The prevalence of anxiety disorders is staggering, with approximately 18% of the population meeting criteria for an anxiety disorder in any given year (
1). Moreover, the prevalence of comorbid anxiety disorders is high; at least 50% of patients given a diagnosis of a principal anxiety disorder also meet the criteria for another anxiety disorder (
2,
3). The rate of comorbidity increases to 76% when including lifetime prevalence of anxiety disorders (
3). Given the high prevalence, efforts to improve the treatment of anxiety disorders are paramount.
Over the past several decades, considerable research has focused on the development of empirically supported treatments for anxiety disorders. Cognitive-behavioral therapy (CBT) is one form of treatment that has been shown to be efficacious with these disorders (
4,
5). Although these disorder-specific protocols are effective in treating symptoms of a given disorder, they are limited in that they may not adequately address comorbid disorders (
6,
7). As such, the development of treatment protocols that target multiple disorders concurrently is especially important to enhance the efficiency of treatment delivery for patients who have multiple symptom constellations.
Moreover, despite the efficacy of disorder-specific CBT protocols, the dissemination of these treatments to the community has been limited (
7,
8). One approach to enhance the dissemination of efficacious CBT treatments is the development of transdiagnostic treatment protocols. Transdiagnostic treatments aim to provide a parsimonious approach to treatment by creating protocols designed to treat multiple disorders. These approaches have been designed to treat disorders that are deemed to be similar in nature because they have the same underlying or maintaining factors and tend to be responsive to the same treatment mechanisms (
9–
11). These treatments have been shown to be efficacious in the treatment of anxiety disorders (
10,
11) and thereby provide an attractive alternative to disorder-specific treatment CBT protocols.
Schmidt et al. (
11) developed a transdiagnostic treatment approach for anxiety disorders called False Safety Behavior Elimination Treatment (F-SET). A major strength of F-SET is the straightforward nature of the techniques used during the intervention. F-SET was designed to treat multiple anxiety disorders concurrently by focusing on the identification and elimination of avoidance and coping strategies used by patients with anxiety. These strategies, called
safety aids, tend to be similar across anxiety disorders and play a central role in their maintenance (
12). As such, the F-SET protocol is especially helpful for clients with multiple anxiety conditions, who tend to use the same safety aids for each condition. Moreover, F-SET also aims to eliminate phobic attitudes by decreasing phobic behaviors through the use of antiphobic exercises. Antiphobic exercises are designed to provide clients with the most compelling type of disconfirmation of the beliefs that are likely driving their fear responses. Clients are told to behave in a manner that is the opposite of how they would normally react when feeling anxious, thereby encouraging the development of an antiphobic attitude. Whereas exposure exercises teach clients to habituate to their anxiety while in anxiety-provoking situations (e.g., speaking to a stranger), antiphobic exercises push clients further by having them engage in activities in which even those without anxiety would not typically engage (e.g., purposely trip and fall in front of others). Thus, clients are pushed beyond the realm of normal experience to provide powerful disconfirming evidence to dismantle the false fear structures maintaining their anxiety (
11).
The F-SET protocol has been shown to be efficacious when used as an individual treatment (
13) and as a transdiagnostic group treatment for anxiety disorders (
11). As an added benefit, the F-SET protocol is relatively brief, ranging from a five 60-minute session protocol when administered individually to an eight 90-minute session protocol when administered in a group setting.
A key feature of F-SET is the ease with which clinicians and clients can master the material. Specifically, the F-SET protocol uses techniques common to empirically validated CBT treatments for anxiety disorders, but these components have been streamlined and simplified to enhance the ease of learning the material. For example, most CBT protocols for anxiety disorders provide training in psychoeducation, cognitive restructuring, and exposure exercises. During the course of the F-SET protocol, clients receive psychoeducation, but training in cognitive restructuring and exposure is not specifically covered. However, through the process of fading and eliminating safety aids and the use of antiphobic exercises, clients frequently complete exposure exercises during the course of treatment (
11,
13). Throughout this process, clients are provided with corrective feedback with regard to their anxiety-related fears and learn that they are overestimating the likelihood and the potential negative consequences of their feared events.
Streamlining the more complex treatment material is an important feature of F-SET because it is not uncommon to encounter clients who have difficulty mastering the use of cognitive restructuring or are resistant to engaging in traditional exposure exercises. We have found the F-SET protocol to be especially helpful when working with these clients. Moreover, by removing the emphasis on cognitive restructuring and exposure exercises, F-SET allows clients to focus on fading their safety aids and developing antiphobic exercises. This allows clients to engage in behavioral changes as early as the first session, resulting in notable changes early in treatment. Finally, deemphasizing the focus on complex material has allowed us to create a treatment that is cost-effective because it requires fewer treatment sessions than other transdiagnostic treatment protocols (i.e., five sessions for individual treatment and eight sessions for group treatment) with a secondary aim of making the protocol easier for novice or master’s-level therapists to administer, thereby potentially enhancing the dissemination of this approach in the community.
This case study illustrates the use of the eight-session group F-SET protocol for a client given a primary diagnosis of panic disorder with agoraphobia (PDA) and a secondary diagnosis of generalized anxiety disorder (GAD). First, we illustrate the acquisition of treatment skills and subsequent reductions in anxiety symptoms. Second, we highlight the client’s use of similar safety aids for both PDA and GAD. Finally, we demonstrate a key strength of the F-SET protocol, the ease of acquiring F-SET skills, which provides the groundwork for clients to continue treatment on their own through the development of a treatment continuation plan. We review the client’s ability to use the F-SET skills on completion of treatment, resulting in enhanced treatment response. Specifically, we discuss an 11-month follow-up assessment to review treatment gains and the client’s experiences on completion of the eight-session protocol.
Case Study
Presenting Problems
Jill (the client’s name and identifying information have been altered to protect confidentiality) is a 20-year-old Caucasian woman who sought treatment at our specialized anxiety clinic for her anxiety, panic attacks, and worry. Jill reported that her anxiety was distressing and beginning to interfere with her schoolwork and socializing with her friends. Jill signed a form indicating consent for treatment and the release of information for research purposes.
