Adolescents and young adults with chronic health conditions are at increased risk for developing symptoms of depression (
1). In addition to distress and life impairments (
2,
3), depression symptoms can interfere with illness self-management, such as medication adherence (
4). Furthermore, young people experiencing depression often report subsequent reductions in social support (
5), which can be an important buffer against the negative impact of stress on young people with health conditions (
6).
Interpersonal psychotherapy (IPT) is an evidence-based, time-limited treatment for depression (
7). Depressive symptoms are conceptualized within an interpersonal context, and interventions aim to support individuals in navigating their social roles and relationships and accessing support through their social networks to manage psychosocial distress (
8). Individually delivered IPT has been tested several times in populations of adults with chronic illness, with some evidence of efficacy but also feasibility challenges (
9,
10). These results suggest that IPT may be helpful for treating depression among young people with chronic illness, but further research is necessary.
IPT has shown substantial evidence of efficacy among young people. IPT for adolescents (IPT-A) was first adapted for a group format by Mufson et al. (
11). Group therapy may be particularly helpful for young people with chronic illness, because many of these individuals experience frequent health care visits or hospitalizations, stigma regarding their illness, or disruptions to daily life that can interfere with peer socialization (
12–
15). A recent meta-analysis (
16) found IPT-A to be more effective than active control conditions in reducing depression symptoms, with no significant difference found between group and individual IPT-A. These results support the use of IPT with adolescents and young adults, although studies have not yet specifically examined whether IPT leads to symptom reduction among young people with chronic illness.
One of the proposed change mechanisms in IPT is social support (
17). Apart from the IPT literature, several studies (
17,
18) have shown that counseling interventions appear to reduce symptoms by increasing social support. Mediation analyses (
19) have suggested that improvements in family and peer interpersonal functioning partially account for the effect of IPT on remitting depression. More research is needed, however, to understand how social support may change during participation in IPT and may ultimately affect depression symptoms.
IPT has been adapted for many purposes, and although some applications have been unsuccessful, its model of change and therapeutic activities have proven to be flexible, appealing, and efficacious with a wide range of populations and treatment targets (
20). This study aimed to assess the feasibility of offering group IPT for depression to young people with chronic illness and to examine whether depression symptoms decreased and perceived social support increased during treatment. We used a single-arm, open-label feasibility trial approach.
Methods
Sample
Nineteen adolescents and young adults receiving individual psychotherapy at an outpatient behavioral health clinic within Children’s Hospital Los Angeles enrolled in an adjunct IPT group during 2018–2019. Our clinic provides care to a predominantly Latinx population of underserved young people with public health insurance. The clinic is located in a medically underserved area, as defined by the Health Resources and Services Administration, in Los Angeles. Mental health services are funded by a contract with the Los Angeles County Department of Mental Health. Typical treatment includes weekly psychotherapy; when clinically appropriate, psychiatry, case management, group therapy, or other adjunct therapies are offered. The group IPT described in this study was offered within this context as part of the clinicians’ regular responsibilities.
Participants were eligible for this feasibility study if they self-identified as having a chronic health condition and depression symptoms. Chronic illnesses can differ broadly, with a variety of symptoms, symptom severities, levels of medical trauma, comorbid conditions, and medical regimens. However, many young people with chronic illness also experience certain commonalities, such as increased engagement with the health care system and the need for health maintenance behaviors, such as taking medication, following physical activity or dietary restrictions, and coping with symptoms (
21,
22). Moreover, young people with diverse medical diagnoses face similar psychosocial challenges, such as navigating disclosure of their illness to peers and missing school or other age-appropriate activities because of their illness (
13,
14). Seventeen of the 19 group members consented or assented (with parental permission) to participate in a study assessing changes in depression and perceived social support during group treatment. Two group members declined to participate; both reported that they did not like to fill out questionnaires. The study was approved by the Children’s Hospital Los Angeles Institutional Review Board.
