Public health initiatives that target depression have typically emphasized secondary and tertiary prevention, such as encouraging appropriate treatment seeking and educating health professionals about recognition and management. Primary preventive strategies have been explored to a lesser extent. Munoz and colleagues (
1) evaluated the impact of disseminating cognitive and behavioral strategies through a television miniseries. They observed a reduction in depression ratings, but only for participants who had elevated symptom ratings at baseline. A subsequent study evaluated the impact of a classroom-based cognitive-behavioral depression prevention "course" among primary care patients (
2). A significant reduction in Beck Depression Inventory ratings was observed, and the reduction was greatest among participants who had elevated ratings at baseline.
The impact of a preventive program is related to both its efficacy and its ability to reach target populations. Technologies such as interactive voice telephony and the Web offer an opportunity to reach large populations at minimal cost. The Web, in particular, can offer a visually attractive and highly interactive user interface. Interactive voice telephony removes the need for Internet access, potentially enhancing access even further. Information about depression is already widely available through the Internet. This study compared the impact of a computer program specifically designed to prevent depressive symptoms with the impact of a program that had a similar appearance but that provided only general information about depression.
Methods
Data collection took place between February 2000 and October 2001. The preventive intervention developed for this project was an interactive computer program accessible through the Web or by interactive voice telephony. The program included four content modules. The first module covered cognitive restructuring techniques, including didactic elements and a series of interactive scenarios. These scenarios were modeled after those described by Panages (
3). The second module focused on activity levels and also included both didactic and interactive components. This section was modeled after the preventive intervention developed by Munoz and Ying (
4). Another section focused on sleep hygiene and stimulus control, using a set of techniques and guidelines adapted from those of Morin (
5). A quiz with personalized feedback was built into this module to improve interactivity. The final module focused on alcohol consumption, adopting as templates documents from the National Institute on Alcohol Abuse and Alcoholism. A control program was also developed with the same number of modules and similar interactive elements, but its content was restricted to general information about depression. A pilot study (N=50) preceded the trial to enable us to identify bugs and to improve flow and wording.
The study was conducted in Calgary, which is located in the western Canadian province of Alberta near the eastern slopes of the Rocky Mountains and has almost one million inhabitants. Participants were recruited into the study through postings, announcements, and advertisements in local media. The postings emphasized the preventive nature of the study, using the slogan "Help us to find an effective prevention." No incentives were offered to volunteers, except that all were offered unlimited access to the telephony and Web sites after completion of the study. Volunteers provided informed consent and were then screened for current major depression by using the Composite International Diagnostic Interview (CIDI) (
6). Loss to follow-up was minimized by obtaining multiple contact sources for each participant at baseline. Eligible participants were assigned to either an active group or a control group by coin toss. Both interviewers and participants were blinded to study group.
Each participant was contacted by telephone once a month for three months. The follow-up interview incorporated the Center for Epidemiological Studies Depression rating scale (CES-D) and sets of questions designed to evaluate the intermediary variables: cognitive style, activity, sleep quality, and alcohol consumption. Two measures of cognitive style—self-esteem and mastery—were selected from a Canadian national population health survey. Subsets of items from the Pleasant Activities Schedule (
7) and the Social Activities Questionnaire (
8) were also included. Two sets of ratings relevant to sleep quality were obtained (
9). A seven-day diary of alcohol consumption based on standard equivalency units was also elicited. After the third and final data collection interview, each participant was interviewed by using a short form of the CIDI in order to detect recent episodes meeting
DSM-IV criteria for major depression.
The primary analysis involved comparisons of the proportions of participants with CES-D scores exceeding the threshold of 15 at each time point on the basis of Fisher's exact test and evaluating the probability of remaining nondepressed during follow-up on the basis of Kaplan-Meier life tables and associated log-rank chi square tests. The Kruskal-Wallis test (equivalent to the Mann-Whitney U test when there are two groups) was used to compare median CES-D ratings.
Results
A total of 786 participants were included in the study, 78 men (9.9 percent) and 708 women (90.1 percent). The mean age of the participants was 45.2±11.9 years. Compared with the Canadian national population, volunteers for the preventive trial were more likely to be women and more likely to report having both work and child care responsibilities. The median number of years of formal education was 15. The mean duration of interaction with the program was 50 minutes. However, some participants reported that they saved or printed pages for off-line review, so this estimate is probably conservative. The baseline CIDI interview indicated that 267 participants (34 percent) had previously experienced episodes of major depression. Of the 786 participants enrolled in the study, 764 (97.2 percent) were successfully followed up for the three months. Among the participants who were willing to guess their study group assignment, 349 of 610 (57.2 percent) guessed correctly.
