, these components should be continuous across all levels of care, integrated under the same roof, and provided by the same treatment team. It is a reality of the current health care climate that such state-of-the-art programs are likely to be found only in research settings. Yet research settings are rarely permanent. They survive only as long as they house active investigators with funding and enjoy local institutional support.
The dual diagnosis treatment program at the West Los Angeles Veterans Affairs (VA) Medical Center was launched in 1990 as a funded project aimed at comparing specialized treatment for persons with a dual diagnosis with conventional forms of treatment (
2). The project ended in 1995 but was followed by several smaller-scale studies that focused on specific program components. The project enahanced treatment at the VA center. Enhanced treatments have included supplemental staff, a token economy, an in-house representative payee, and experimental groups (
3). The program currently has no research support, and it is experiencing a rapidly growing census and unprecedented staff attrition.
The program's initial research protocol specified a definition of dual diagnosis that recognized only schizophrenia and cocaine abuse. Moreover, the outpatient component of the program was available only to individuals who were initially treated on the program's inpatient ward. In 1996 the medical center expanded admission criteria by including all types of substance use disorders and by opening the day hospital to outside referrals. Over a period of five years, the day hospital census has grown from 10 to 20 patients a day to 80 to 100 patients. Staffing consists of three four-person teams, each with a psychiatrist, a psychologist, a nurse case manager, and a psychiatric nursing assistant or licensed psychiatric technician, with additional nursing and social work staff serving the inpatient ward.
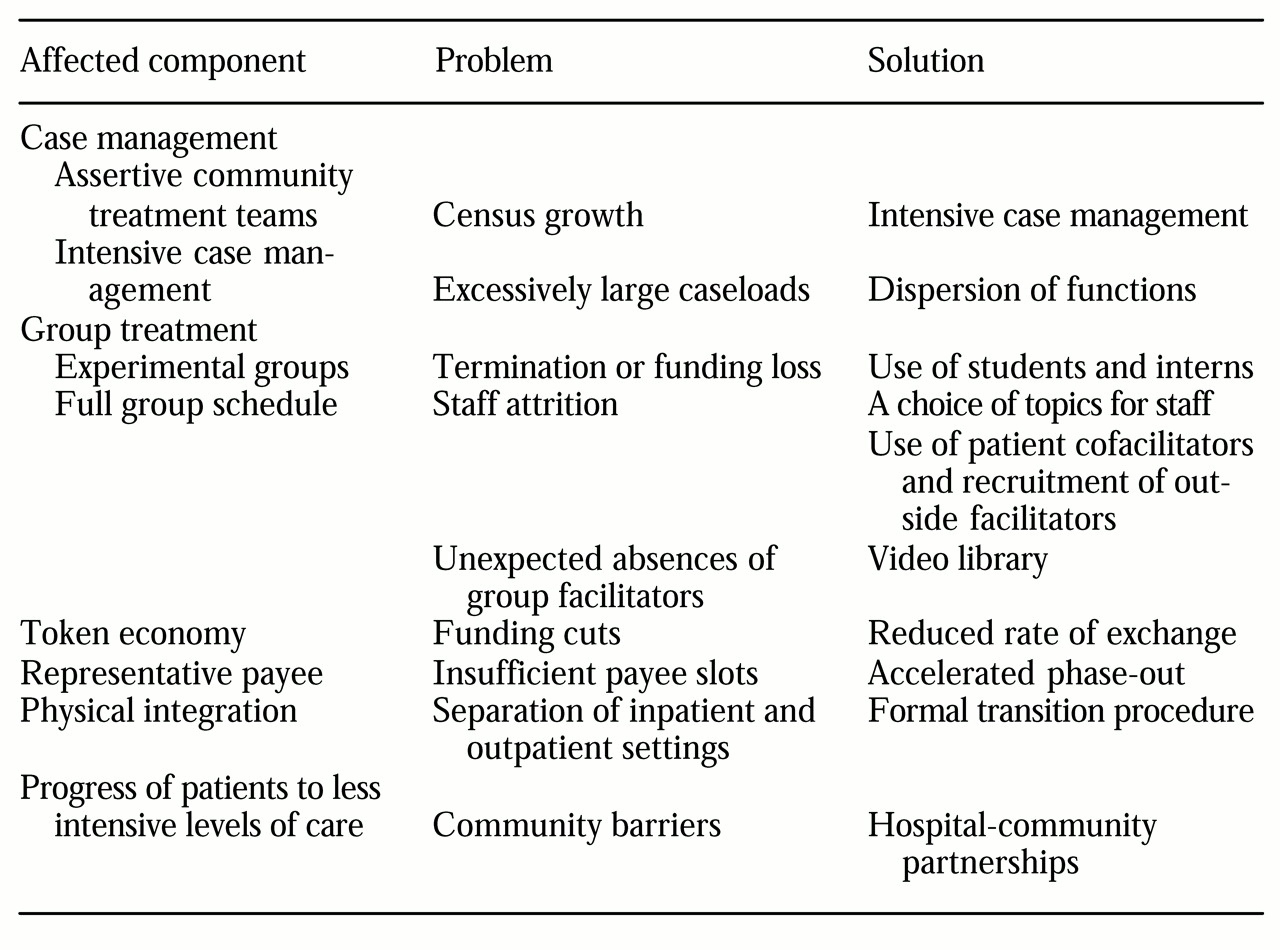
This paper describes some of the improvisations instituted by the program in an attempt to continue to provide empirically validated treatments through periods of increasing and decreasing funding and shrinking institutional support. The strategies that are discussed in this paper are outlined in
Table 1.
The dual diagnosis program
Case management
The program assigns a preeminent role to case management as the central mechanism through which discrete treatment elements are coordinated and delivered. During its first six years, the program espoused a strong version of the assertive community treatment case management model (
4). Members of each of two interdisciplinary teams jointly assumed responsibility for directly providing all necessary services to their patients. Unfortunately, with rapid census growth assertive community treatment became unfeasible, because team members could no longer all be actively involved in all aspects of every patient's case management.
Thus the program adopted a somewhat less ambitious model, commonly referred to as intensive case management (