Intervention
Four groups were conducted during the study, with two psychologists cofacilitating each group. All group cofacilitators had completed a 2-day training through the IPT Institute, and at least one cofacilitator at each session had community-based certification in IPT. The intervention followed the overall structure presented in the IPT Institute’s handbook for group leaders (
23). This handbook organizes IPT material described in other manuals (
11,
24) into six modules that support clinicians in adhering to IPT’s phased structure (e.g., initial, middle, and conclusion) and in covering each of the IPT problem areas (role transitions, role disputes, interpersonal deficits, and grief).
Before group treatment began, each participant met with one of the group therapists for an individual session to complete an interpersonal inventory and summary. The first group sessions focused on building group cohesion by sharing unique and common experiences of distress, circles of social support, interpersonal summaries, and goals. The second module covered the concept of transitions, with the IPT timeline activity used to increase understanding of associations between events, interpersonal functioning, and social support. The third module focused on disputes, as well as training and practice in active listening and assertive communication skills. During the disputes module, leaders facilitated the “ladder exercise” from the group IPT handbook (
23). For this activity, participants were asked to select an interpersonal problem and then to mark the size of the problem on one image of a ladder and the importance of the relationship on a second image of a ladder. Leaders then facilitated discussion of the problem and relationship in pairs and in the larger group, aiming to support participants’ understanding of how conflicts affected their depression symptoms. The fourth module covered asking for help and problem solving with support. Participants were given structured questions to answer from the group IPT handbook (i.e., what the problem is, what kind of help is needed, who can help, and how to ask for help graciously) (
23). The fifth module was focused on grief and loss, providing participants the opportunity to share narratives of loss and to receive support from and provide support to their peers. Originally, the grief problem area in IPT referred only to the experience of bereavement (
25). However, in the IPT group handbook, this problem area was expanded to encompass a range of experiences, from bereavement to other substantial losses (e.g., parental separation, end of an important relationship, loss of functioning related to a health condition). Participants were given a handout from the handbook (
23) with examples of supportive questions they could ask one another during the process of sharing their grief narrative (e.g., What has the loss been like for you? Who would you like to get support from? How would you like them to support you?). The final module guided the IPT group through review of and reflection on the prior modules and each member’s progress on individual goals, and concluded with a celebration to honor the connections formed during the group treatment. Each session included a range of activities—icebreakers and games promoting group cohesion, pen-and-paper activities conducted in pairs, group brainstorming with a scribe, and role-plays to practice interpersonal skills.
We adapted group IPT in a few ways for our particular population. The number of sessions was increased from the standard 8 to 12 on the basis of the facilitators’ clinical judgment that breaking concepts into smaller pieces would enhance understanding and that repeating concepts would be helpful to our participants, who frequently missed sessions. For example, we would introduce the concept of transitions and complete an example timeline activity during session 3; we would then review the example timeline and facilitate pair discussions of individual timelines during session 4. The review during the second session on transitions was intended to reinforce concepts for those who attended the first session as well as to introduce the topic to participants who had missed the previous session. Other group-based IPT interventions have also used 12-week models (
11,
26). Handouts were reformatted with large fonts to accommodate group members with low vision. In addition, each session was adapted to focus on interpersonal functioning and depression symptoms in the context of living with a chronic illness. For example, when asking about role transitions, the therapists would prompt group members to consider changes related to their chronic illness, such as receiving a new diagnosis or medication or transferring to a new health care provider. Similarly, when covering disputes, clinicians included discussion of disagreements about adhering to medical restrictions or experiences of health-related bullying. Finally, we integrated a few therapeutic art activities to reinforce IPT concepts.
Measures
Participants completed written questionnaires in a group setting, with standing folders to protect their privacy, to assess their demographic characteristics, depression symptoms, and perceived social support. Questionnaires were administered pretreatment (baseline), midtreatment (6 weeks), and immediately posttreatment (12 weeks). Depression symptoms were measured by using the nine-item Patient Health Questionnaire (PHQ-9) (
27), a self-reported instrument covering
DSM criteria for major depressive disorder. Each item consists of a Likert scale, ranging from 0, not at all, to 3, nearly every day. The PHQ-9 has demonstrated rigorous reliability and validity (
27,
28) and has adequate psychometric properties to assess treatment response (
29). Social support was assessed by using the Social Provisions Scale (SPS) (
30). SPS scores have been associated with depression in samples with medical illness (
31). Reliability and validity of this measure were originally established by Cutrona and Russell in 1987 (
30) and have been confirmed in more recent adult samples (
31).
