About one-third of all homeless single adults have severe and persistent mental illness and suffer from neuropsychological impairments in attention, executive functioning, verbal memory, and general intellectual functioning (
1,
2). Among persons with schizophrenia, these impairments are associated with poor community functioning and poor social skills (
3). The results of previous research suggest that training and medication, especially atypical antipsychotics, can improve some aspects of neuropsychological functioning among persons with schizophrenia (
4).
In this study we assessed whether neuropsychological functioning is also associated with the receipt of housing and the type of housing received. Although this question has not been studied among persons with severe and persistent mental illness, previous research has indicated beneficial effects of housing, including reduced hospitalization rates (
5), improved residential stability (
6), social support, and improved client satisfaction (
7). We have previously reported differential gains in residential stability by housing type (
8), further highlighting the importance of structured environments in the course of treatment for persons with severe and persistent mental illness (
9).
In this study, homeless persons with severe and persistent mental illness were randomly assigned to either independent apartments or staffed group homes. We tested two hypotheses. First, we hypothesized that overall neuropsychological functioning would improve significantly across the full study sample over 18 months. Our second hypothesis was that executive functioning—measured by the Wisconsin Card Sorting Test (WCST)—would improve more among persons assigned to group homes than among those assigned to independent apartments.
Methods
The Boston McKinney Project was a controlled field trial of distinct residential alternatives for a population of homeless persons with severe and persistent mental illness (
2,
6,
8). A total of 112 persons were recruited from three shelters for homeless adults with mental illness, where they had been in stable residence for a median duration of about two months. These participants gave written informed consent and were paid for participating in the study. They were subsequently randomly assigned to either a group home (N=61) or an independent apartment (N=51) and completed neuropsychological testing an average of 32 days before they moved into their housing assignments (
2). The study began in 1990 and ended in 1995. All procedures were approved by the appropriate institutional review boards.
The study participants' clinical case managers arranged follow-up neuropsychological testing for 91 participants who completed the study (80 percent)—52 who were assigned to group homes and 39 who were assigned to independent apartments—at an average of 18 months. The background and clinical characteristics of the participants who completed the study were similar to those reported in other studies of homeless persons with severe and persistent mental illness (
1,
5,
6). No significant differences in demographic or clinical characteristics or baseline neuropsychological performance were observed between participants who completed the study (N=91) and those who did not (N=21).
Independent apartments and group homes were distinct residential alternatives (
6): independent apartments were single-occupancy units, whereas each group home accommodated six to ten persons in separate bedrooms but with shared facilities. The group homes were "evolving consumer households"—designed so that residents could assume greater control of the residence over time by taking on staff responsibilities, from daily chores to managing the household as a self-governing group (
8).
No significant differences were noted in baseline neuropsychological functioning or sociodemographic characteristics between participants assigned to the two housing conditions, either for the full sample or for the 91 participants who participated in the 18-month follow-up. Nor were significant between-group differences noted in the number of participants who remained in their initial housing assignments throughout the study period (69 percent of participants assigned to group homes and 68 percent of those assigned to independent apartments) or in the percentage who participated in the 18-month follow-up (85 percent of participants assigned to group homes and 76 percent of those assigned to independent apartments), although participants who were assigned to group homes were less likely to have any subsequent periods of homelessness (14 percent compared with 31 percent, χ
2=4.04, df=1, p=.044). Service use throughout the study period did not differ significantly by housing type (
10).
