Many Americans receive mental health care under capitated financing in which governments and private insurers pay providers a fixed amount per year for each insured person regardless of the amount and types of treatment provided (
1). Cost containment has been the principal motivation for implementing capitation. Advocates for capitation argue that fee-for-service financing encourages providers to increase their income by providing unnecessary services. Capitation presumably reverses this incentive, because providers, rather than insurers, bear the cost of unnecessary treatment (
2). Much empirical research into the effects of capitation reports that shifting the cost of excess treatment to service providers reduces the use of services, particularly inpatient services (
3,
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15).
The principal criticism of capitation has been that the allure of income causes providers to neglect clients' needs, thereby inducing greater severity of illness than expected under fee-for-service financing. Little empirical work has directly tested this proposition. Instead the work focuses on indicators of good clinical practice. The literature has given much attention, for example, to compliance with pharmacotherapy (
16,
17,
18,
19). This indicator has wide acceptance because failure to comply with pharmacotherapy increases the risk of worsening symptoms, which can have negative implications for the client as well as for his or her family and community.
A Utah study found reduced prescriptions of recommended dosages of antipsychotic medications under capitation (
16). A Tennessee study reported that capitation of the reimbursement of Medicaid mental health providers coincided with a decreased likelihood that mentally ill consumers adhered to pharmacologic regimens and with a reduction in the length of time clients were prescribed antipsychotic drugs (
17).
At least two studies raised questions concerning the external validity of the Utah and Tennessee findings. Capitation did not coincide with any changes in the type or dosage of antipsychotic drugs prescribed to persons with schizophrenia enrolled in the Massachusetts Medicaid program (
18). In Colorado, use of antipsychotics did not differ between capitated-reimbursement and fee-for-service areas, and utilization of second-generation antipsychotics was higher in the areas that had capitated reimbursement (
19).
Reduced pharmacotherapy does not, moreover, axiomatically mean a decrement in the quality of care. The argument for capitation implies that pharmacotherapy may be overused under fee-for-service financing because a provider may prescribe drugs beyond their useful period. The provider thereby incurs no cost but reduces the chances, however small, of being accused of stopping treatment prematurely.
The failure of the pharmacotherapy research to converge on what effect, if any, capitation has on pharmacotherapy, combined with the fact that reduced drug treatment in an insured population does not necessarily imply increased incidence of illness, suggests that other outcomes should be studied to help settle the debate about the effects of capitation on the well-being of enrollees. We attempted to further that debate by assessing the use of psychiatric emergency services by populations whose mental health coverage shifted from fee-for-service to capitated financing. Our analysis examined psychiatric emergency services provided by general hospital emergency departments.
Although differentiating "inappropriate" from "appropriate" use of psychiatric emergency services has proven controversial (
20), little controversy surrounds the objective of reducing both categories of use. Research has regularly reported much inappropriate utilization of psychiatric emergency services (
21,
22). Studies have found that many clients receiving psychiatric emergency services could be treated less expensively and more effectively in outpatient settings (
23,
24,
25,
26).
Mental health services researchers have argued, moreover, that a well-functioning mental health system with good outpatient services would minimize appropriate utilization of psychiatric emergency services by preventing episodes of serious illness (
27,
28,
29,
30). Research indicates that utilization of psychiatric emergency services gauges the effectiveness of a mental health system (
31,
32).
Although the mental health services literature cites the use of psychiatric emergency services as an indicator of a system of care's effectiveness, few empirically based studies have focused on emergency treatment under capitation. Two studies of children reported contradictory results. A Colorado assessment found no persistent changes in the use of psychiatric emergency services by children under capitated financing (
33). A Massachusetts's study found evidence of increased utilization of psychiatric emergency services (
34). Two studies involving overlapping populations of severely mentally ill adults in Massachusetts (
35,
36) and studies of adults in Minnesota (
37) and Utah (
6) reported no change with capitation.
We used rigorous time-series techniques to test the hypothesis, implied by the critics of capitation, that shifting the financial risk of excess treatment to providers leads to neglect of clients' needs and, in turn, to an increase in the use of psychiatric emergency services.
The study was conducted in conjunction with a project approved by the institutional review board at the University of California, Berkeley.
We used data from Colorado to test our hypothesis. Concerned about rising costs in its Medicaid program, the Colorado legislature in 1992 created a demonstration project that financed services on a prepaid and capitated basis. To participate in the demonstration project, 14 of Colorado's 17 community mental health centers reorganized themselves into seven new agencies that contracted with the state to provide mental health services to Medicaid recipients in separate geographic areas. Four of these newly formed agencies continued to operate independently on a not-for-profit basis and received capitated payments directly from the state. Three agencies, which received capitated reimbursement, entered a joint venture with a for-profit behavioral health organization that provided administrative services and contracted with community hospitals and other external providers. The three remaining community mental health centers continued to operate on a fee-for-service basis during the study period.