5), in which case management functions are performed exclusively by each team's nurse case manager. This model works optimally with caseloads not exceeding 25. However, caseloads at the dual diagnosis day hospital for each of three case managers currently average between 70 and 85.
Several solutions have been implemented. First, each team's psychologist was asked to handle all aspects of particularly challenging cases. Second, routine case management duties such as tracking patients' program attendance were assigned to each team's psychiatric nursing assistant. Third, nursing responsibilities of the nurse case managers were assigned to the licensed psychiatric technician. And fourth, selected patients in the day hospital were trained as "big brothers" to be responsive to new patients' needs.
The result of these arrangements has been that each team member serves as an ex officio case manager. The program is thus able to continue to fulfill its commitment to comprehensive treatment, albeit with some trade-offs in terms of dispersion of functions.
Behavioral skills training
The core of the dual diagnosis day hospital treatment program consists of five daily groups aimed primarily at ameliorating the functional and social impairments of schizophrenia. The program uses a series of manualized skills training modules (
6) as well as a specially designed substance abuse module. It is in the area of skills training that the program has been most affected by the vicissitudes of research funding and staffing decisions.
The substance abuse management module (
7) is a good example. It was developed within the program to meet the need for a harm reduction package that would be behavioral in form and population specific in content (
8,
9). The module was initially conducted by its authors, but after two years of development it became the property of regular staff. At that time a problem arose as to how it could be incorporated into already overloaded schedules.
The answer was found in "student power." The program is blessed with a stream of psychology preinterns and interns, psychiatric interns and residents, and drug counseling trainees, who complete one- to five-month rotations. Students are typically highly motivated to learn cutting-edge treatments. A collateral benefit of using students has been the variety of styles they bring to the program. Patients who remain in the day hospital for long periods often complain about having to continually cycle through the same modules. However, complaints are not heard when the same module is successively facilitated by different individuals.
One of the program's biggest challenges is that of providing outpatients with a solid five hours of group treatment each day. With four substance abuse management module groups being double tracked, providing the desired level of treatment requires a total of 29 groups a week. Many staff members lack time or enthusiasm for groups, and others are intimidated by an average group size of 40 to 50. To make group facilitation more palatable, reluctant staff members are invited to lead groups that are based on their own interests and expertise. Allowing staff this flexibility does not dilute the quality of the program as long as core behavioral modules remain intact.
