Patient-centeredness is essential to high-quality medical care (
1) and involves eliciting information about patients' needs and preferences for treatment. Attention to patients' preferences is ethically desirable and may improve entry and retention in care, especially for minority populations whose needs and preferences may differ from those of other patients (
2) and who have lower rates of care (
3). Patients' preferences are particularly salient in depression treatment, because multiple efficacious treatments (for example, antidepressants and psychotherapies) and modalities (for example, group and individual) exist.
Conjoint analysis, widely used in market research, is now being adapted for measuring health care preferences (
4). Grounded in economic theory, conjoint analysis assumes that consumers make choices among products by considering characteristics or attributes—for example, size, color, and brand—and making trade-offs among these attributes to arrive at a final choice. In a conjoint analysis survey, consumers are presented with hypothetical products with varying combinations of attributes and are asked to choose among the products (
4). Conjoint analysis is unlikely to allow respondents to choose what they think they should choose, is predictive of behavior, and is easy to administer (
5). However, conjoint analysis surveys require complicated cognitive processing (
4), and it is unknown whether conjoint analysis can reliably assess the treatment preferences of low-income, low-literacy groups who have little treatment experience.
Before conducting a full-scale validation, we examined the feasibility (the rates of survey acceptance and completion) of conjoint analysis to measure preferences for depression treatment and the strategies to reduce barriers to care among depressed, low-literacy Latino primary care patients.
Methods
The study was approved by the human subjects committees of the Los Angeles County University of Southern California Medical Center, the University of California at Los Angeles, and Charles R. Drew University and took place at a central Los Angeles primary care clinic that serves mostly Latino low-income patients with Medicaid or no insurance.
English- and Spanish-speaking patients aged 18 years or older who were seen for outpatient appointments in the general medicine and women's clinics from March to August 2002 were approached for screening in waiting rooms by bilingual study personnel. After the participants gave verbal consent, they were screened for major depression by using the Personal Health Questionnaire, a self-report version of the PRIME-MD (
6), and for dysthymia by using three additional questions from the PRIME-MD (
7).
Patients with major depression or dysthymia were eligible for the study, and those with suicidal ideation, a history of bipolar or psychotic disorder on the basis of screening questions from Project IMPACT (
8), or evidence of gross cognitive impairment were excluded. After we received written informed consent, the eligible patients completed a conjoint analysis survey.
To design the conjoint analysis survey, we defined attributes, assigned attribute levels, and created hypothetical scenarios. Attributes of depression interventions and strategies to reduce treatment barriers were identified from previous treatment interventions (
8,
9), clinical guidelines (
10), and focus groups. For treatment choice, levels were assigned for treatment type (counseling, antidepressants, and a combination of the two), treatment format (individual or group), and treatment location (primary care or mental health clinic). For barrier-reduction strategies, levels were assigned for system navigation (help making appointments versus no help), reducing transportation barriers (bus pass, telephone appointments, or no assistance), and educational interventions (individual education session, group education session, pamphlets, or videos).
Attribute levels were combined to create hypothetical treatments or barrier-reduction strategies. For example, treatments might be individual counseling at the primary care clinic or a medication group at a mental health clinic. Each survey included 12 pairwise comparisons of treatment scenarios and 12 pairwise comparisons of barrier-reduction scenarios that were determined by using a fractional factorial design. The survey was administered in English or Spanish with visual depictions of combinations; copies are available on request. Brief descriptions of treatment and barrier-reduction strategies were read to patients from a standardized script before the survey was administered. For each pair of scenarios, the patients were asked to select the one they preferred.
We assessed gender, age, education, country of origin, and ethnicity. Items from the Partners in Care study (
9) assessed self-rated health and previous use of counseling or psychotropic medication.