The not-for-profit agencies began operating on August 1, 1995. The for-profit providers started on September 1, 1995. Providers were initially paid a capitated-reimbursement rate based on historical patterns of utilization of psychiatric emergency services in their regions. The agencies received prospective payment each month with subsequent adjustment to reflect changes in enrollment. The agencies assumed full financial risk for outpatient mental health services, including emergency department visits, and for inpatient mental health services provided by community hospitals to all Medicaid enrollees. They were also at risk for state hospital services provided to children and to adults 65 years of age and older. State hospital services for enrollees between the ages of 22 and 64 were not included because Colorado's Medicaid program does not cover state hospital services for persons in this age group. The agencies were not at risk for the cost of psychotropic medications (
3).
The not-for-profit agencies were allowed to accumulate savings from unused capitated payments from the state. Agencies could use these resources to enhance programs for all clients, including clients not enrolled in Medicaid. The joint venture of three state-contracted agencies and a for-profit behavioral health organization could earn a profit of up to 5 percent of the contract value. Agencies had to use profit beyond 5 percent to enhance client services (
3).
Methods
Analyses
Our analyses were in the tradition of the interrupted time-series quasi-experiment (
38). The null hypothesis for such tests assumes that the postintervention values of the dependent variable do not differ from values expected from the preintervention series. The fact that such series often exhibit autocorrelation, including trends, cycles, and the tendency to remain elevated or depressed after high or low values, complicates arriving at the values expected from the preintervention series. Researchers typically solve this problem by identifying autocorrelation and expressing it as an effect of earlier values of the dependent variable itself.
The Colorado experience allowed us to go beyond modeling autocorrelation. State implementation of capitation in a subset of counties allowed us to measure the dependent variables in the unaffected fee-for-service counties and to use the series as control variables in the test equation. This approach provided the benefit of the typical approach because it removes any autocorrelation in the dependent variable induced by forces also at work in the fee-for-service counties. The approach had the added benefit of controlling for third variables that exhibit no autocorrelation and affect capitated and fee-for-service areas. Such a third variable could have induced a type I error if it had changed coincidentally when capitation began.
Our tests proceeded through these steps. First, we created weekly time series of the number of emergency treatment episodes begun in each of the 109 weeks starting July 8, 1994. Hospitals provided all the psychiatric emergency services counted in this study. The hospitals then billed the capitated agencies for services provided.
Second, we separately modeled the two series from the capitated areas as a function of the series from the fee-for-service areas. We modeled a total of 105 weeks for each area by centering capitation at week 53, which gave us symmetric pre and post periods of one year for both areas. Third, we inspected the residuals from step 2 for autocorrelation. We used the strategy attributed to Dickey and Fuller (
39) as well as Box and colleagues to identify and model autocorrelation (
40). The strategy, autoregressive, integrated, moving average (ARIMA) modeling, draws from a very large family of models available to empirically specify autocorrelation in time series.
The equation resulting from the above steps is as follows:
In this equation, ▿
d is the difference operator that indicates a series was differenced at lag d (values at t subtracted from values at lag t-d) to remove secular trends or cycles detected by the Dickey-Fuller test (
39). Z
t is the number of emergency episodes begun in week t in either the for-profit or not-for-profit capitated areas, X
t is the number of emergency episodes begun in week t in the fee-for-service area, ω is the estimated parameter for individuals served in the fee-for-service area, and ϕ is the autoregressive parameter. B is the "backshift operator" that yields the value of the series it conditions at time t-p for the autoregressive parameter or t-q for the moving average parameter. Seasonality in a series, for example, would result in p or q values of 6 or 12; θ is the moving average parameter and a
t is the error term for week t.
For the fourth step in the analysis, we inspected the residuals from the above equation for patterns consistent with our hypotheses. We searched for patterns in weeks 53 through 105, the week of capitation and each subsequent week up to one year later. More specifically, we used the method attributed to Demming (
41) as well as Alwan and Roberts (
42), and described by Liu and Hudak (
43), to detect "level shifts," or cases in which the residuals move above or below their 95 percent confidence interval (CI) (two-tailed test) and remain, on average, at the new level for the remainder of the test period or until a subsequent level shift. A level shift would be specified as follows:
In this equation, lt is a binary variable scored 0 for all weeks before the initial outlier in the period during which capitation would have had an effect, and 1 for all weeks after; ω2 is the increase or decrease in Z associated with lt.