Analytic Plan
We used generalized estimating equation (GEE) models that were based on linear regression to evaluate PHQ and SPS scores across the entire study period (pretreatment, midtreatment, and posttreatment time points), with analyses adjusted for repeated measures. We followed intention-to-treat principles and included all available data from the participants, and we evaluated whether depression symptoms decreased and whether social support increased from pretreatment to midtreatment and from pretreatment to posttreatment. The significance level was set at 5%, with a two-sided test. All statistical computations were performed with Stata/SE, version 15.1.
Results
Participants had a mean±SD age of 18.12±1.27 years (range 16–20 years). Most (65%, N=11) participants identified as cisgender female, 18% (N=3) identified as cisgender male, and 18% (N=3) identified as transgender or nonbinary. The sample was predominantly Latinx (82%, N=14), and participants identified their race as other (70%, N=12), Black (12%, N=2), Native American (12%, N=2), and multiracial (6%, N=1). Participants had a wide range of chronic conditions, including solid organ transplants, rheumatic disease, cancer, spina bifida, fatty liver disease, fibromyalgia, chronic lung disease, and hyperlipidemia.
Deidentified Clinical Examples
During our pilot study, group members often expressed their appreciation for the opportunity to talk with peers who understood the unique social challenges (e.g., stigma, hesitancy to disclose illness to peers, feeling left out of typical adolescent activities, end-of-life concerns) experienced by young people with chronic health conditions. Below we share deidentified clinical material for each of the four IPT problem areas.
Role transitions.
Group members discussed many role transitions that had affected their mental health and interpersonal functioning, including many that are common among young people regardless of health status, such as graduation from high school, changes in family structure, or the end of friendships or romantic relationships. They also shared difficult changes related to living with a chronic illness, such as being expected to manage their condition more independently, adjusting to a new medication or dietary restriction, or transitioning from pediatric to adult subspecialty care. For example, in one cohort, a group member reported feeling sad and stressed about saying goodbye to the rheumatologist who had cared for them since they were a baby as they prepared to transition to the adult health care system. Other group members validated this peer’s experience, sharing how they had struggled with identical or similar goodbyes (e.g., when a trusted nephrologist retired or when a pediatrician graduated a fellowship and left the training hospital). Group members provided emotional support by listening, displaying empathy, and communicating positive expectations that the peers who were beginning the goodbye process would be able to cope well and to potentially forge similar connections with future providers. During this module, we incorporated a therapeutic art activity illustrating a transition, in which the participants completed a drawing of a bridge over a river. This art activity provided an opportunity to reinforce concepts from the IPT timeline activity by supporting participants in expressing how interpersonal barriers or support influenced their experience of a transition. For example, one participant drew a choppy, swirling river, labeling portions with the difficult interpersonal aspects of the experience (e.g., being bullied, ignored, and disappointed), and a treacherous rope bridge, showing how hard it was for them to get through a life change.
Role disputes.
Group members discussed how conflict with others in their lives affected their mood and influenced their depression symptoms. They described common disagreements with peers, teachers, siblings, and parents, as well as many disputes that were specifically related to their chronic illness. Many group participants shared with each other disputes they had had with their parents and health care providers about medication adherence, health-related restrictions, and the desire for more independence. For example, one cohort of participants found common ground in their struggles with what they perceived as overprotective parents. A young woman who used a wheelchair described how hopeless she felt about her future, because her mother felt it was unsafe for her to take the bus alone in light of her mobility difficulties. Several participants described similar experiences of not being allowed to go to a park or a friend’s house because of parents who worried they would experience a health complication without anyone knowledgeable about their condition nearby. Together, the group members expressed relief at realizing they were not alone in going through these disputes, and they gave one another suggestions for possible compromises or safety precautions to be used in negotiations with parents.
Interpersonal deficits.
