In the last decade, exposure-based therapies, such as prolonged exposure (PE) (
1), have been recognized as the first-line treatment for posttraumatic stress disorder (PTSD) (
2). One goal of PE is reactivation of the pathological fear structure to facilitate extinction of fear-inducing stimuli through repeated exposure and corrective emotional processing of the trauma memory (
3). Subjective units of distress, a self-reported measure of general psychological distress, are collected at regular intervals throughout exposure sessions and have typically been used to assess elements of emotional processing, including fear activation, emotional engagement, and extinction within and between sessions (
1). Reliance on subjective units of distress is a practical approach, but it may fail to capture changes for clients who may be avoidant or less attuned to their emotional states. Recently, the growing availability of mobile health technologies has made objective measurement of physiological responses during therapy sessions possible. Use of these technologies enables examination of the psychotherapy processes contributing to therapeutic outcomes. Researchers have started to examine physiology in the context of exposure treatment to assess aspects of treatment response. These studies have primarily relied on pre-post analyses (
4) and have found increased psychophysiological reactivity to trauma cues, as well as changes from pre- to posttreatment in heart rate (HR) reactivity to trauma cues, to be associated with treatment response (
5).
Unfortunately, when these technologies have been integrated into PE treatment studies, analytical approaches have differed. As these technologies proliferate, the adoption of consistent analytical approaches will help to ensure meaningful cross-study comparisons and data interpretation, as well as integration with other psychophysiological modalities.
A key component of exposure-based therapies is emotional engagement with the trauma memory, defined as activation of a distress reaction during the exposure procedures (
6). Although historically focused on fear (
1), other strong emotional experiences, particularly anger, shame, guilt, and sadness, contribute to trauma reactions (
7). PE is based on the emotional processing theory (EPT), which posits that emotional engagement is integral to activation and modification of the pathological emotion structure (
8). This central tenet of EPT has mostly been subjectively examined. Historically, subjective engagement has been assessed by using peak subjective units of distress from the first and last imaginal exposure sessions (
9), or by using the change from each session’s baseline rating of subjective units of distress to the peak rating within each session, averaged across sessions for overall treatment analysis (
10). We would expect some correlation between physiological measures of distress and subjective units of distress in an emotionally aware individual—particularly when the individual accesses high-arousal emotions (e.g., fear, anxiety, and anger). During PE, when the individual is accessing emotions tied to the trauma memory, we would expect a high correlation between a measure of arousal (e.g., HR) and subjective units of distress. Indeed, in a recent effort to examine emotional engagement by using ambulatory physiological measures, we (
11) calculated correlations between subjective units of distress, HR, and electrodermal activity to assess concordance between objective and subjective emotional engagement during imaginal PE therapy sessions. That study found high concordance between measures during therapist-identified pivotal sessions, in which the patient made the greatest therapeutic gains.
Whereas emotional engagement may be defined as emotion activation throughout the session, another key component in PE is initial emotion activation. Initial emotion activation is defined as the highest level of distress during the first imaginal exposure and theoretically represents activation of the traumatic emotional response during the initial therapeutic exposure. Conceptual and operational ambiguity between initial activation and emotional engagement has unfortunately led to mixed findings in the literature. For example, Cooper et al. (
6) reviewed evidence for emotional engagement but included initial emotion activation operationalized as peak subjective units of distress, changes from baseline to peak distress during the first imaginal exposure only (
12–
14), and changes in distress across sessions (
9,
10) as part of the same construct. Another study (
15) examined physiological reactivity during written exposure therapy and found that high fear activation during the first session predicted greater decreases in PTSD symptoms posttreatment. In that study, fear activation was calculated as time from start of exposure to peak HR, identified by using continuously collected interbeat interval data. Separating these constructs with a specific analytical roadmap will help the field better operationalize and understand the process and importance of emotion activation during PE and other exposure therapies.
Finally, according to EPT, extinction (originally referred to as “habituation”) represents a reduction in reactivity after repeated exposure to the threatening stimulus (
3). Neuroscience models suggest that PE habituation processes align with fear extinction processes (
16), in which there is a reduction in the emotional response over time. In the context of PE, the threatening stimulus during imaginal exposure procedures is the trauma memory, to which the client is meant to extinguish his or her emotional response. Prior studies operationalized extinction, both within and between sessions, generally as a decrease in subjective units of distress. The most common operationalization for within-session extinction is the change from peak subjective units of distress to last rating of subjective units of distress in a given session (
6). Between-session extinction has been operationalized as the change in peak subjective units of distress across sessions (
17), change in mean subjective units of distress from first to last exposure session (
18), or, when HR measures were examined (
13), a general linear regression suggesting decreased distress responses across therapeutic sessions. Although each approach has merit, variability in the operationalization of extinction has hindered an understanding of PE treatment response mechanisms (
6).