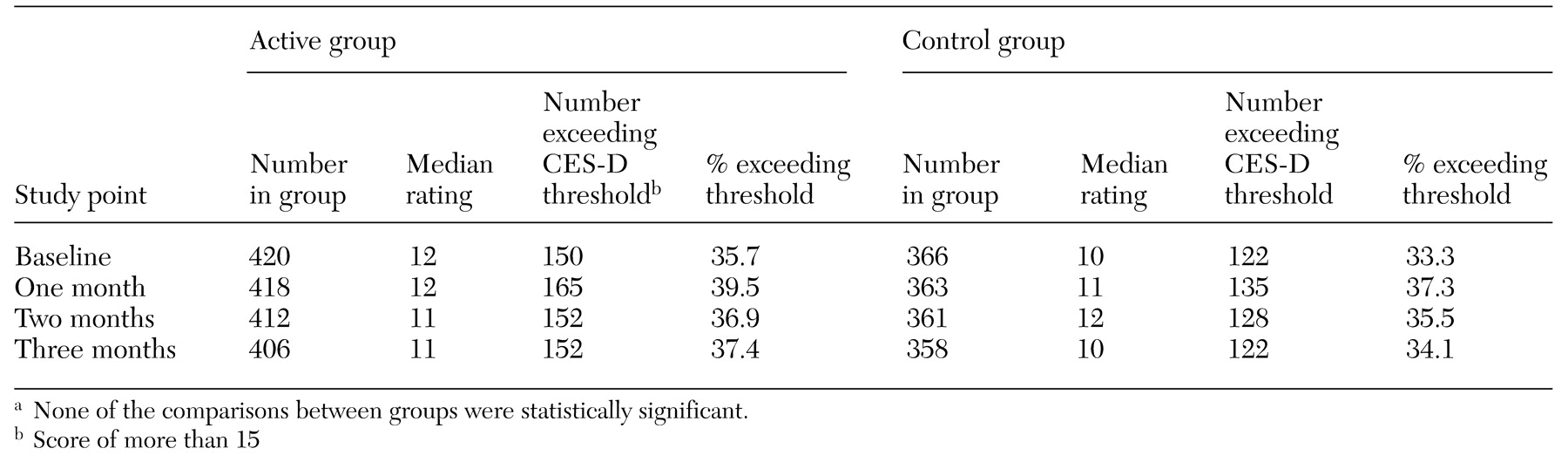
Comparisons between treatment groups are presented in
Table 1. Scores did not show a tendency to diminish over time, and there was no evidence of differences between the two groups at any time point. A rating on the short form of the CIDI was provided by 756 participants at their final interview: 51 (12.7 percent) of 401 participants in the active treatment group had an episode of major depression, compared with 45 (12.7 percent) of 355 in the control group. The three-month incidence of major depression in both study groups substantially exceeds the 12-month incidence of major depressive episode in the general Canadian population, which suggests that despite the study's inclusion of persons with active major depression, those who volunteered to participate in the study constituted a high-risk group.
No association was found between treatment and the proportion of participants who reported heavy drinking. At baseline, 17 (4 percent) of 420 participants in the active treatment group and 18 (4.9 percent) of 366 participants in the control group consumed more than two drinks per day. After three months of follow-up, the proportions were nearly identical: 16 (3.9 percent) of 406 and 18 (5 percent) of 358, respectively. Neither heavy drinking nor any drinking was significantly associated with depression.
Several of the targeted variables were predictive of subsequent depression. Among participants with scores below the CES-D threshold at baseline (N=514), Kaplan-Meier analysis based on chi square log-rank tests indicated that participants who had lower than median baseline self-esteem scores (χ2=8.25, df=1, p=.004), mastery ratings (χ2=15.27, df= 1, p<.001), daytime sleep quality ratings (χ2=8.99, df=1, p=.003), social activity ratings (χ2=26.67, df=1, p<.001), and pleasant activity ratings (χ2=16.04, df=1, p<.001) all had a significantly higher risk of subsequently exceeding the CES-D threshold. However, no significant association was observed between the preventive program and any of these variables.
Discussion and conclusions
Preventive programs can have a substantial impact on disease burden if they can alter risk and reach a large proportion of the target population. Reports of successful treatment using automated cognitive-behavioral approaches (
10) suggest that it may be possible to deliver preventive programs by using distance technologies. The preventive program we developed was not found to be more efficacious than providing general information about depression, which is already widely available on the Web. Our analysis indicated that several of the targeted variables—such as self-esteem and social activity—were associated with depression. These variables may yet prove to be useful targets for prevention. Future studies should focus on the capacity of preventive interventions to alter risk-modifying variables. Such research may benefit from an in-depth analysis of the users' experience with distance technology programs, including their understanding of the material and its impact on their cognitions and behavior.
Acknowledgments
This project was funded by the Health Research Fund, administered by the Alberta Heritage Foundation for Medical Research, and by a grant from the Calgary Health Region. Dr. Patten was supported by a Population Health Investigator Award from the Alberta Heritage Foundation for Medical Research.