For many group members, chronic illness had interfered with their school attendance or peer socialization for large parts of their childhood or adolescence. In some cases, they had experienced medical trauma, bullying, or neglect by peers, which had led them to feel less confident about their social skills and their ability to connect with others. For example, a young woman shared that she would not be able to attend Senior Day at a local amusement park with her graduating class because her chronic illness would cause fatigue and pain if she had to be on her feet in the sun all day. She described how she felt depressed and that this was another reminder of how she was not “normal” and “would never make friends.” Her peers in the group quickly pushed back, encouraging her not to give up on attending if she wanted to experience this celebration. After conversation with her peers, completion of the interpersonal problem-solving activity, and a role-play of asking her principal for accommodations, she expressed readiness to advocate for her needs. Her ultimate success in attending Senior Day also helped to build the group’s collective confidence in assertively asking for what they needed.
Grief and loss.
Group members described a range of grief and loss experiences related to their chronic illnesses and independent of their health status. Clients in our clinic are often highly affected by trauma, and several participants in our groups had experienced parental loss or abuse. Grief experiences related to chronic illness included loss of physical and cognitive functioning, receiving diagnoses of serious or progressive diseases, and a feeling of “lost time” or “lost childhood.” In one cohort, two group members connected about having impaired cognitive functioning related to central nervous system insults. They shared how difficult it was to experience a loss of language and memory skills and received support and empathy from group members as they shared their stories.
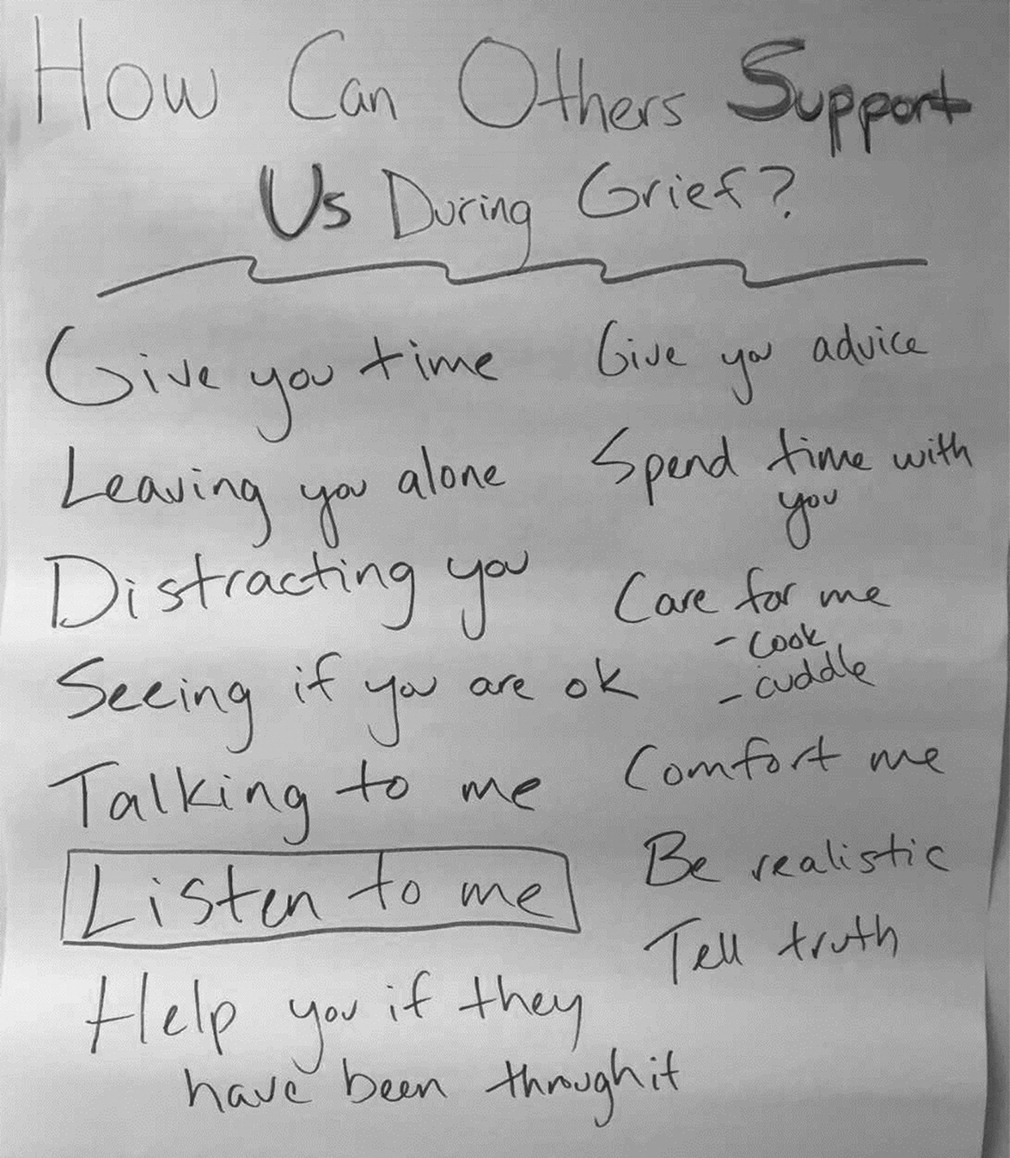
Figure 1 illustrates a group brainstorming activity from this module, in which a scribe recorded group members’ ideas about which types of support they would appreciate during times of grief.
