In 1992 the Commonwealth of Massachusetts introduced managed care in an effort to control the use and costs of Medicaid-reimbursed mental health and substance abuse services. A substantial body of research has examined the extent to which these goals have been realized (
1,
2,
3). These studies have shown that managed care was associated with a reduction in the use of inpatient services reimbursed by Medicaid. However, policy interventions are known to have effects beyond those intended, and the extent of such effects in Massachusetts has yet to be examined.
In this article we address the question of whether there were unintended—but theoretically predictable—consequences of the introduction of managed care in Massachusetts. Specifically, we ask whether shifting the care of a substantial number of adults with severe mental illness to a Medicaid managed care plan might have elevated their risk of being admitted to the inpatient forensic mental health system operated by the Massachusetts Department of Mental Health.
Methods
Analytic approach
To address the question of whether restrictions on inpatient treatment under managed care have led to greater use of the mental health department's inpatient forensic services, we posited and tested two hypotheses. The first hypothesis was that Medicaid beneficiaries with psychiatric disabilities had a greater risk of forensic admission than nonbeneficiaries after the introduction of managed care because of a reduction in their use of acute inpatient treatment. The second hypothesis was that police and judges, having observed these limitations on hospitalization, would use criminal justice and backdoor commitment strategies more often after the introduction of managed care in the case of persons with severe mental illness, regardless of their insurance status. Under this scenario, the risk of being hospitalized under criminal authority would increase after the implementation of managed care, but any such increase would not be specific to Medicaid beneficiaries.
Data
Data from the Massachusetts Department of Mental Health were used to test the two hypotheses. An individual's status as a recipient of residential or case management services was determined by whether he or she was included in the registries maintained by the department for these types of programs. Medicaid beneficiaries were identified by indicators of Medicaid enrollment. A forensic admission was defined as admission to a state hospital under any of the legal mechanisms outlined above.
Sample
The study sample comprised persons with severe and persistent mental illness between the ages of 18 and 64 years who had received services from the Massachusetts Department of Mental Health in fiscal year 1992, the year before managed care took effect, and in fiscal year 1994, one year after the effective date of managed care. Note that in Massachusetts the fiscal year extends from July 1 of the previous calendar year to June 30 of the next year. For example, fiscal year 2002 began on July 1, 2001, and will end on June 30, 2002. With an inception date of October 1, 1992, Medicaid managed mental health care is defined as having begun in fiscal year 1993.
Individuals were included in the study cohort if they had received one or more of three types of services from the mental health department in both fiscal year 1992 and fiscal year 1994: at least one episode of nonforensic inpatient treatment in a departmental facility, department-funded residential services, or departmental case management. A total of 7,966 persons met these criteria.
Model development and variable construction
A multivariate model was developed to test the two hypotheses. This model was used to assess the relationship between forensic hospitalization and Medicaid beneficiary status in each year. Because of potential differences in the risk of involvement with the criminal justice or forensic systems between Medicaid beneficiaries and nonbeneficiaries, several covariates were included in the model to adjust for key demographic variables and factors related to service recipient status. Demographic covariates included sex, age, and race, all of which are known to be risk factors for involvement with the forensic system (
26). The receipt of case management and residential services was seen as potentially protective against forensic system involvement (
26), and these factors also were included as covariates.
The effects of sex, age, and race were assumed to be constant over time—that is, time invariant. Age was measured in fiscal year 1992, centered at 41 years—the mean of the age distribution—and parameterized by both a linear and a quadratic component. The quadratic component was included because it was assumed that the effect of age on the risk of forensic involvement was not linear across the full age distribution. Race was recorded as white or other.
The diagnostic measures available in these data were found to be inconsistent or missing in several cases and thus were excluded from the analysis. We made this decision with the knowledge that all the individuals in the cohort had met the mental health department's criteria for receiving services in two separate fiscal years and thus had had a diagnosis of severe and persistent mental illness throughout that study period. It was assumed that receipt of case management and residential services, as well as Medicaid beneficiary status, were subject to change between fiscal years—that is, time dependent. Each person's status on these factors—measured as a "yes" or "no" binary variable—was thus measured for each fiscal year. Data on changes in status during each fiscal year were not available.
In addition, we were unable to determine the insurance status of nonbeneficiaries, although previous experience with this population and consultation with knowledgeable officials of the department of mental health suggested that many of these persons probably had Medicare coverage—not managed—as their primary form of insurance. Although some Medicare beneficiaries also receive Medicaid benefits, this population was not included in the managed care plan. Other nonbeneficiaries are uninsured and receive all services from the department. A very small number have some form of private insurance. None of the nonbeneficiaries were subject to managed care practices of the kind introduced by Medicaid.
Statistical methods
The simplest approach to testing our hypotheses would probably have been to conduct two analyses of Medicaid beneficiaries' and nonbeneficiaries' likelihood of forensic admission, one for the pre-managed care period and another for the post-managed care period, and then compare the effects of beneficiary status across the two models. However, this approach would have presented two major problems.