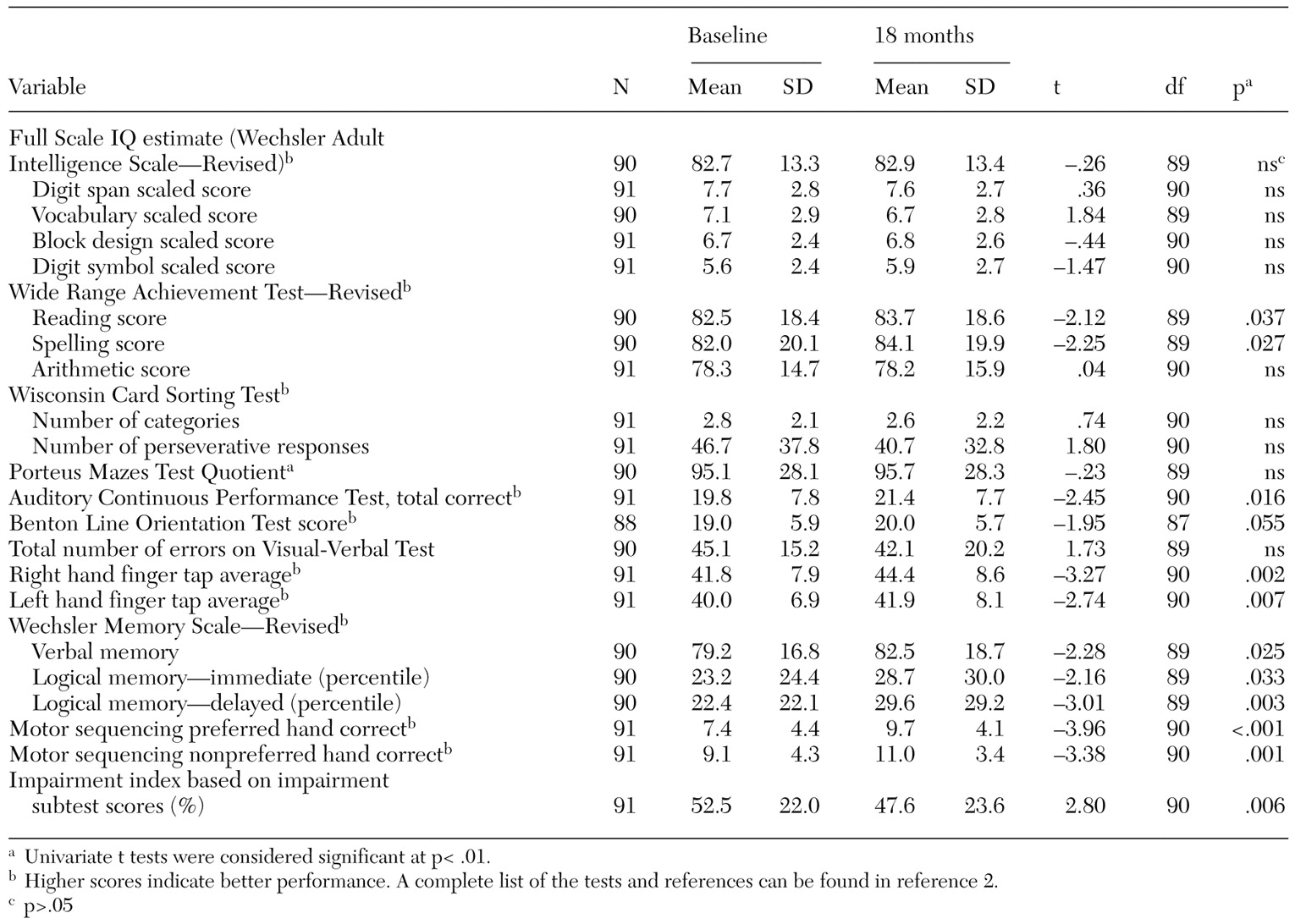
The same neuropsychological battery was used at both the baseline and follow-up assessments. We created an overall impairment index based on the percentage of scores on the 20 impairment subtests listed in
Table 1 (
2). We measured several variables that might have differed by housing assignment and that could have influenced neuropsychological functioning: substance use, medication dosage (chlorpromazine and benztropine equivalents) and case manager-reported medication compliance, size of social network, change in the amount of time case managers spent with each client, time devoted to mental health services during the first and last six months in residence, and time spent in the assigned housing condition.