Evidence of Feasibility
Participants attended an average of 6.12±3.20 sessions. The means and standard deviations for depression symptoms and for perceived social support at each study time point are reported in
Table 1. No significant baseline differences were found in depression symptoms or perceived social support between group completers (N=13) and noncompleters (N=4). One noncompleter was unable to finish the group therapy because of severe health problems, another moved out of the city, and the remaining two did not report reasons for dropping out. Among those who completed the group treatment, participants attended an average of 7.69±1.44 of the 12 sessions.
Preliminary Results of the Self-Reported Data
GEE modeling showed no significant decrease in PHQ-9 scores at 6 weeks compared with baseline, but a significant decrease in PHQ-9 scores was evident at 12 weeks compared with baseline (β=−2.94, 95% CI=−5.30 to −0.59, p=0.014). For perceived social support, GEE modeling showed a slight but statistically insignificant increase in SPS scores at 6 weeks compared with baseline, but the increase in SPS scores was statistically significant at 12 weeks compared with baseline (β=4.24, 95% CI=0.51 to 7.98, p=0.026).
Discussion
The evidence for the feasibility of group IPT for young people with chronic illness and depression symptoms was mixed. On one hand, most participants were able to complete the treatment. In fact, only 24% (N=4) of group members dropped out of the study, about half the dropout rate reported in Blanco and colleagues’ (
10) trial of individual IPT for women with breast cancer. On the other hand, participants missed about half of the sessions, indicating that they faced barriers to full engagement in the therapy. The deidentified clinical examples illustrated how the IPT interventions were often a good fit for the interpersonal problems our participants experienced. Exploratory GEE results showed that PHQ-9 scores decreased significantly over the course of the 12-week treatment, indicating a shift from moderate depression to mild depression on average. Furthermore, young people in our study reported that their social support significantly increased during their participation in group IPT. However, because of the lack of a control group, we could not conclude that group IPT caused the changes in depression and social support. The improvements may have resulted from participation in any type of group, from the concurrent individual therapy sessions, or from natural symptom improvement over time.
Review of the content of each module during two sessions was an important adaptation in this feasibility study, because it provided group members with a second chance to learn about and apply interpersonal concepts they may have missed, as well as the opportunity to further encode group interventions after processing information for a second time. This repetition was especially necessary because, on average, participants attended only half the sessions. Furthermore, several participants had cognitive symptoms related to their chronic illness, and repeated exposure to concepts may have improved their understanding and retention of the material. The low attendance rate observed in our study suggested that group IPT has some feasibility challenges for use among young people with chronic illness. Absences were often related to medical appointments or worsened pain, fatigue, or other illness symptoms. The expansion of telehealth services via videoconferencing technologies (
32,
33) may enhance the feasibility of delivering therapies such as IPT to people with chronic illness (
34). For example, Donnelly et al. (
35), in a single-arm pilot study, reported high feasibility for delivering IPT by telephone to patients undergoing cancer treatment. Facilitating IPT groups via telehealth could be appropriate for young people with infectious diseases or compromised immune systems who may be unable to attend services in person. In addition, asynchronous IPT groups, such as secure online forums patients can log into when they have time to do so and are feeling well, may increase feasibility. Furthermore, although group therapy may help young people with chronic illness to feel a sense of belonging and less socially isolated, one-on-one IPT sessions tailored to individual needs may be easier to schedule. Future research should investigate the efficacy of IPT within various settings to optimize use of tailored treatments and to reduce barriers to engagement in evidence-based behavioral health services for young people with chronic health conditions.