First, in comparing the effects estimated by the two models—for example, the log-odds of forensic commitment—the precision of the effects would have been overstated because of nonindependence in the observations. Thus we needed to use a method that could account for correlations in the data across periods. Second, both system-level data and data from our cohort showed a negative trend in forensic hospitalization rates between fiscal year 1992 and fiscal year 1994, an extension of a trend that began in the mid-1980s. To isolate and identify the effects of managed care, we needed to control for this trend.
An approach well suited for this task is logistic regression incorporating an occasion-specific effect (
27) estimated with generalized estimating equations (GEEs). GEEs are an extension of generalized linear models that allow the inclusion of correlated observations. This approach separately relates the average response to explanatory variables and specifies the variance, as in a generalized linear model. However, unlike a generalized linear model, in which the likelihood is maximized by solving estimating equations, the complete distribution of the response is not needed, so a "quasi" likelihood is maximized by solving generalized estimating equations.
In our study, GEEs fit a single model of forensic hospitalization, incorporating variables for the main effects of Medicaid beneficiary status and fiscal year, respectively, as well as a term to capture the interaction of Medicaid beneficiary status and post-managed care period. The analysis was based on 15,932 observations—that is, one per fiscal year for each case.
Results
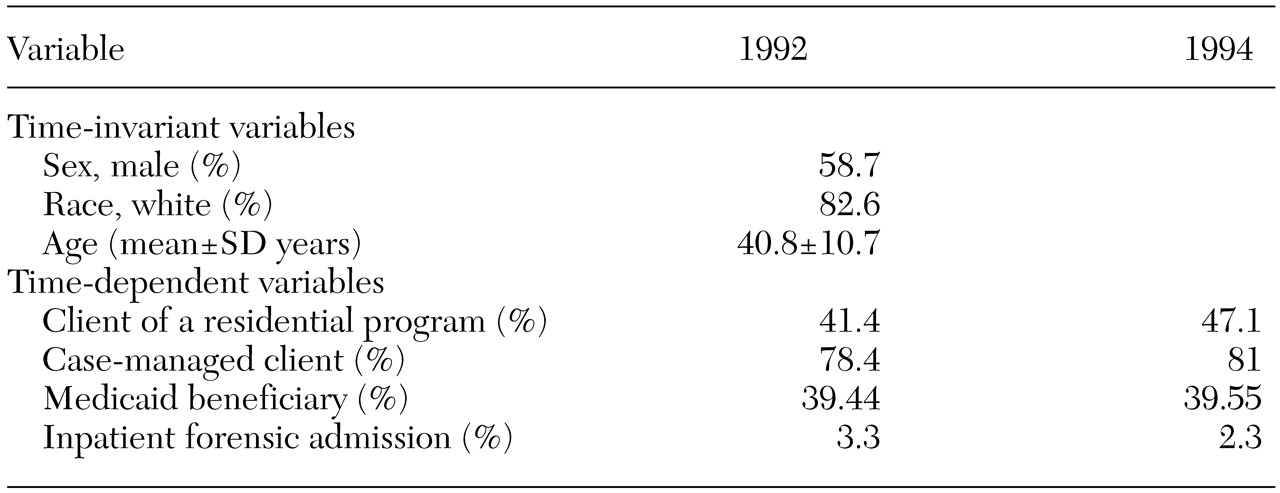
Table 1 summarizes the demographic and service use characteristics of the sample. The study cohort was predominantly male and white. Changes in service use were noted between the two fiscal years. In the post-managed care period the cohort used more case management and residential services. The proportions of Medicaid beneficiaries were nearly identical in each period. Sixty-nine percent of fiscal year 1994 Medicaid beneficiaries were enrolled in both years; 31.7 percent of fiscal year 1992 Medicaid beneficiaries were not enrolled in fiscal year 1994, and 18.8 percent of fiscal year 1992 nonbeneficiaries were enrolled in fiscal year 1994.