During the intake interview, Jill’s primary complaint centered on experiencing recurrent panic attacks. Jill reported experiencing panic attacks every one or two days. Her anxiety typically increased throughout the day, and she frequently had panic attacks in the evening or at night when she was alone. Jill also reported experiencing pervasive worry about her health and the well-being of her family and friends, but she felt that her panic attacks were more bothersome than her worry.
History
Family and social.
Jill reported being raised by her biological parents in the southern United States. She reported some family history of anxiety, with her mother having a history of recurrent panic attacks. However, no anxiety problems were reported on her father’s side of the family. Jill has an older sister and a younger brother, neither of whom were reported to have experienced significant problems with anxiety.
Employment.
Jill was a full-time undergraduate student at a large southern university. She was not employed. Jill reported an escalation in her anxiety at the end of her first year of college after she transferred to a new undergraduate institution to complete her studies.
Medical and psychiatric history.
Jill denied a history of significant medical problems. She also denied a history of drug or alcohol use and reported that she did not take any medications on a regular basis. Jill was prescribed alprazolam (.5 mg) as needed, but she reported that she used it infrequently (i.e., one to two times a month). She also reported that she had not received counseling or psychiatric services before seeking treatment at our anxiety clinic.
Assessment
Clinical interview.
The Structured Clinical Interview for the DSM-IV (SCID-I/P;
14) was used to assess past or present Axis I psychopathology. The SCID-I/P has been shown to be a reliable and valid measure of
DSM-IV-TR (
15,
16) Axis I disorders. The SCID-I/P was administered by an advanced doctoral student in clinical psychology who had received comprehensive training in administering structured interviews to ensure high interrater reliability for Axis I conditions (
17). Reliability was established by reviewing a random sample (N=16) of diagnostic interviews that were conducted in the anxiety clinic at the same time as Jill sought treatment. The interviews were reviewed by a rater independent of the initial evaluation. All primary diagnoses were represented in this sample, and the ratings demonstrated perfect interrater agreement for the primary Axis I diagnosis. The 11-month follow-up was conducted by an advanced graduate student blind to the client’s diagnoses at intake to control for possible biases during the follow-up assessment.
At intake, Jill received a principal diagnosis of PDA. Jill reported that her panic attacks had started approximately a year before the intake interview and that her panic had progressively worsened over time. At the time of intake, she was experiencing spontaneous or limited-symptom panic attacks on a nearly daily basis. At times, she would have multiple panic attacks a day. Jill’s anxiety tended to increase throughout the day, frequently resulting in panic attacks during the evening or night. Because of this, Jill avoided being home alone and also avoided going out late at night because she viewed being alone or staying out late at night as triggers for her panic attacks. She depended on her roommates to ensure she was never home alone. In addition, she also avoided going places alone. She avoided crowded places, such as grocery stores, movie theaters, and restaurants, and she also avoided driving alone. She reported that she typically went into crowded places or drove only if she was with a friend. Interestingly, Jill also reported that while she had difficulty going places alone, her anxiety was worse if she was at home alone during the evening. When she was in public, she always had someone available if she needed help, which was not the case when she was at home alone. Thus, Jill structured her life and activities so that she would not be home alone and would always have a friend to go places with her.
Despite these difficulties, Jill was able to consistently attend class, although she did report a fear of having a panic attack in class, resulting in difficulty concentrating. Jill was also highly attuned to changes in her bodily sensations. She tended to monitor her body for any changes in sensations (e.g., increase in pulse, weakness in her arm) that might be a sign of an impending panic attack. Because of this, Jill frequently checked her pulse and avoided activities that would result in physiological changes. For example, Jill revealed that she no longer engaged in exercise (e.g., running, playing tennis) because she was afraid of inducing panic attacks or making them worse. This was especially bothersome for Jill because she had always been active and had engaged in a regular exercise routine of running, swimming, and playing tennis before she began having panic attacks.
Jill also endorsed pervasive and uncontrollable worry consistent with a diagnosis of GAD. Jill reported that she had always been a worrier but that her worry had worsened over the past year. When worrying, she experienced feelings of restlessness, tiring easily, muscle tension, and feeling on edge. She also reported worrying about everything and being afraid that something bad would happen. One of Jill’s primary worry domains revolved around concerns about her health. She frequently worried about getting a serious medical illness (e.g., heart disease) or having a serious allergic reaction, despite being in good health. She also frequently checked medical Web sites to determine whether various physical symptoms she experienced were consistent with the symptoms for a serious medical illness.
Jill also tended to be overly cautious and avoided situations and things that might result in her getting sick. For example, she closely monitored her food intake, avoiding all raw vegetables and any food items that made her feel as though she might be having an allergic reaction. For example, Jill reported that she stopped eating peanut butter because she thought her lip was numb after eating it on one occasion, despite regularly eating it as a child and adolescent. She also reported a fear of having an allergic reaction if she got stung by a bee or an insect and would at times avoid the outdoors. Jill also reported worrying about her schoolwork, fearing that she would not do well in her courses, despite being an A student. Jill engaged in perfectionistic and rigid behaviors (i.e., structured schedule) to reduce her worry and anxiety. Jill’s rigid schedule ensured that she would always be on time and that she could complete her tasks (e.g., school assignments) early. She would get very upset if her daily schedule was altered. Because of this, if a scheduled activity (e.g., meeting up with friends) was changed to a different time, she would get very anxious and often would not go to the event because it altered her schedule.
Jill was also assessed for mood and substance use disorders. Jill endorsed experiencing minimal depressive symptoms (e.g., low mood and anhedonia a couple days a month); however, she did not meet the criteria for major depressive disorder. Alcohol and substance use disorders were ruled out because she did not report alcohol or drug use.
On the basis of her report, Jill was given a diagnosis of PDA and GAD during the intake interview. Symptom severity was assessed using the Clinical Global Impressions Scale (CGI;
18), a clinician-rated tool to assess overall degree of impairment in functioning. The CGI is rated on a seven-point Likert scale (rated from 1, normal, not at all ill; 4, moderately ill; to 7, among the most extremely ill patients). During the intake, Jill was given a clinical severity rating of 5 for her PDA diagnosis and of 4 for her GAD diagnosis.