The results of this feasibility study highlighted the potential benefit of offering IPT groups within pediatric hospitals or subspecialty health care settings. IPT groups may fit appropriately within comprehensive, integrated care models involving universal screening and referral to treatment, such as the tiered model proposed by Schwartz and Feudtner (
4). IPT–Adolescent Skills Training (IPT-AST) has already been adapted as an indicated prevention program for young people with elevated depression symptoms in academic settings (
36). Evidence exists that IPT-AST can significantly reduce depression symptoms and improve overall functioning for young people at risk for major depressive disorder (
37,
38), although preventive effects have not been detected at 12-month follow-up (
37,
38). Taking this mixed evidence into account, it could be helpful to integrate IPT into the pediatric hospital setting. Although the impact may be time limited, young people with chronic illness often miss more school days than their peers without illness and, therefore, may miss out on social-emotional programming similar to IPT-AST that may be provided in schools (
12). Recent work by Mufson and colleagues (
39) suggested that delivering IPT in pediatric primary care clinics was feasible, acceptable, and potentially beneficial for a sample of urban Latinx adolescents. Intervention researchers may consider extending this model to the subspecialty health care setting, because young people who need these services likely experience depressive symptoms at even higher rates and have more frequent contact with health care providers compared with young people receiving care in different settings.
Although social support was not tested as a mediator in the current study because of the single-arm design and small sample size, the findings that depression symptoms decreased and perceived social support increased through participation in group IPT suggest that future researchers should test social support as a mechanism of change. In addition, future research investigating how, for whom, and when interventions such as IPT work would improve the practitioner’s tool kit in settings such as pediatric hospitals and community mental health agencies. Future qualitative studies with young people participating in group IPT would be helpful for clarifying how well this treatment model fits this population’s needs and experiences. Further research should also investigate the efficacy of group IPT for this population in various settings in order to optimize tailored treatments and to reduce barriers to engagement in evidence-based therapy.
Finally, although this pilot study was limited in size and scope, characteristics of the enrolled sample differed from those reported in prior published research. Therefore, the data reported in this article have added to the body of empirical literature on IPT. For example, several IPT trials with Latinx young people in New York or Puerto Rico have been published, but our pilot study enrolled a Latinx population in Los Angeles. Latinx young people are diverse, and each regional community has a unique composition of national origin, ethnic and racial heritage, cultural influences, and sociopolitical context. In addition, trials of IPT with adult sample populations with chronic illness have been published, but, to our knowledge, none have been conducted with young people with chronic health conditions. The experience of living with a chronic illness during adolescence or young adulthood may result in different interpersonal difficulties (e.g., with achieving independence or experiencing school bullying) than such an experience during adulthood. For these reasons, our data have contributed to the broader IPT literature.
These results should be considered in relation to the study’s limitations. First, this study enrolled a small sample size, which reduced statistical power and generalizability. Second, the study’s analyses did not rule out the potential impacts of cohort effects on the results. Third, the impacts of IPT on social support and depression were unclear because this study did not include a control group and because all participants were receiving individual psychotherapy. Finally, depression and social support were only measured during participation in group IPT, making it impossible to test for the persistence of changes following completion of group treatment.
Conclusions
This article described our process for selecting, adapting, and implementing group-based IPT with a sample of young people with chronic illness. By using GEE analyses, we found that depression symptoms significantly decreased and that perceived social support significantly increased by the end of treatment. However, session attendance was low, indicating feasibility challenges. Additional inquiry would be beneficial to further determine the efficacy of group-based IPT within various clinical settings (e.g., integrated health care, academic hospital, telehealth) to best address the mental health needs of young people with chronic illness.