Results
Of the 156 administrators surveyed, the response rate was 60 percent (N=94).
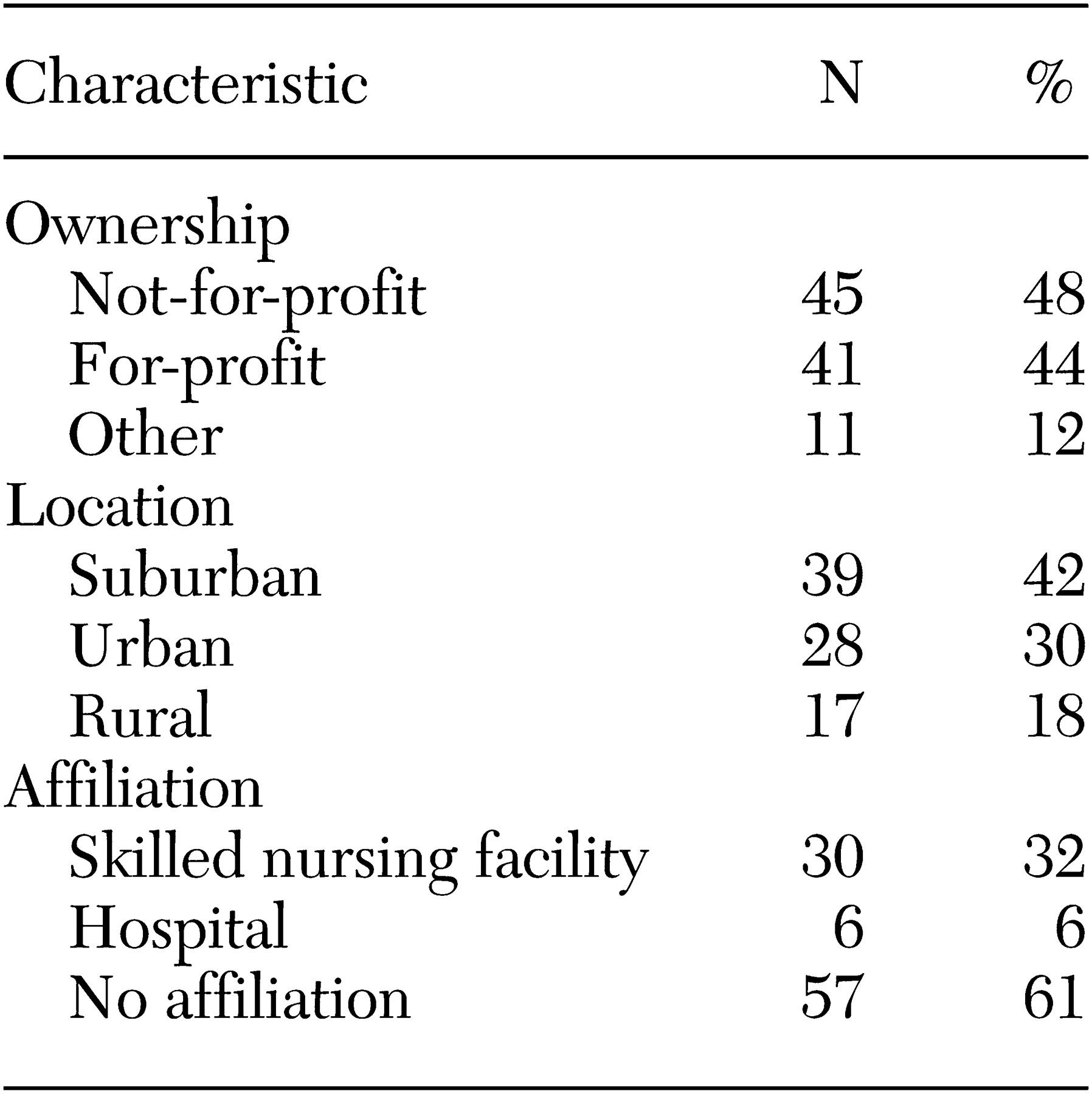
Table 1 describes key characteristics of the facilities, including ownership, location, and affiliations, as reported by each survey respondent.
Thirty-six facilities (38 percent) had a dementia unit. Sixty-six administrators (70 percent) reported a daytime staffing ratio of less than one staff member for ten residents. With respect to nighttime personnel, 67 administrators (71 percent) reported staffing ratios of less than 1:10.
In assessing mental illness, 62 administrators (66 percent) reported that they performed some type of mental health evaluation when residents were admitted into the assisted living facility. Thirteen facilities (14 percent) noted that mental health was evaluated only at admission, nine (10 percent) had monthly evaluations, 26 (28 percent) had quarterly evaluations, and 24 (26 percent) had yearly evaluations. In addition to their scheduled evaluations, 63 facilities (67 percent) had evaluations "as needed."