In summary, although there have been some attempts to integrate HR and other physiological measures of distress into psychotherapy, these approaches have not yet been widely used during PE or other trauma therapies. As interest and availability of mobile health technologies grow, clarity and guidance in data analytic approaches will be needed. These tools provide an avenue not only to better understanding the mechanisms and processes underlying trauma therapies, such as PE, but also to identifying and better treating individuals who struggle to engage with trauma therapy. A guide to analyzing the data produced by these tools will not only ensure that clinical studies are comparable and comprehensible, but also enable the field to build a foundation on which studies and methods can be replicated both in academic and clinical environments. Our aim was to examine three approaches to analyzing data collected via mobile health technologies during PE. Specifically, here we provide explanations and examples of how to analyze continuously collected psychophysiological data in each EPT domain: emotional engagement, initial emotion activation, and within- and between-session extinction during clinic-based PE. Furthermore, we discuss relevant scientific questions, the conclusions that may be drawn, and the benefits and limitations of each approach.
Methods
Participants
Data from three participants from a pilot study examining physiological reactivity during PE therapy were examined. The study was approved by the University of California, San Francisco, Institutional Review Board, and the data were collected between July 8, 2018, and August 20, 2019. All participants provided written informed consent. All three participants were male veterans who self-identified as non-Hispanic White and had been deployed during conflict eras. Participants A (age 70) and B (age 75) served during the Vietnam era, and participant C (age 33) served during the 9/11 era. Participant A was prescribed naltrexone, trazodone, and venlafaxine; participant B was prescribed duloxetine; and participant C was not prescribed any psychiatric medications. Participants A and C were combat veterans, whereas participant B was deployed on aircraft carriers. Each participant had a qualitatively different traumatic event, given differences in age, combat theater, and time since the trauma occurred. We expected the two older participants to have less malleable traumatic associations because of the longer time since the trauma occurred. All three participants reported moderate to moderately severe PTSD and depression symptoms during their PTSD evaluations. Participants completed a clinical interview, which included questions from the Clinician-Administered PTSD Scale for DSM-IV (
19), but did not complete a formal assessment before starting treatment. In line with the descriptions provided in the PE manual (
1), participant A reported distress in a manner suggesting extremely low distress tolerance (i.e., an overengager) and did not respond to treatment. Participant B underreported distress in a manner suggesting emotional numbing or disconnection (i.e., an underengager) and responded to treatment. Participant C was well engaged and partially responded to treatment. These engagement patterns may have been a byproduct of the time since the trauma had occurred and may have affected the consolidation and reconsolidation process during PE. Specifically, the two older veterans likely experienced entrenched traumatic associations and avoidance patterns, which may have contributed to their difficulty engaging in PE.
Procedure
Participants undergoing PE in a U.S. Department of Veterans Affairs (VA) PTSD treatment clinic were recruited for participation into the VA Mobile Health Study, which aimed to examine objective ambulatory physiological monitoring during sessions of leading evidence-based PTSD treatments that use exposure protocols. Eligibility criteria included a PTSD diagnosis, as determined by clinical intake procedures for a VA PTSD treatment clinic, and agreement to not receive other psychotherapy or PTSD treatment during the study and to allow digital recording of audio and psychophysiology data (i.e., HR) during therapy sessions. Beginning at the initial session of PE, participants wore the Empatica E4 (
20), a research-grade activity tracker wristband, to capture physiological reactivity. All participants completed the standard PE protocol, although participant B’s treatment included the addition of external stimuli to enhance engagement (
11).
Physiological Recordings
The Empatica E4 wristband has four embedded sensors to record physiological responses: an electrodermal activity (EDA) measure for skin conductance, a photoplethysmography sensor to measure HR via blood volume pulse, a temperature sensor for skin temperature measurement, and a three-axis accelerometer for movement measurement. For the present analyses, only the HR measurements were used as proxies for the autonomic nervous system. Although EDA is a common measure of arousal, recent independent studies (
21,
22) have suggested that the E4 does not produce reliable EDA data, thus EDA is not presented here. The procedures outlined here, however, can also be applied to continuously collected EDA. HR is a frequently used noninvasive measure of autonomic nervous system activity, in which individuals with PTSD have demonstrated dysregulation (
23). HR data acquisition followed standard guidelines and used Empatica E4–suggested placement, recording, and data processing procedures (
20). HR was sampled at 1 Hz, with values given at every second during the recording period.
Data Processing
Prior to conducting all planned analyses, HR was binned into 10-second intervals by computing continuous averages of every 10 seconds, in order to reduce the unexplained variation across measurements. Only data occurring during the imaginal portion of the session (disregarding pre- and postimaginal exposure data) were evaluated to enhance comparability between approaches. Statistical analyses of emotional engagement and initial emotion activation were performed by using R, version 2.1 (
24). Extinction statistical analyses were performed by using the “nlme” package (
25) in R, version 3.6 (
24).
Results
Approach 1: Emotional Engagement
Statistical analysis for emotional engagement.