Self-report measures.
The Anxiety Sensitivity Index (ASI;
19) was used to measure anxiety sensitivity. The ASI is a 16-item scale that is used to assess the fear of anxiety and the potential cognitive, social, and physiological consequences associated with anxiety (e.g., “It scares me when I feel shaky”). Respondents are asked to indicate the degree to which they agree or disagree with each item on a five-point Likert scale (rated from 0, very little, to 4, very much). Elevated anxiety sensitivity has been shown to be closely associated with the development of panic attacks (
20,
21) and panic disorder (
22). Moreover, reductions on the ASI are associated with a reduction in panic symptoms (
23,
24). The ASI has been shown to be a valid and reliable measure of anxiety sensitivity (
19). ASI scores higher than 25 indicate a clinically significant level of anxiety sensitivity. At baseline, Jill scored a 43 on the ASI, indicating a high level of anxiety sensitivity.
The Beck Anxiety Inventory (BAI;
25) was used to assess general level of anxiety. The BAI is a 21-item self-report measure that assesses the overall clinical severity of anxiety symptoms associated with multiple anxiety diagnoses. Participants are asked to indicate the level to which they have perceived various anxiety symptoms as bothersome during the past week. The items are rated on a four-point Likert scale (rated from 0, not at all, to 3, severely, I could barely stand it). The BAI has been shown to be a reliable and valid measure of anxiety (
25). Scores on the BAI range from 0 to 63, with higher scores indicating greater levels of anxiety (0–7, minimal anxiety; 8–15, mild anxiety; 16–25, moderate anxiety; >36, severe anxiety). At baseline, Jill scored a 29 on the BAI, indicating a moderate level of general anxiety.
The Beck Depression Inventory–II (BDI-II;
26) is a 21-item self-report scale for measuring symptoms of depression. Participants are instructed to rate the severity of symptoms items on a four-point Likert scale. The BDI-II has been shown to be a reliable and valid measure of depression (
27,
28). Scores on the BDI-II range from 0 to 63, with higher scores indicating a greater level of depression (0–13, minimal depression; 14–19, mild depression; 20–28, moderate depression; 29–63, severe depression). At baseline, Jill scored a 16 on the BDI, indicating mild symptoms of depression.
The Penn State Worry Questionnaire (PSWQ;
29) is a 16-item self-report questionnaire assessing pervasive and uncontrollable worry. Respondents are asked to indicate the extent to which each item (e.g., “Once I start worrying, I cannot stop”) is typical of them on a five-point Likert scale (rated from 1, not at all, to 5, very). Scores range from 16 to 80, with higher scores reflecting greater levels of worry. A score of 65 or higher indicates a clinical level of worry (
30). At intake, Jill’s PSWQ score was a 68.
The Safety Behavior Checklist (SBC) is a self-report measure composed of 76 items that assess the frequency of safety aid use (
11). Respondents are asked to rate the frequency of use of each safety aid in general and in feared situations separately on a 10-point Likert scale rated from 1 (never) to 10 (always). Lower scores on the SBC indicate lower levels of safety aid use. The SBC has been used in previous studies to measure the use of safety aids (e.g.,
11). Because clients tend to be unaware of their safety aids before starting treatment, the SBC was not administered until after Session 1 to ensure that Jill was aware of the definition of a safety aid.
Case Conceptualization
Consistent with the current conceptualization of the nature of anxiety and the maintaining factors of these disorders (
31), Jill used numerous avoidance behaviors and coping strategies related to her anxiety. Like many patients with anxiety, she engaged in extensive use of safety aids. Safety aids are believed to play a central role in the maintenance of anxiety disorders (
11,
31). Although safety aids are effective at reducing anxiety in the short term, they prevent clients from learning that what they fear is not actually as bad as they perceive it to be. Over time, the continued use of safety aids results in a feedback loop in which clients habitually engage in the use of safety aids to immediately reduce their anxiety. Clients often become increasingly dependent on these strategies to help cope with their anxiety and to help them function on a daily basis.
The F-SET protocol focuses on several common types of safety aids used to reduce anxiety including: avoidance of situations, avoidance of bodily sensations, use of companions, checking or reassurance seeking, cognitive strategies (e.g., distraction), avoidance of alcohol and other substances, and idiosyncratic safety aids. Jill used numerous safety aids in each of these categories. For example, Jill avoided many situations that increased her anxiety, such as crowded places and being home alone at night, and she avoided unpredictable or potentially dangerous situations (e.g., going to a bar with her friends). By avoiding these places, Jill felt that she could control her anxiety. However, if she was unable to avoid one of these situations, she engaged in the use of additional safety aids to help her cope with her anxiety. For example, if she felt obligated to attend a social event at a bar, she would attend the event for a short period of time and then make an excuse to leave early, or if she needed to go into a crowded place, such as a busy store, she would bring a friend to help ease her anxiety.
Jill also avoided bodily sensations to help reduce her anxiety. As her anxiety worsened, Jill stopped exercising. She no longer played tennis or went running, biking, or swimming because she was afraid an increase in her bodily sensations would induce a panic attack. She also avoided walking briskly or taking the stairs because it would increase her heart rate. By keeping her bodily sensations to a minimum, Jill felt that she was able to prevent a panic attack. She began to attribute an elevation in her bodily sensations as a trigger for her panic and believed that avoiding elevations in these bodily sensations kept her safe from experiencing panic. She also believed that carrying a water bottle would prevent her from getting dehydrated or too hot, which she also thought would protect her from having a panic attack. Her avoidance of bodily sensations and the use of idiosyncratic safety aids (i.e., a water bottle) prevented her from learning that her bodily sensations were not harmful and would not lead to a panic attack.
Jill also frequently engaged in checking behaviors to reduce her anxiety. Jill frequently texted her boyfriend and family to ensure they were okay. Moreover, if she found herself in a situation that required her to be home alone, she would seek reassurance from her boyfriend by sending multiple texts and constantly checking her phone for a response. Being in contact with her boyfriend helped reduce her anxiety because he would reassure her that everything was okay and that help was available if needed. However, engaging in checking and reassurance-seeking behaviors strengthened Jill’s fear of being home alone, thereby preventing her from learning that being alone would not lead to some catastrophic event. Finally, Jill’s avoidance of certain foods, such as raw vegetables, followed a similar pattern. By avoiding particular foods, she felt that she could prevent an allergic reaction.