We also used the methods described above to search for and to control level shifts in the weeks before capitation reform. Including these shifts in the models reduces variance in the error terms that could otherwise lead to false acceptance of the null hypothesis for the effects of capitation.
Data
We obtained data from the Colorado Medicaid Agency's administrative databases describing all visits to general hospital emergency departments by adult Medicaid beneficiaries with a primary mental or substance use disorder. We used Medicaid claims data and data from the "shadow billing" system that Colorado developed for the capitation demonstration project to enumerate emergency department visits. The Medicaid claims data were reported by general hospitals and physicians for services provided from July 1994 through August 1996. The encounter data in the shadow billing system were reported from August 1995 through August 1996.
Shadow billing files may underreport utilization of services because providers who receive capitated reimbursement do not have a financial incentive to track utilization (
14,
37). We believe the Colorado data on emergency department visits are accurate, because the agencies that did have capitated reimbursement do not provide these visits. Rather, these agencies reimburse hospitals for these services. The hospitals have a financial incentive to report visits to the agencies that had capitated reimbursement, and these agencies, in turn, have an incentive to track emergency department visits so that they can determine their expenditures for these services.
Results
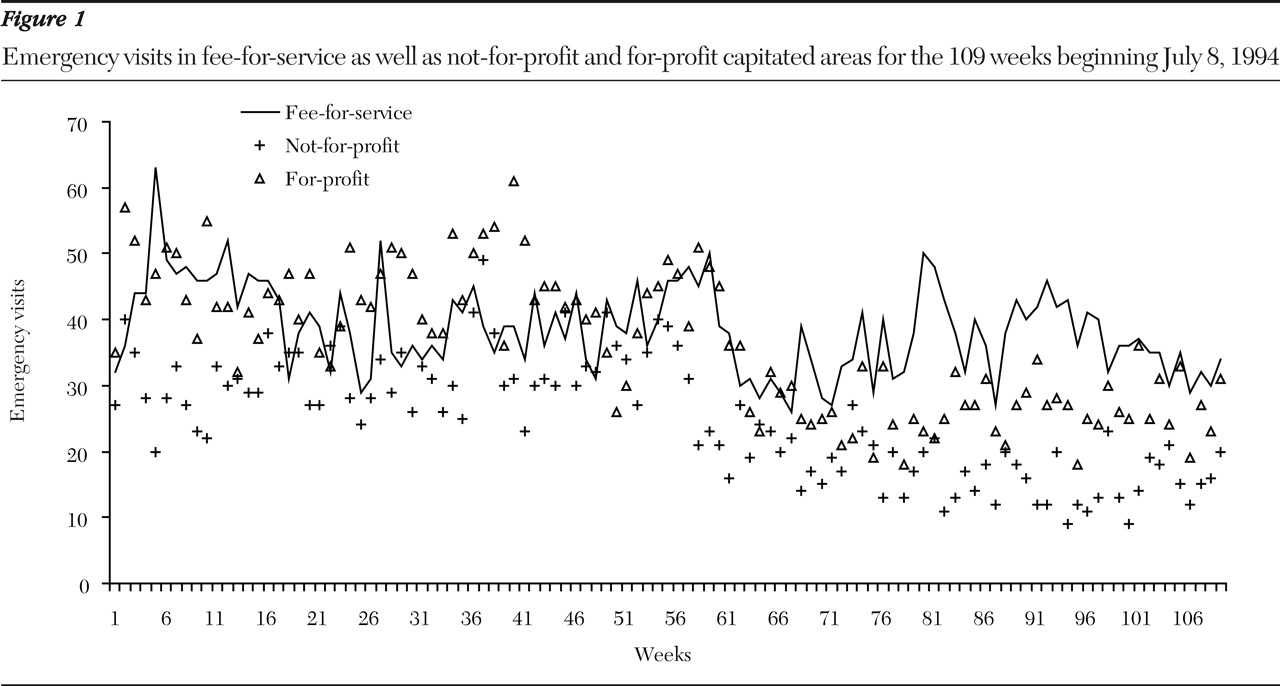
The series are plotted in
Figure 1. General hospitals in the fee-for-service areas treated an average of 26.2 emergencies per week over the 109-week observation period. Providers in the not-for-profit and for-profit areas treated an average of 20.1 and 29.0 emergencies per week, respectively.