We used Hotelling's T2 to test our hypothesis that there would be significant (p<.05) overall improvement in neuropsychological functioning from baseline to follow-up, followed by two-tailed paired t tests for 20 test scores and the impairment index. A significance level of p<.01 was used to test significance for univariate comparisons. We used analysis of covariance to test the hypothesis that there would be greater improvement among participants assigned to group housing than among those assigned to independent apartments, with the change in the WCST categories score as the dependent variable, controlling for changes in the six previously mentioned covariates that might have mediated or confounded housing effects (p<.05).
Results
Neuropsychological functioning improved significantly among the entire study sample from baseline to follow-up, demonstrating an effect of time (Hotelling's T2=67.68, df=20, 66, p<.01, N=86). This change was also reflected in the overall impairment score (t=2.80, df=90, p=.006). The results of univariate analyses indicated significantly improved performance on delayed verbal memory and on motor speed and sequencing.
Executive functioning (WCST categories scores) significantly declined among the participants who were assigned to independent apartments (3.2 compared with 2.3, t=2.41, df=37, p=.021) and increased slightly among those who were assigned to group homes (2.5 compared with 2.8, not significant). The effect of housing type on WCST scores was statistically significant (F=5.70, df=1, 82, p=.019). Other covariates—for example, time spent in the assigned housing condition and substance use rates—did not significantly account for these results.
Discussion and conclusions
The results of this study support the idea that the provision of housing can influence neuropsychological performance among homeless persons with severe and persistent mental illness. Both the experience of being housed and of living in group housing rather than independent apartments had effects on cognition among the participants in this study.
We cannot definitively conclude that housing itself improved general neuropsychological functioning, because there was no comparison group of homeless persons who did not receive housing. Nor can we rule out improvement due to practice effects. However, our findings are consistent with the results of previous research that showed multiple benefits of residential stability for persons with severe and persistent mental illness (
5,
6,
7). Moreover, over such a long interval between baseline and follow-up, practice effects are unlikely (
2,
4). Although overall neuropsychological improvement was apparent in our sample, the number of tests performed is cause for caution in interpreting specific effects.
Because the study participants were randomly assigned to the two housing conditions, were comparable at baseline, received comparable treatment throughout the study, and were not differentially affected by the potential confounders we identified, such alternative explanations cannot account for the association of housing type with WCST scores. The changes are unlikely to have been caused by differences in attrition rates, because no significant differences were noted in baseline performance between participants who completed the study and those who did not.
Consistent with our second hypothesis, differential gains in performance were found among participants assigned to group homes, yet primarily differential losses were noted among those assigned to independent apartments. We speculate that this finding was due to the baseline experience of the participants, who were all recruited from stable homeless shelters. Relative to this baseline experience, a move to an independent apartment was characterized by a loss of social structure and interaction, whereas a move to a group home did not represent a substantial change. We encourage further research to identify the specific aspects of group or independent living that affect executive functioning and the subgroups that are subject to such differential effects.
The results of this study suggest that improved neuropsychological functioning can be added to the advantages to be derived from providing housing to persons who have severe and persistent mental illness. Admittedly, the improvements we observed were modest, and the sample remained significantly impaired. Nevertheless, the fact that improvements in neuropsychological functioning were demonstrated offers some hope that homeless persons with severe and persistent mental illness can develop more adaptive levels of functioning. Future research should test whether improvement in these functions is associated with improved social skills and community functioning.
Acknowledgments
This research was supported by McKinney grant R18-MH-4808001 from the National Institute of Mental Health to Dr. Goldfinger and by grants from the National Association for Research in Schizophrenia and Depression to Dr. Caplan and Dr. Seidman. The authors thank Barbara Dickey, Ph.D., and Walter E. Penk, Ph.D, for their contributions to the study; Jill M. Goldstein, Ph.D., for comments on an earlier version of the manuscript; and Nicholas J. Horton, Sc.D., and Jessica Su, M.S., for statistical advice.