Most of Jill’s safety aids had a similar theme. Essentially, in her mind, her safety aids kept her safe from potential harm. If she was unable to completely avoid an anxiety-provoking situation, she would engage in the use of other safety aids to help her cope with her anxiety. The extensive use of safety aids resulted in a cyclic pattern of increased dependency on safety aid use to cope with her anxiety. If she was unable to use one particular safety aid, she used another to reduce her anxiety. Thus, Jill’s extensive use of safety aids was a clear maintaining factor in her PDA and GAD diagnoses. Therefore, Jill appeared to be an excellent candidate for the F-SET protocol.
Course of Treatment and Assessment of Progress
Treatment consisted of eight weekly sessions over the course of two months. All treatment sessions lasted 75–90 minutes. The course of treatment focused on providing psychoeducation on the nature of anxiety, discussing the development of true and false fear structures, identifying safety aids used by clients, and developing fading exercises and antiphobic exercises to eliminate the avoidance strategies maintaining clients’ anxiety. The first three sessions of the group F-SET protocol (sessions 1 and 2 in the individual protocol) focus on providing psychoeducation, discussing safety aids, reviewing the antiphobic or phobic attitude, and developing fading and antiphobic exercises. Introducing the key components early in treatment is important to ensure that clients begin to engage in their exercises early in treatment. This is in contrast to many other CBT protocols that tend to introduce treatment concepts in a sequential manner; however, we believe this approach helps with the brevity of F-SET. Sessions 4–8 (sessions 3–5 in the individual protocol) provide therapists with more flexibility in that they can prioritize the discussion of certain safety aids on the basis of clients’ presenting problems. This is especially so when using the individual protocol because therapists can focus on the safety aids most relevant to the client; however, the group treatment is generally administered because of the range of safety aids used by the group members. We next provide a session-by-session overview of the group F-SET protocol.
Overview of Sessions
Pretreatment: diagnostic feedback, treatment goals, and treatment rationale.
The pretreatment session focused on providing diagnostic feedback in which the results of the intake interview and recommendations for treatment were discussed. Because of Jill’s extensive use of safety aids, she was deemed to be an excellent candidate for F-SET. Jill also discussed her primary treatment goals, which included being able to go places alone, engaging in a regular exercise program (e.g., running several times a week) as she did before developing panic attacks, and no longer depending on rigid scheduling to reduce her anxiety.
Session 1: anxiety terminology, fear structures, and safety aid psychoeducation.
Session 1 focused on a discussion of anxiety-related terminology (e.g., stress, anxiety, panic, worry, true and false alarms, anxiety disorders). The emotional processing model (
32) and fear structures were discussed. Specifically, fear structures were defined as memory structures that contain information about fearful stimuli in the environment. Once a fear structure is activated, an individual will have a fear response, resulting in physiological, cognitive, and behavioral responses associated with anxiety. The client is taught that fear structures can be true or false fear structures. True fear structures contain information about truly dangerous stimuli (e.g., being attacked by a bear), whereas false fear structures contain information about perceived threats (e.g., social interaction). The use of safety aids was also discussed, with an emphasis on the role they play in maintaining false fear structures.
Jill discussed her experience of anxiety (i.e., onset, impairment), her primary anxiety-related fear structures, and her common safety behaviors. She was provided with the SBC, to be returned at the next session, and a safety aid monitoring form on which to begin identifying her safety aids.
Session 2: types of fear structures and fading and eliminating safety aids.
Session 2 focused on discussing the types of fear structures relevant to anxiety disorders (i.e., fear of fear, fear of negative evaluation, fear of catastrophic events). The session also reviewed the common types of safety aids (e.g., avoidance of situations) and provided a rationale for fading and eliminating safety aids. The three primary approaches to fading safety aids were also discussed: reducing the frequency of use, reducing the degree of use, and delaying use.
Jill identified fear of fear and fear of catastrophic events as her primary false fear structures. Jill also discussed several safety aids she used that were associated with fear of fear. Specifically, she discussed her avoidance of bodily sensations (e.g., avoidance of exercise), use of checking to monitor her pulse, and carrying a water bottle to keep her from getting hot or feeling dehydrated.
Jill also mentioned safety aids associated with her fear of catastrophic events. Jill frequently checked her phone and texted her boyfriend each night until she fell asleep. To illustrate, Jill spent approximately one hour per night engaging in checking behaviors by constantly rereading and sending texts to her boyfriend and family members to ensure they were okay before going to sleep. She indicated that this was a safety aid she wanted to begin fading as part of her homework for the following week. Jill began decreasing the frequency of use by reducing the amount of time she spent checking her phone. Instead of spending one hour checking her phone, she was instructed to begin her fading by reducing the time allocated to checking her phone to 45 minutes, progressing to 30 minutes, 15 minutes, and so on until she was no longer using her phone as a safety aid. Jill also selected fading the use of a water bottle by reducing the degree of use. Instead of carrying it at all times, she began leaving her water bottle at home or in her car a couple of times a day.
Session 3: antiphobic attitude and antiphobic exercises.
Session 3 centered on discussing the role of phobic behaviors in maintaining anxiety and the importance of having an antiphobic attitude when treating anxiety disorders. Whereas having a phobic attitude involves avoiding stimuli that may trigger a false fear structure, having an antiphobic attitude involves adopting an attitude and behavior that are the opposite of what one has been doing in relation to one’s fears. For example, to combat the fear of looking foolish or being embarrassed, one is encouraged to intentionally do something that is embarrassing, such as tripping and falling in front of others or wearing mismatched clothing.