Forty-five administrators (48 percent) estimated that nearly half of all assisted living residents were cognitively impaired. Administrators also ranked the three most common types of mental illness encountered among their residents. The most commonly reported illness was dementia (reported by 56 administrators, or 60 percent), followed by depression (24 administrators, or 26 percent), hallucinations or delusions (four administrators, or 4 percent), anxiety (three administrators, or 3 percent), and alcohol use (one administrator, or 1 percent). Likewise, administrators ranked the three most problematic behaviors they had experienced with residents; patients' resistance to care was found to be the most common problematic behavior (39 respondents, or 42 percent), followed by wandering (24 respondents, or 26 percent), verbal abuse (eight respondents, or 9 percent), screaming (three respondents, or 3 percent), paranoia (three respondents, or 3 percent), sexually inappropriate behaviors (two respondents, or 2 percent), and physical abuse (two respondents, or 2 percent).
Administrators ranked primary care physicians as the most common type of provider of mental health services in assisted living facilities (56 administrators, or 60 percent). Psychiatrists were ranked second (45 administrators, or 48 percent), followed by community mental health agencies (40 administrators, or 43 percent), private therapists (27 administrators, or 29 percent), and friends (five administrators, or 5 percent).
To explore the types of mental health resources available in the community, we listed various therapy options—including family, individual, and group therapy as well as spiritual counseling, medications, and electroconvulsive therapy—and asked administrators what types of therapy options were available to their residents. Unfortunately, we did not inquire about how many residents actually needed or used each service. Given this limitation, we were not able to calculate which types of therapy were underused.
To understand the discrepancy between treatments available and treatments used, we inquired about barriers that may prevent a resident from receiving mental health care. Resident refusal ranked as the most common treatment obstacle (62 respondents, or 66 percent), followed by family refusal (52 respondents, or 55 percent). Cost (23 respondents, or 25 percent) and stigma of mental illness (25 respondents, or 27 percent) were ranked higher than lack of transportation (16 respondents, or 17 percent), unavailability of treatment (13 respondents, or 14 percent), or confidentiality concerns (three respondents, or 3 percent).
Mental illness may be a barrier to admission or a reason for discharge within the long-term-care continuum. A total of 75 facilities (80 percent) had a written discharge policy; 16 facilities (17 percent) did not, and two administrators (2 percent) did not know whether a policy existed. Physical abuse ranked as the most likely reason for denial of admission (71 administrators, or 76 percent), followed by sexually inappropriate behaviors (48 administrators, or 51 percent), screaming (44 administrators, or 47 percent), wandering (40 administrators, or 43 percent), verbal abuse (32 administrators, or 34 percent), paranoia (19 administrators, or 20 percent), and resistance to care (16 administrators, or 17 percent). Every administrator endorsed at least one behavior.
The reasons for premature discharge parallel those related to the denial of admission. Physical abuse again received the highest ranking (73 respondents, or 78 percent), followed by sexually inappropriate behavior (55 respondents, or 59 percent), screaming (44 respondents, or 47 percent), wandering (40 respondents, or 43 percent), verbal abuse (39 respondents, or 42 percent), resistance to care (23 respondents, or 25 percent), and paranoia (19 respondents, or 20 percent). Verbal abuse and the patient's resistance to care were more likely to be reported as reasons for denial of admission than as reasons for discharge.
Discussion
The results of this survey suggest that mental illness is an issue in assisted living facilities. More than 60 percent of the 94 administrators viewed dementia as problematic and 26 percent endorsed depression as an issue, which suggests that there may be a significant need for mental health services in assisted living facilities. It is not surprising that mental health services are needed in these facilities, because similar results have been seen in nursing homes (
3). However, unlike in nursing homes, mental illness in the assisted living facility setting is largely unstudied (
5).
Our results imply that of the treatments available, medications and supportive therapies are the most likely treatments to be endorsed by administrators. However, because we did not survey administrators about how many residents actually needed or used each service, we were not able to calculate which types of therapy were underused.
From this study, it appears that the largest barrier to obtaining services may be related to the attitudes of patients and families themselves. The stigma of mental illness, lack of understanding of the etiology of mental illness, or previous negative experiences may fuel these attitudes.
Although each of the facilities in this study was licensed in the state of Michigan, policies and procedures varied among institutions. Twenty percent of all facilities did not have a written discharge policy. Not surprisingly, physical violence and aggression were the likely reasons for admission refusal and for discharge.
Our research has limitations. For example, only licensed assisted living facilities were surveyed. Also, although administrators were asked about mental health service access and use, we did not include definitions of each service provided. In addition, we do not know whether services were actually needed. These questions suggest that further research on mental health is needed in this arena.