Clients with a dual diagnosis often encounter confusion and uncertainty among health care providers about what system should provide their care—the mental health system or the substance abuse treatment system. Many clients with dual disorders are not compliant with treatment, and they experience repeated relapses, rehospitalizations, and homelessness. The costs of their care are often significantly higher than for clients with a single disorder.
We examined services received by Medicaid beneficiaries with dual disorders and the costs of these services. Using adjudicated Medicaid claims for services provided to residents of Monroe County, New York, during calendar year 1998, we first identified the subset of 2,276 Medicaid beneficiaries who received both mental health and substance abuse services. Beneficiaries who had a psychiatric or substance-related diagnosis were excluded if they received services only in a primary care setting and did not use specialty mental health or substance abuse services.
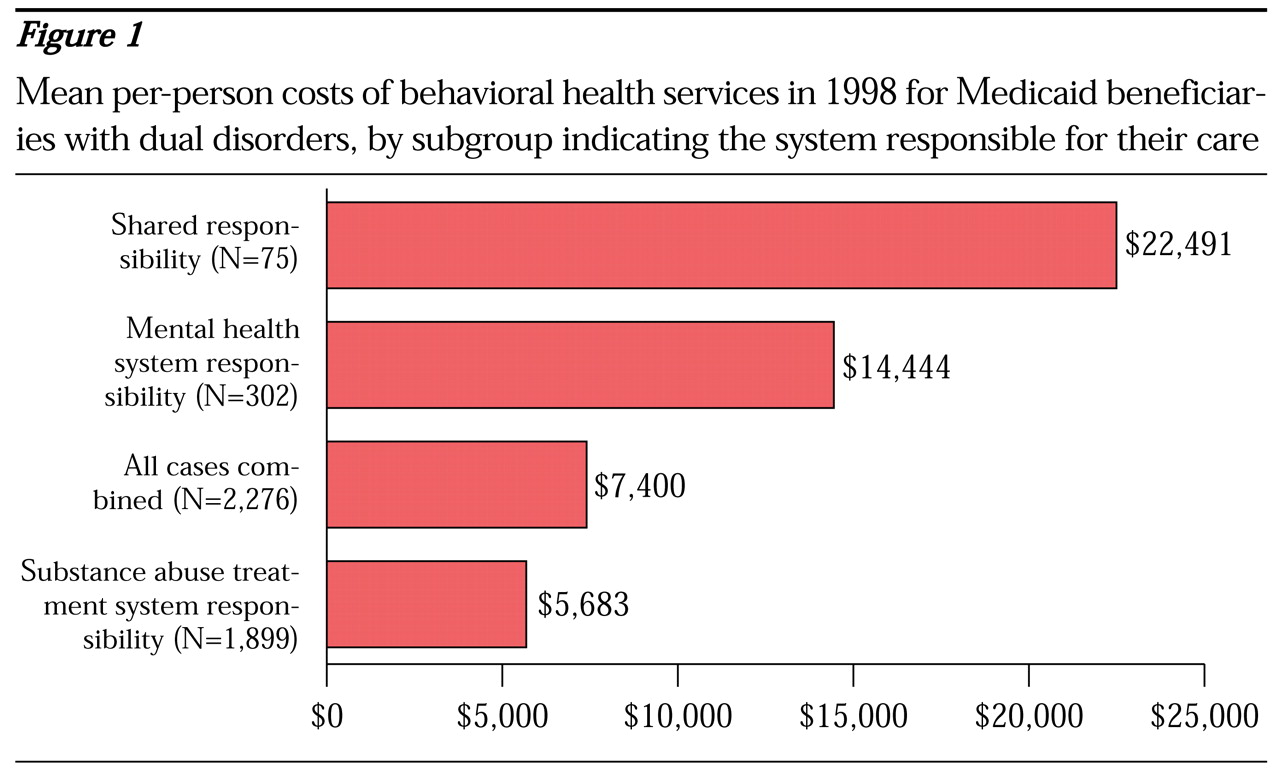
The 2,276 beneficiaries were categorized into three groups, depending on the system that was primarily responsible for their care. The mental health system was deemed responsible if a beneficiary used any mental health specialty service, including continuing day treatment, intensive or supportive case management, and intensive psychiatric rehabilitation training. Beneficiaries who could not be included in the first group and who had two or more inpatient mental health admissions and at least one admission for inpatient substance abuse treatment were in the shared-responsibility group, because the mental health system and the substance abuse treatment system shared responsibility for their care. The third group comprised beneficiaries for whom the substance abuse treatment system was deemed responsible; they did not meet the criteria for assignment to either the mental health or the shared-responsibility group. We predicted that the costs of care for beneficiaries in the shared-responsibility group would be higher than the costs of care for beneficiaries in the other two groups.
Figure 1 illustrates the substantial cost differences among the three groups. The results confirm our hypothesis about the higher costs of care for the Medicaid beneficiaries in the shared-responsibility group. Costs were lower for beneficiaries with dual disorders who received their care from a single service delivery system than for those who received services from both systems.
More detailed analyses are required to better ascertain actual patterns of care and to understand differences in service use between the groups. Also, it is impossible to know whether the higher costs for the shared-responsibility group were appropriate to the level of care needed or represented extra expenditures for disjointed care.
However, even at this aggregate level, the data suggest the need to review potential opportunities to improve the efficiency and coordination of services provided to Medicaid beneficiaries who receive services from both systems of care.