To develop an antiphobic attitude, Jill was instructed to engage in antiphobic exercises as part of her weekly homework. The use of antiphobic behaviors and the development of antiphobic exercises to challenge Jill’s false fear structures were discussed. Jill was trained in methods to decrease her phobic behaviors while increasing her antiphobic behaviors. We assisted Jill in developing appropriate antiphobic exercises to engage in for the following week. Because one of Jill’s main treatment goals was to overcome her fear of bodily sensations and to resume a regular exercise routine, she began by focusing on her avoidance of bodily sensations. Jill was instructed to run up and down the stairs one to two times a week for approximately 10 minutes each time. Because Jill reported that she would typically stop exercising once she began to feel anxious, she was instructed to combat this anxiety by pushing herself beyond the point at which she would normally want to discontinue exercising. Because Jill indicated that she stopped exercising or reduced the intensity of her exercises after approximately 5 minutes, an initial duration of 10 minutes was selected to ensure she would experience sufficient physiological sensations. In addition, the importance of continuing to exercise once she began feeling anxious was emphasized. Instead of reducing the intensity of her exercising, she was instructed to behave in an antiphobic manner by increasing the intensity of her exercise to help her learn that increasing her psychological sensations would not lead to her feared consequences. Jill also continued to fade her safety behaviors of checking her phone and carrying a water bottle using the same strategies as in session 2. She also began to fade her avoidance of crowded places (e.g., beginning to study in the library during busy times). Because her fear of going places alone without a companion was too great to be a starting point for the fading, Jill was allowed to bring a companion to the library with her. Her use of the companion was faded later in treatment.
Session 4: subtle safety aids and avoidance of bodily sensations.
Session 4 focused on discussions of checking, reassurance seeking, and compulsive behaviors as well as avoidance of bodily sensations as safety aids. Fading exercises and antiphobic exercises were also discussed. The importance of identifying subtle avoidance (e.g., avoiding eye contact or drinking alcohol at social gatherings) in comparison to obvious avoidance (e.g., not attending a social gathering) was highlighted. Jill continued dealing with her avoidance of bodily sensations by exercising for at least 10 minutes per day and reducing the checking of her pulse. Jill began exercising with a companion (i.e., a friend went to the gym with her). The use of companions was faded as treatment progressed (see session 7 for details). Jill also continued to fade her safety aids of checking her phone and carrying her water bottle, and she completed the midtreatment questionnaire battery to assess for symptom change.
Session 5: avoidance of situations.
Session 5 addressed the use of avoidance of situations as a safety aid. The typical methods of avoiding situations were discussed, including not entering a situation because of fear, as were the subtler avoidance strategies of leaving a situation when anxiety arises or not participating fully in a situation. Jill’s fading exercises focused on beginning to fade the avoidance of situations. For her homework, Jill continued to fade her avoidance of crowded places. Instead of studying in the library with her companion as she had over the previous weeks, she was instructed to begin fading the frequency of using her companion. She started fading the companion by going to the library alone each morning when it was not busy. As fading progressed, she started going to the library alone during peak times. First, she did this a few times a week, then she progressed to doing this daily.
Jill also began to fade her avoidance of situations she perceived to be unpredictable or unsafe, such as going to a bar or club with her friends. She started by reducing the frequency of avoiding these situations by going out with her friends. She began going out with her friends once a week and progressed to a couple of times a week. When she did go to a bar, she also tended to make excuses to leave early (i.e., before it got too late), so delaying the use of the safety aid was also targeted. For example, Jill would typically leave the bar after about an hour or if it got too late. Instead of leaving after an hour, she increased the amount of time before leaving the situation (e.g., 90 minutes, two hours) until she no longer left before her friends.
She also continued to engage in her antiphobic exercises of sprinting up and down the stairs. Although Jill was compliant throughout the course of treatment, she tended to have more difficulty with the antiphobic exercises than the fading exercises. We should note that this is not uncommon when using the F-SET protocol; many clients find the antiphobic exercises somewhat unpleasant. When discussing Jill’s assigned antiphobic exercises, it became clear that she was reducing their intensity. Instead of sprinting up and down the stairs, she was walking up and down the stairs. Whereas walking up and down the stairs was a good exercise to begin fading her fear of physiological sensations, the intensity was lower than ideal for an antiphobic exercise. To address this, we reviewed the rationale for the antiphobic exercises, emphasizing the need for the exercise to be extreme, that is, more intense than normal, to fully activate her false fear structures and combat her fear of bodily sensations. Because it seemed as though the initial 10-minute duration of the antiphobic exercise might have been too long for Jill, it was reduced to a few minutes while maintaining the desired intensity. Riding a stationary bike was added to her fading routine as an additional antiphobic exercise to reduce her avoidance of bodily sensations and to boost her progress. At this point in treatment, Jill was successful at increasing the duration of her biking routine from approximately 10 minutes to 25 minutes, but she still tended to avoid increasing the intensity of her cycling by maintaining a moderate level of exertion. To address this, Jill was instructed to incorporate sprints during her biking routine. Specifically, she was told to maintain a sprint for 30–60 seconds at least two to three times each time she rode the bike to address her fear of exercising beyond her comfort zone.
It should be noted that although most clients find the antiphobic exercises easy to implement, it may at times be beneficial to briefly model the antiphobic exercises for clients if they express uncertainty about how to engage in the exercise or if the therapist suspects that a client is not properly completing the exercise. For example, we have found that demonstrating the proper intensity of sprinting up the stairs or creating a role play of how to intentionally say the wrong answer can be helpful if the client is having difficulty performing the exercises.
Session 6: cognitive strategies, companions, and idiosyncratic safety aids.
Session 6 focused on the use of cognitive strategies (e.g., distraction), the use of companions (i.e., presence and absence of companions as safety aids), and the use of idiosyncratic safety aids. Jill’s discussion focused on her use of distraction (e.g., cleaning her house) because her use of companions had been discussed extensively in previous sessions. Jill began fading her use of cognitive strategies by limiting the amount of time she spent cleaning (e.g., 30 minutes). Jill also continued fading her safety aids from the previous weeks. Despite making substantial progress fading the use of her phone at night, Jill was still checking her phone throughout the day. To address her progress in this area, we incorporated a second technique to fade checking her phone—delaying the use of the safety aid. Instead of checking her phone immediately, she was instructed to wait a certain amount of time (i.e., 5 minutes, 10 minutes, 30 minutes) before checking her phone. She also reduced the availability of her phone by keeping it in a room other than the one she was in (e.g., leaving it in the living room at night) or leaving it in her car when she went to class.