Steps 1 through 3 above yielded the following equation for emergency episodes in the not-for-profit area:
▿Zt=-.0363▿Xt+(1-.8410B)at
The presence of the ▿ operators confirms that, as suggested by
Figure 1, the series exhibit a downward trend over the test period and required differencing. The coefficient (-.0363) for the fee-for-service area was not statistically different from 0 (p<.05, two-tailed test), implying that the two series did not move similarly around their downward trends. Therefore, the parameter was excluded from the remaining steps of the test. The moving average parameter (-.6410) was significantly (p< .05, two-tailed test) less than 0, implying an oscillation such that one week's movement from the downward trend was followed by a smaller value in the opposite direction.
Using the same procedures yielded this equation for emergency episodes in the for-profit area:
▿dZt=-.2590▿dXt+(1-.7699B)at
The ▿ operator on Zt indicates that utilization of psychiatric emergency services trended downward in the area financed with for-profit capitation and in the other two areas. The coefficient for the fee-for-service comparison area exceeded twice its standard error. The moving average parameter, similar in size and sign to that for the not-for-profit area, implies an oscillation around downward trend.
Step 4, inspecting for patterns in the residuals under not-for-profit capitation, found a level shift of seven visits per week below the CI of the expected value. The shift began during the week of August 6, 1995, one week after capitation started. This downward shift implies that in the year after capitation, providers in the not-for-profit area treated 30.6 percent fewer than the 1,190 psychiatric emergencies expected from trends, cycles, and other autocorrelation in the series over the two-year test period and from treatment patterns in the fee-for-service area. The results did not change if we included treated emergencies in the fee-for-service area as a control.
The residuals from the best fitting model of the for-profit area exhibited a level shift of 8.3 admissions per week below the CI of the expected value. The shift began during the week capitation started, the week of August 27, 1995. This downward shift implies that during the year after capitation, providers in the for-profit area treated 26 percent fewer than the 1,718 psychiatric emergencies expected from trends, cycles, and other autocorrelation in the series over the two-year test period and from treatment patterns in the fee-for-service area.
No other level shifts in the use of psychiatric emergency services appeared after capitation in either the not-for-profit or for-profit areas.
Discussion and conclusions
Shifting the cost of excess treatment from Medicaid to providers did not coincide with a sustained increase in utilization of psychiatric emergency services provided by general hospital emergency departments in Colorado. On the contrary, after the implementation of capitation the use of psychiatric emergency services in capitated areas decreased to levels lower than those expected from trends, cycles, and other forms or autocorrelation and from use of services in areas where providers continued to be reimbursed on a fee-for-service basis. Trends were similar in areas of Colorado served by for-profit and not-for-profit providers who received capitated reimbursement. This decline persisted through the end of the first year after capitation.
The Colorado experience demonstrates that shifting the financial risks of excess treatment to providers does not necessarily reduce the quality of care, at least as gauged by the utilization of psychiatric emergency services by adults enrolled in Medicaid. In fact, assuming such risk may motivate providers to initiate practices that reduce both inappropriate and appropriate use of psychiatric emergency services. Providers in Colorado whose reimbursement was capitated, particularly those in the nonprofit area, expanded crisis services and other intensive outpatient and residential services aimed at obviating the need for hospital and emergency department use (
3). Findings from a previous study indicate that capitated providers in Colorado utilized second-generation antipsychotic medications, which were not covered under capitation, more extensively (
19). Greater use of second-generation antipsychotics may have improved adherence among consumers with schizophrenia, which may have, in turn, reduced their need for emergency department visits.
Our results, of course, may not generalize to other states. Colorado may have implemented capitation more effectively than did, for example, Tennessee and Utah. As the authors of the Tennessee study note, the transition to capitation in Tennessee was fraught with problems (
44,
45,
46). Colorado's transition was much smoother, perhaps because Colorado implemented capitation more slowly, delineated responsibilities more clearly, and gave traditional Medicaid providers a greater role in the program (
3). In addition, during the study period Colorado may have reimbursed capitated providers more generously than other states that implemented capitated reimbursements, which may have reduced providers' incentives to restrict access to services that might prevent psychiatric emergencies.
Finally, our results may not generalize in time. Our data are eight years old. Although the capitation schemes implemented in Colorado remain common, treatment and prevention alternatives may have changed and altered the likely response of providers to financial risk. Further study could help determine whether the effects we observed persist over time.
At the very least, our results suggest that the reflexive assumption that capitation is always detrimental to persons with mental illness is too simplistic. Having established that capitation affects access to and the quality of mental health services, we need to improve our understanding of the conditions under which capitation generates good, bad, or neutral outcomes for clients.
Acknowledgments
Funding for this research was provided by grant R01-MH-5413 from the National Institute of Mental Health. The authors thank the late Midge Starzyski, Ph.D., R.N., of Colorado Health Networks for her helpful comments on a previous version of this manuscript.