Patient characteristics were examined with descriptive statistics. A random utility model was used to create binary logit estimates of treatment and barrier-reduction preference parameters (
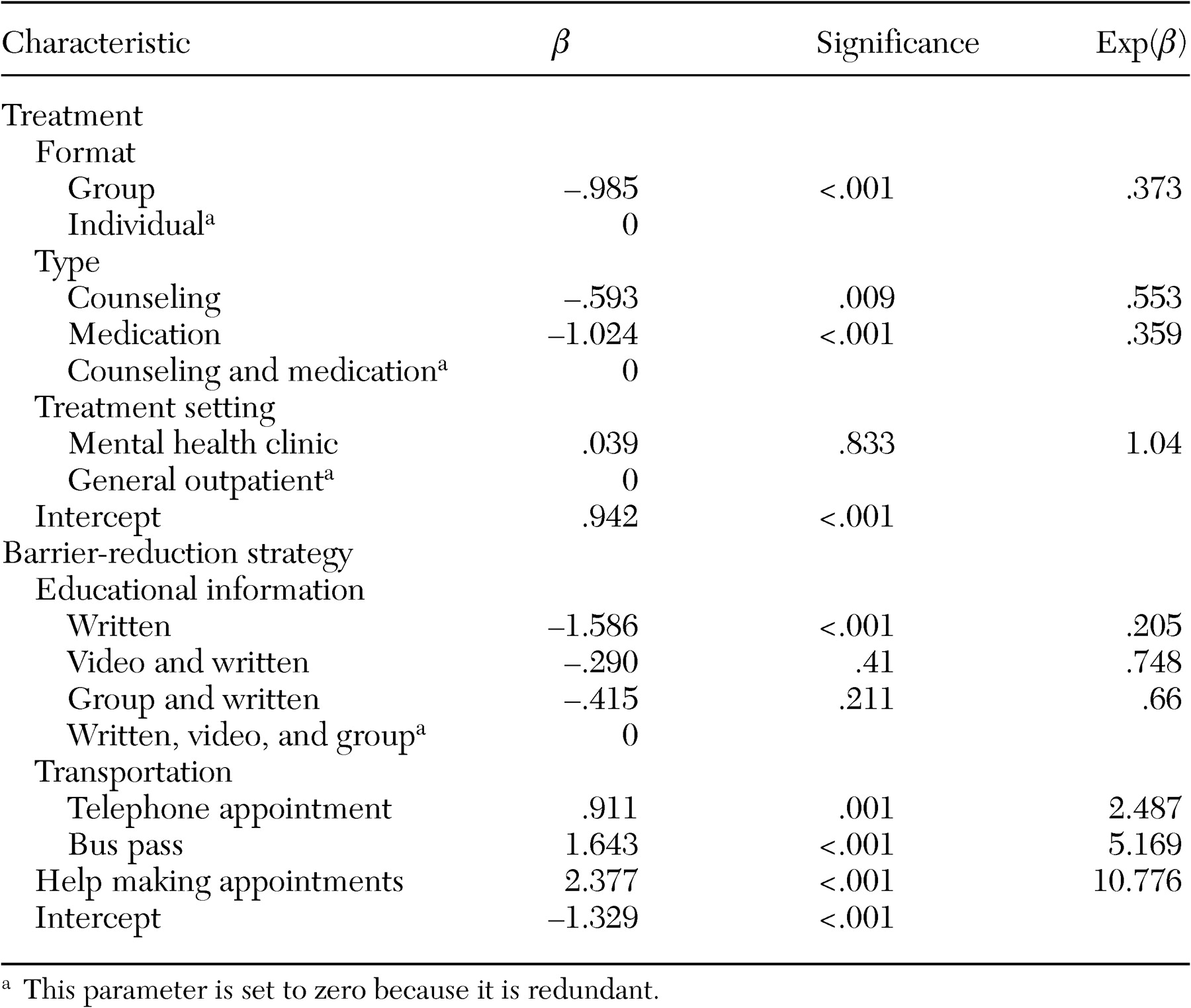
5). For each regression, the dependent variable was a binary indicator of treatment acceptance, and independent variables were the attribute levels. The estimated β coefficients indicate the relative utility of each attribute level, with positive values indicating stronger preference. The exp(β) represents the odds that a particular attribute level will increase overall treatment acceptance. Fixed-effects variance components models were used to determine whether main effects varied significantly on the basis of individual patient characteristics. Data were analyzed by using the SPSS 11.5 multinomial logit regression procedure.
Results
Of the 276 patients we approached, 241 (87 percent) agreed to participate in the screening. Forty-two (58 percent of 72 who were eligible) agreed to complete the survey. Of these, 20 (48 percent) had dysthymia, six (14 percent) had major depression, and 16 (38 percent) had both. Most were women (40 patients, or 95 percent); were Latino, mostly from Mexico and El Salvador (39 patients, or 93 percent); were aged 31 to 65 years (34 patients, or 81 percent); and had fair or poor self-rated health (30 patients, or 82 percent). Many of the patients had fewer than six years of education (22 patients, or 52 percent), and most completed the surveys in Spanish (36 patients, or 86 percent). Although 12 patients (29 percent) had had previous counseling and 14 (33 percent) had previously taken psychotropic medication, only two (5 percent) were currently in treatment.
Table 1 presents the results of the conjoint analysis survey. Study participants significantly preferred individual to group treatment and counseling plus medication to either approach alone and showed no significant preference for treatment setting. Educational materials significantly enhanced the likelihood of treatment acceptance, with additional education cumulatively increasing the odds of treatment acceptance. The odds of treatment acceptance were increased more than twofold by the availability of telephone appointments, fivefold by the availability of bus passes, and tenfold by the availability of assistance in making appointments. Preferences were stable across individual characteristics.
Discussion and conclusions
To our knowledge, conjoint analysis has not previously been used to assess health care preferences among low-income, low-literacy Latinos. When visual depictions and simple standardized descriptions were used, depressed patients with little education could complete surveys without difficulty. However, the survey response rate (58 percent) was lower than those in conjoint analysis surveys of nondepressed samples with higher incomes and education levels (
4).
By mimicking the actual decision-making process in which trade-offs must be made between the attributes of a product or service, conjoint analysis may yield more realistic results than those obtained from traditional attitude surveys, which ask about each attribute separately (
4). Conjoint analysis also estimates the relative utility of intervention attributes, allowing decision makers to prioritize those components when resources are limited. In our sample, strategies to overcome access barriers had greater utility than treatment attributes. Finally, conjoint analysis surveys produce a relatively large data set for a small number of respondents by obtaining multiple observations for each individual.
Our small homogeneous sample and modest response rate reduced the precision of our estimates and the generalizability of the results. Future validation studies will require increased recruitment efforts, especially for men, and should compare preferences measured on conjoint analysis with observed treatment choices. Few of the study participants had experience with depression treatment, which perhaps limited informed decision making. It is unknown whether depressive symptoms might impair the ability to weigh options in conjoint analysis surveys. Future studies should thus examine the effect of treatment exposure and improvement in depressive symptoms on preferences. Willingness to pay for treatment options should also be assessed.
Evaluating patients' preferences is an essential step in developing patient-centered interventions. Although they require validation, our pilot findings suggest that conjoint analysis is feasible for measuring depression treatment preferences among low-income Latino patients.
Acknowledgments
This study was supported by an unrestricted educational grant from Pfizer, Inc., and the UCLA/NIMH Faculty Scholars Program (NIMH grant K-12-MH00990-01-01; Kenneth B. Wells, M.D., M.P.H., primary investigator). The authors thank Jennifer Green for her help with data collection and in manuscript preparation.