Jill continued to engage in her antiphobic exercises, but she continued to struggle with the intensity. Instead of sprinting up the stairs, she would still jog at a slow pace. Because jogging slowly did not reach the intensity desired for an antiphobic exercise, we decided to use this exercise as a fading strategy. However, antiphobic exercises were also incorporated into Jill’s routine by instructing her to increase her pace to a sprint when jogging up and down the stairs for one to two days of the following week to obtain the intensity desired for an antiphobic exercise.
Session 7: medication, alcohol, and other substances.
Session 7 focused on the use (or avoidance) of medications, alcohol, and other substances as safety aids to reduce anxiety. Jill tended to avoid using caffeine because she felt she was very sensitive to the effects of caffeine and feared she would have a panic attack. Fading the avoidance of caffeine was initiated. Jill began fading by incorporating small amounts of caffeine (i.e., one-quarter of a cup of coffee) into her diet. She also continued to fade carrying her water bottle and avoidance of crowded places (e.g., increasing the amount of time spent in crowded places). Jill also began to fade the use of her companions when exercising by going to the gym alone one to two days a week and by exercising in a different location (e.g., a different room) in the gym on days when she went to the gym with her friends.
Session 8: becoming your own therapist and relapse prevention.
The final session focused on relapse prevention, development of a plan for continued fading outside of treatment, and case termination. During the last session, Jill expressed concern about completing treatment because she felt that although her problems with anxiety had improved, she had not eliminated all of her safety aids. A continued safety aid fading plan was developed to ensure Jill would maintain the treatment gains observed during the course of treatment and to ensure continued fading and elimination of the remaining safety aids after treatment was discontinued. The safety aid plan provided a list of the safety aids that Jill would continue fading.
Although Jill had made significant progress fading her safety aids, she had several safety aids that she needed to continue fading after treatment, such as her avoidance of bodily sensations, use of water bottle when exercising, avoidance of dangerous situations, and avoidance of certain foods (e.g., raw vegetables, peanut butter, and caffeine). The safety aid fading plan outlined specific strategies to continue fading and ultimately to eliminate the remaining safety aids. For example, Jill was instructed to continue increasing the duration of her exercise routine until she reached her desired goal of exercising several days a week for approximately 60 minutes on each occasion. Similar instructions were provided for the remaining safety aids to ensure Jill would be able to fade the safety aids on her own.
Complicating Factors
As with any treatment approach, potential complications may occur when using the F-SET protocol. F-SET complications typically emerge during the process of fading safety aids. The therapist should monitor several “fading pitfalls” throughout the course of treatment. Some common complications include having trouble identifying whether a behavior is a safety aid, fading safety aids too quickly, fading some safety aids but not all, and replacing old safety aids with new safety aids. As would any client, Jill engaged in some of the common fading pitfalls, including the tendency to replace faded safety aids with new safety aids and difficulty identifying whether some behaviors were being used as safety aids. To illustrate, Jill’s use of these two common fading pitfalls are described next.
Replacing faded safety aids.
During treatment, Jill tended to fade difficult safety aids (e.g., avoidance of bodily sensations, water bottle) by using other safety aids to reduce the distress she experienced during the fading exercises. For example, when fading her avoidance of crowded places (e.g., studying in the library), she added the use of a companion to help her begin fading this safety aid. She also began to carry her anxiety medication with her as she began to fade the use of the water bottle. Beginning to carry her medication was highlighted as a safety aid that she was using to replace her water bottle. Thus, Jill was assigned to begin fading it (i.e., leave the medication at home), and she was able to fade it the following week. It is important to note that, at times, incorporating new safety aids can be helpful when a client is fading a safety aid that is particularly difficult to fade. When adding new safety aids, it is important for the client to recognize the behavior as a safety aid and work to reduce it as treatment progresses.
This demonstrates the importance of closely monitoring fading exercises to ensure clients are not simply replacing their safety aids with new ones. It is common to observe this pattern because clients with anxiety disorders typically engage in several layers of safety aids. That is, they may tend to use several safety aids at the same time, or they may use several types of safety aids to cope with a particular anxiety-provoking situation (e.g., sometimes checking their phone, sometimes using distraction techniques). As such, it is important to ensure that clients are aware of these safety aids and that each safety aid is faded during the course of treatment.
Ambiguous safety aids and partial fading.
Often, clients engage in behaviors that may or may not be acting as safety aids. To illustrate, Jill kept a water bottle on her person at all times. When initially asked about fading her use of the water bottle, Jill was reluctant to endorse the use of the water bottle as a safety aid, reporting that because she got dehydrated easily, she felt she needed it to keep from becoming dehydrated. In situations in which it is not clear whether something is being used as a safety aid, it is recommended that an individual fade the ambiguous safety aid to test whether it is acting as a safety aid. Once the client’s anxiety disorder has remitted, the client can begin to reinitiate the behavior, as long as it is not being used to reduce anxiety (e.g., carrying a water bottle because of thirst). Over the course of treatment, Jill began to fade the use of her water bottle (e.g., reducing the frequency of use by not bringing it on short trips away from home and leaving it at home on days when her anxiety was lower than usual). Despite making progress, she was still using this safety aid on termination of treatment. For this reason, continued fading of use of the water bottle was identified as a safety aid to continue fading on her own, and a plan was put in place to ensure it would be faded. By the 11-month follow-up assessment, Jill had successfully eliminated the use of a water bottle (i.e., she no longer carried a water bottle) by continuing to fade the frequency of use over the months after treatment ended.