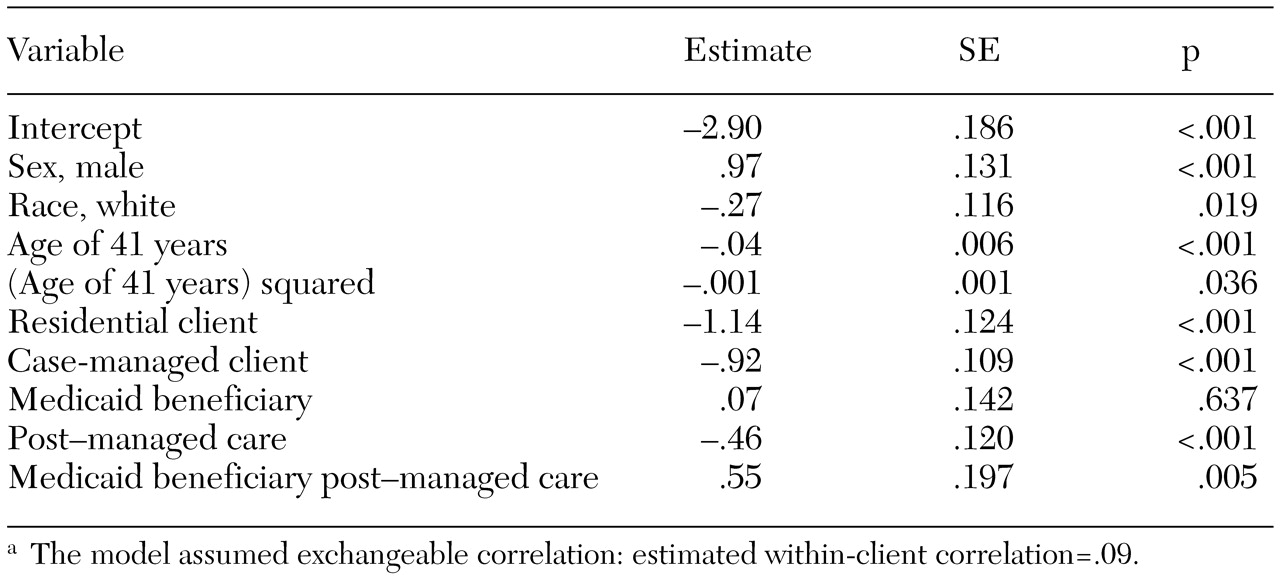
The results of the GEE model are shown in
Table 2. The interaction term was significant and positive, indicating that Medicaid beneficiaries had a significantly higher risk of forensic hospitalization than nonbeneficiaries in the post-managed care period (odds ratio=1.85, 95 percent confidence interval=1.37 to 2.50). Thus our first hypothesis was supported. However, our second hypothesis—that there would be a generalized increase in the risk of forensic hospitalization among persons with mental illness—was not supported. The declining rate of forensic admissions observed in our sample (
Table 1) and the significant negative main effect for the post-managed care period in our GEE model strongly contradicted this hypothesis. For non-Medicaid beneficiaries, the likelihood of a forensic commitment was significantly higher in fiscal year 1992 than in fiscal year 1994 (odds ratio=1.58, CI=1.25 to 2.00), whereas no significant difference was observed among Medicaid beneficiaries (odds ratio=.91, CI=.67 to 1.23).
Among the covariates in the model, being male and being white were positive predictors of forensic hospitalization, whereas being older, being involved in a residential program, and receiving case management services each appeared to protect against forensic hospitalization.
Discussion and conclusions
We examined two theoretically and historically based hypotheses on the possible effects of Medicaid managed mental health care on the use of a state's inpatient forensic system. Our data strongly supported the hypothesis that Medicaid beneficiaries would have a greater risk than nonbeneficiaries of forensic commitment after the introduction of managed care.
Medicaid beneficiaries' risk of forensic hospitalization remained essentially constant throughout the study period, whereas the risk for nonbeneficiaries declined significantly. These findings have implications for the social control framework from which our hypotheses were derived, for the forensic components of public mental health agencies, and for the persons for whom the risk of forensic hospitalization was greater after the introduction of managed care.
As we have noted, several studies have provided empirical support for the hydraulic model of social control. Our findings also lend credence to that model and provide a case for its consideration in future analyses of changes within the social control system. Moreover, our results are consistent with those of studies showing that the use of forensic hospitalization is particularly sensitive to changes in other sectors of the mental health system. However, the processes underlying this shift clearly need additional quantitative and qualitative study if they are to make a real contribution to this theoretical model.
Our findings also have implications for the forensic sectors of public mental health systems. Aggregate data made available to us by the Massachusetts Department of Mental Health indicate that, despite an occasional upward spike, inpatient forensic hospitalizations have declined since the statewide implementation of court clinics in the mid-1980s. The data presented here indicate that this decline has, in general, continued since the introduction of Medicaid managed care, but not among Medicaid beneficiaries. One could therefore argue that managed care has imposed opportunity costs on the forensic system by impeding the system's efforts to further reduce the use of inpatient services.
The results of this study also have direct fiscal implications for forensic systems and for the criminal justice systems that refer individuals to inpatient forensic services. If it is the case, as our data suggest, that the likelihood of involvement with the courts did not decline among Medicaid beneficiaries as it did among similar persons with severe mental illness, then these agencies also are likely to have incurred unnecessary costs. Determining just how substantial these costs were would require rigorous economic analysis. Nevertheless, such research would contribute to a more complete accounting of managed mental health care's net costs and savings across a broad spectrum of public agencies.
Finally, but perhaps most significantly, our findings have implications for the consumers of mental health services for whom the risk of forensic admission remained constant while that for other consumers declined. Individuals detained in the criminal justice and forensic systems who might not otherwise have been so detained arguably were subjected to more coercive system interventions than necessary, an outcome clearly not envisioned by the designers of the plan. Again, further study would be needed to determine whether this was the case and, if so, how any coercive interventions were manifested.
The statistically significant relationships we observed suggest that managed care has generated potentially important secondary effects. However, they provide no insight into the mechanisms behind those effects. Future research should be based on both qualitative observation and quantitative data gathered prospectively for extended periods to show how individuals are channeled into one system or another and how changes in any of the components of those systems affect that process. Such inquiries should go even further to assess the outcomes of forensic evaluations and the ultimate dispositions of any subsequent criminal proceedings. Data derived from such research would assist policy makers in weighing potential individual and systemic costs and consequences in the design of system interventions.