Patients provide another resource. A weekly 12-step group is facilitated by patients, and several patients who helped develop groups cofacilitate them with staff. An additional resource is provided by external facilitators, for whom recruitment is ongoing. Groups are currently being offered by a chaplain, a pharmacist, and a VA-affiliated representative payee.
Of all group scheduling problems, the most immediate and perennial is that of the group for which the assigned facilitator is unexpectedly absent and no coverage has been arranged. The antidote is a video library consisting of patient education videos and television programs recorded by staff. Among the latter are excellent Public Broadcasting Service and cable programs on mental health topics as well as dramatic presentations relevant to patients' concerns.
Incentive system
An incentive system was built into the treatment program's initial protocol. The system works by awarding points to patients for engaging in designated program activities. Points are redeemable for $1 VA canteen books. Two years ago, protected funds for the incentive system were cut by one-third. The program could adapt only by instituting yet another increase in the point-canteen book rate of exchange and placing a still lower ceiling on the number of canteen books it allows outpatients to redeem daily. However, to the constant amazement of staff members, the value of the point as a motivator seems never to diminish. These observations suggest that even symbolic token economies can be effective.
Money management
The dual diagnosis treatment program was established after a treatment outcome study found a strong association between first-of-the-month receipt of disability payments and psychiatric symptoms and hospital admission (
10). This finding prompted the solicitation and granting of VA funds for an in-house representative payee to manage the income of patients who are prone to spending their disability checks on drugs. However, the number of contractually provided payee slots is inadequate to meet the program's needs. To reduce a growing waiting list, the program has implemented a procedure whereby clients who have achieved a requisite amount of sobriety and psychiatric stability are started on a six-month phase-out during which mediated payment occurs only for basic living expenses. Although some patients may be phased out prematurely, most reach a point at which they have begun to experience the intrinsic rewards of managing their income adaptively. Attendance is assured during the phase-out because the program remains the locus of money disbursement.
Continuity of care
The most recent threat to the program's integrity has come from the physical separation of its inpatient and outpatient components. Even when the inpatient ward and the day hospital were housed together, day hospital retention rates were lower for patients making a transition from the inpatient ward than for community referrals. This difference is presumably related to the fact that patients referred from the inpatient ward are not completely stabilized because of shortened hospital stays.
To minimize the effects of the separation, the program has bolstered and elaborated a transition process that was already in place. This process has several steps. First, the day hospital is described to inpatients when they are admitted to the hospital, and toward the end of their stay they attend a spirited transition group that promotes its benefits. Second, day hospital case managers are present at their respective teams' inpatient rounds at least once while prospective transferees are being reviewed. Third, inpatients start attending the day hospital several days before being discharged and are transported on the first day by their case manager. Fourth, each transitioned inpatient is assigned a day hospital big brother who is capable of selling the program and addressing the patient's discontents. Finally, close case management is provided during the first several weeks of day hospital attendance. The deliberateness of this process may serve not only to maintain the flow of inpatients to the day hospital and preserve their retention at previous levels but also to actually improve these program aspects.
Another vexing problem is the relationship between continuity and intensity of care. Ideally, patients proceed from inpatient status, which lasts seven to 14 days, to the day hospital, which requires a minimum of one visit a week, to formal outpatient status, which consists of a minimum of one visit every one or two months. This sequence is based on the assumption that patients require less intensive services over time. Unfortunately, few patients in the dual diagnosis treatment program reach outpatient status. This outcome is largely attributable to a lack of drug-free neighborhoods and rehabilitative resources in the surrounding community. Thus the day hospital continually receives and provides new services to patients at a higher rate than that at which it is able to decrease services to those already in the program. One solution is an effort by the medical center to partner with existing community enterprises to provide treatment-compatible environments outside the hospital.
Conclusions
Despite situational shortfalls, a treatment philosophy can be preserved and effectuated through innovation, trial and error, and a constant willingness to adapt. It is hoped that some of the adaptations forged by the dual diagnosis treatment program described here will, by virtue of either their process or their content, be of use to other dual diagnosis programs in which goals too often seem to exceed available resources.