Midtreatment, Posttreatment, and Follow-Up Assessment
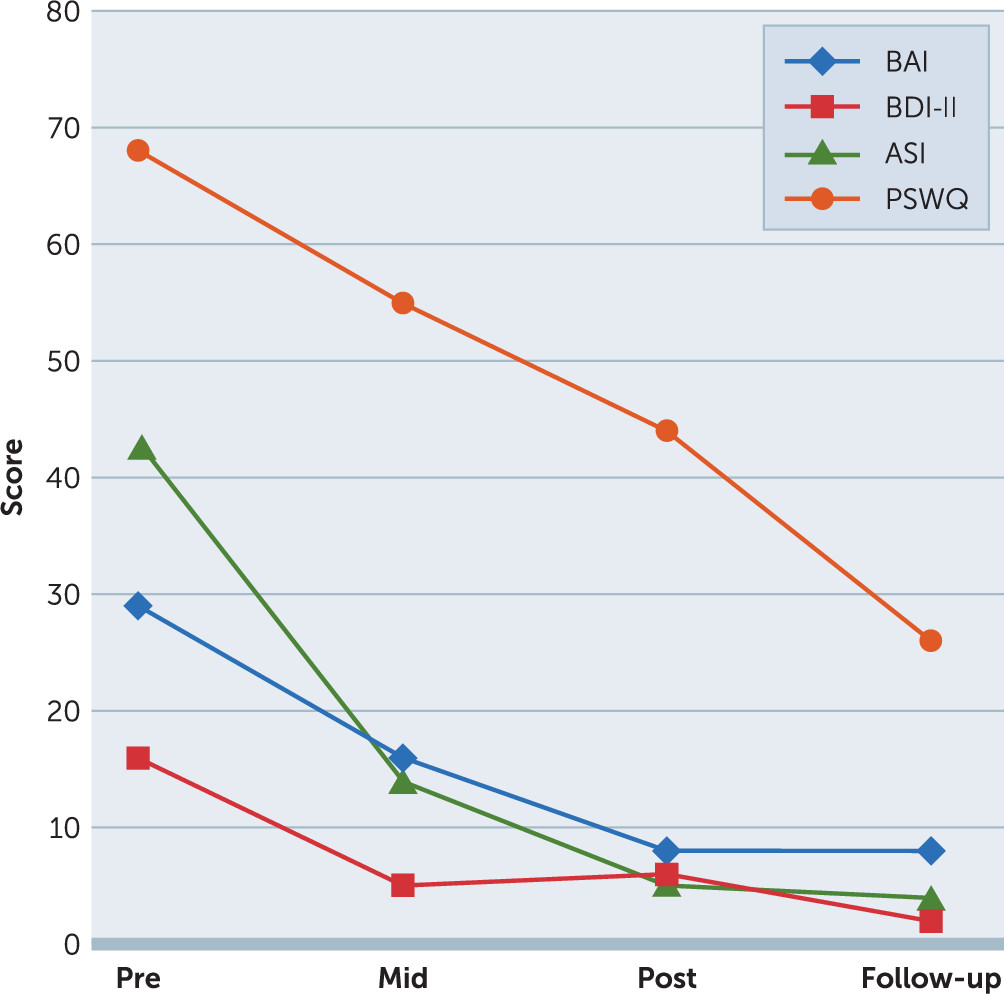
Figure 1 demonstrates the change in symptoms from the baseline assessment to the 11-month follow-up assessment. All self-report measures were administered at each timepoint.
Midtreatment assessment.
During session 4, Jill was administered a battery of self-report questionnaires to assess for changes in symptoms at midtreatment. Jill scored 14 on the ASI, 55 on the PSWQ, 16 on the BAI, and 5 on the BDI-II, indicating a reduction in symptoms at midtreatment.
Posttreatment assessment.
At posttreatment, Jill was administered a battery of self-report questionnaires to assess for changes in symptoms over the course of treatment. Jill scored 5 on the ASI, 44 on the PSWQ, 8 on the BAI, and 6 on the BDI-II, indicating a reduction in symptoms at posttreatment. Despite making substantial progress, Jill was engaging in a number of safety aids at posttreatment. To ensure she continued to make progress outside of treatment, Jill was encouraged to continue fading her safety aids by following the safety aid fading plan that was developed during the last treatment session.
Follow-up assessment.
An 11-month follow-up assessment was conducted. The assessment included administration of the SCID-I/P by an independent evaluator to ensure a nonbiased diagnostic assessment at follow-up, completion of a battery of self-report questionnaires, and an interview with the first author to discuss Jill’s continued use of treatment skills after completing the F-SET treatment protocol. At the 11-month follow-up, Jill no longer met the diagnostic criteria for PDA or GAD. The results from the clinician-administered SCID-I/P assessment were consistent with her scores on the self-report questionnaires. Specifically, Jill scored 4 on the ASI, 26 on the PSWQ, 8 on the BAI, and 2 on the BDI-II (see
Figure 1), demonstrating a clinically significant decrease in scores on these self-report measures. Jill also indicated that she did not receive additional psychological or pharmacological treatment after successfully completing the F-SET treatment.
Change in safety aid use.
Table 1 shows the change in Jill’s safety aid use throughout the course of treatment and at the 11-month follow-up assessment. It should also be noted that it is not uncommon for individuals to become more aware of their safety aids during the initial sessions of treatment. Therefore, it is not unusual for new safety aids to be endorsed during the course of treatment. For example, Jill did not initially endorse the following safety aids: checking blood pressure and pulse, acting overprotective or overcautious, carrying food or a water bottle, relying on a companion for travel, and relying on companions when attending social gatherings. Initially, Jill was not aware that these behaviors were safety aids, but as she learned more about the nature of safety aids, she began to recognize these behaviors as such. Thus, these safety aids were endorsed in the posttreatment administration of the SBC, but not during the baseline administration (after session 1).
Continuation of treatment progress.
During the 11-month follow-up assessment and interview, Jill discussed her continued use of fading and antiphobic exercises to enhance her treatment progress after completion of the eight-session F-SET protocol. After treatment ended, Jill reported that she continued with the safety aid fading plan established during the final F-SET session. It is notable that during this time, Jill used a variety of fading and antiphobic exercises that were not included in the posttreatment continuation plan, and she generalized the fading strategies she used for some safety aids (e.g., chugging a cup of coffee) to other similar safety aids (e.g., eating a large bowl of food that she feared because of a possible allergic reaction). Thus, Jill demonstrated the ability to take what she learned in session and to translate this knowledge into usable strategies to continue her progress despite encountering situations that were not directly addressed during the course of treatment.
After terminating treatment, Jill continued to use the fading strategies to reduce her avoidance of bodily sensations and use of companions. To illustrate, because she found fading her avoidance of bodily sensations particularly difficult, she tended to use several safety aids to engage in exercise. Jill reported that as she became more comfortable with her physiological sensations, she began to reduce the use of the other safety aids as well, by exercising without her companions and fading the use of her water bottle. Instead of taking water with her when she ran, she left it at home. Not only did she fade her use of companions while exercising, but she also generalized her fading of companions to other situations. For instance, she reduced the amount of time she spent with her companions when they went places together (e.g., shopping). Instead of staying with her friend the entire time she was shopping, she began to move to other locations in the store (e.g., the other side of the store), thereby decreasing the degree to which she used her companion as a safety aid. She also began going to places such as the grocery store alone, being at home alone without engaging in phone-checking behaviors, and driving without a companion.
Jill also incorporated antiphobic exercises into her fading exercises. To illustrate, as she faded her use of companions when exercising, she noticed an initial increase in her anxiety while running. To combat this anxiety, she would increase her running pace to a sprint to show herself that she was not going to have a panic attack while running without her companions or water bottle. As Jill faded her avoidance of certain foods, such as raw vegetables and peanut butter, she used antiphobic exercises to combat her fear of having an allergic reaction. For example, instead of having a small amount of the feared food, she would eat a large bowl of raw vegetables or a couple of tablespoons of peanut butter to see whether she could bring on an allergic reaction. Jill reported that these exercises were particularly effective in that she quickly learned that regardless of the quantity she consumed, she did not have the feared allergic reaction. Finally, she also tried chugging a cup of strong coffee to combat her fear of the effects of caffeine on her anxiety. Jill reported engaging in this exercise on one occasion because she is sensitive to caffeine and did not like the effect it had on her. It should be noted that her use of caffeine was particularly challenging and did not change substantially during the course of treatment (see
Table 1).
Finally, when discussing Jill’s improvement in daily functioning, she reported that since treatment her life has changed dramatically. She noted that others have noticed the substantial change in her functioning and have commented on her improvement. When asked how her life has changed from the initial intake session, she reported that her anxiety no longer controls her life, she no longer has a rigid schedule or needs to plan everything, and she feels anxiety free.
Treatment Implications of the Case Study
This case study illustrates the use of the F-SET treatment protocol, which is a transdiagnostic treatment focusing on the identification and elimination of safety aids. This case study also shows the ease with which clients achieve mastery of the F-SET skills and techniques learned in treatment to develop a continuation of treatment through ongoing fading of safety aids and using antiphobic exercises after treatment has been terminated. This feature of the F-SET protocol is important for several reasons. First, the ease with which clients can become proficient in applying treatment techniques without the ongoing supervision of a therapist has direct implications for the cost of treating anxiety disorders, in that clients can enhance and maintain the benefits of treatment without paying for ongoing services. In addition, the continued use of the skills acquired during treatment may help reduce the potential for a relapse. Moreover, the transdiagnostic nature of F-SET provides an attractive treatment approach to treating clients with comorbid anxiety disorders in that therapists can treat more than one disorder at a time. This study illustrates this strength, because the F-SET techniques were effective at concurrently targeting Jill’s panic- and worry-related safety aids. Finally, the F-SET protocol is straightforward and relatively user friendly, making this an ideal treatment to disseminate into the community.
Discussion
The high rates of comorbidity among anxiety disorder patients (
3) suggest the importance of treatment protocols, such as transdiagnostic treatments, that can address multiple disorders concurrently. A clinical approach to treating disorders sequentially can result in a client needing to be in therapy for a longer period of time, and it requires clinicians to master multiple protocols in the treatment of a single client. Therefore, the use of transdiagnostic protocols such as F-SET should be strongly considered when a client presents with comorbid anxiety conditions.
The benefits of the F-SET protocol were evident for Jill. First, fading safety aids is a skill that does not require lengthy practice for mastery. Once the decision has been made by the clinician and client to fade a particular behavior, the client can immediately implement that behavioral change without needing to practice any specific techniques in session. For example, by the end of the second session, Jill began fading her first safety aid (i.e., checking her phone at night). Thus, Jill quickly began using fading strategies and was able to make behavioral changes early in the course of treatment.
Another benefit of F-SET was that because of the protocol’s simplicity, Jill was readily able to successfully continue treatment on her own without the help of a therapist, which resulted in a continued decrease in symptoms, most notably worry (as measured by the PSWQ), after completing treatment. Because of the ease of skill acquisition and ability to see additional gains after termination of formal therapy, F-SET may be of particular utility in situations in which a clinician knows the number of sessions will be limited.
In addition to being easy for the client to master, F-SET is a protocol that clinicians can learn quickly. This provides a great opportunity for clinicians who feel they do not have a great deal of time to dedicate to learning a new protocol. Moreover, students or novice therapists may find F-SET to be a particularly accessible CBT protocol when developing their therapeutic skills.
Finally, when using F-SET, it is important that clinicians take the time to fully understand the nature of their clients’ behaviors, particularly their use of safety aids. The determination of whether a behavior is functioning as a safety aid for a particular client can sometimes be difficult, because individual presentations will vary considerably. In the case of an ambiguous safety aid, the therapist is recommended to encourage the client to fade the behavior and then reintroduce it once symptoms have subsided as long as the behavior is not being performed to reduce anxiety.
As with any investigation, this investigation should be considered in light of its limitations. The single-case design is a key limitation in that we are unable to provide detailed information on more than one client because the data for the other group members completing the treatment were incomplete. As such, the findings of the present study are preliminary. However, this limitation is somewhat diminished by the previous research supporting the F-SET’s efficacy in both group (
11) and individual (
13) formats. Moreover, given that previous work on F-SET has taken place in a community clinic specializing in the treatment of anxiety disorders, it will be important for future work to examine the F-SET in a variety of contexts (e.g., community mental health centers) to demonstrate its efficacy in other settings.
In sum, although there is a need for further research on the F-SET protocol, it appears that F-SET is an efficacious treatment for anxiety disorders that can target comorbid conditions concurrently. Furthermore, the simplicity of the F-SET protocol has numerous benefits for ease of dissemination as well as ease of client skill acquisition.