To assess emotional engagement, as indicated in the classic PE protocol, therapists wrote down the time at which they asked a participant for a rating of subjective units of distress. These timestamps, based on the therapists’ personal watches, were used as event markers when examining HR data. The mean HR value for the 60 seconds prior to the rating was extracted for each distress rating taken during the PE sessions. This time frame was chosen because participants were asked to rate their distress for the moment prior to being asked about it. As noted in the original PE protocol (
1), asking a participant to provide a distress rating can be distracting and affect their emotional state during exposures—for example, the manual (
1) encourages eliciting fewer ratings during the first telling of the narrative to avoid bringing the participant in and out of the exposure with questions. Furthermore, this range of time provides some correction for external clock time measurement errors (e.g., if a therapist’s watch was a few seconds off from the Unix timestamp used by Empatica). Bivariate correlations were then computed to compare distress ratings with mean HR from the 60 seconds prior to the rating as a measure of concordance between the subjective distress ratings and objective measures of distress (i.e., HR) during the imaginal exposure procedures. Pearson’s correlation coefficient (r) was then examined across sessions to identify sessions with high or low levels of concordance, as well as changes in concordance throughout treatment. Participant C was not included in the present analysis because he reported the same distress level throughout most sessions (i.e., exhibited no variability), and bivariate correlation analyses cannot be performed without variability within the data.
Potential benefits and limitations of the emotional engagement approach.
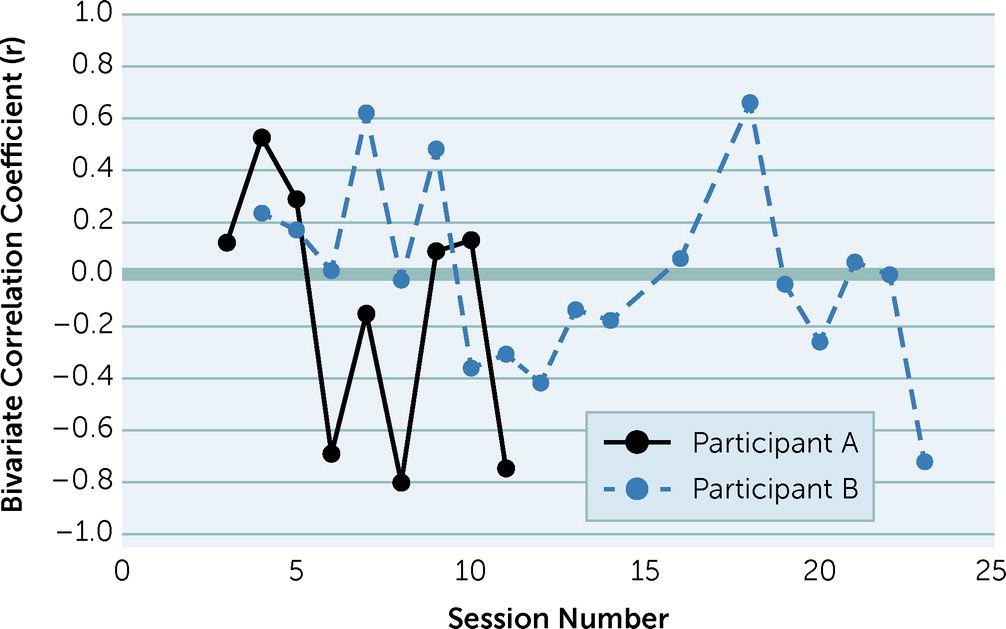
Figure 1 displays the Pearson’s correlation coefficient for each session over time, indicating whether participants increased their concordance between HR and subjective units of distress during treatment. Sessions with high concordance between HR and distress units included participant A’s session 4 (r=0.53, df=9, p=0.09) and participant B’s sessions 7 (r=0.62, df=6, p=0.10) and 9 (r=0.48, df=24, p=0.01). Notably, these sessions were also identified by therapists as pivotal sessions. Therapists defined pivotal sessions as those in which the participant demonstrated increased insight into trauma reaction and reported subjective units of distress that aligned with the therapists’ clinical judgment of the participant’s distress. Therapists identified and documented these sessions prior to any psychophysiological data processing or analysis. For participant A, the therapist documented that during session 4, the participant discussed holding back emotionally, used more emotional words during his trauma narrative, and, by the final retelling, named specific emotions. For participant B, session 7 involved the integration of two auditory cues to augment emotional engagement during the imaginal exposure. These auditory cues consisted of the alarms that sounded at the beginning of the traumatic event and were introduced after both the therapist and the participant agreed that he was struggling to access his emotions during imaginal exposures A full description of this case is available elsewhere (
11).
The level of concordance, or discordance, between subjective and objective measures of distress provides a metric of how aware a person is of their own distress. Within our small sample of male veterans, low concordance was common at treatment outset. This finding was congruent with the common need to provide psychoeducation about emotional experiences at the outset of PTSD therapies, including PE and cognitive processing therapy. Examining emotional engagement during PE may provide insight into emotional processing within and between sessions (
11). Participants A and B both demonstrated the greatest concordance during sessions in which their therapists noticed changes in their emotional engagement. Within-session concordance between self-reported and objectively measured distress could become a specific therapy goal, and between-session concordance could be used as a treatment outcome—particularly if combined with measures of emotional awareness. One potential metric of between-session concordance could be change in concordance from the first session to the last session (for participant A, this would be −0.87, and for participant B this would be −0.96, demonstrating that for both participants, concordance in the final session was less than that in the initial session). Another metric could be change in concordance from the first session to the peak session (for participant A, this would be 0.40, and for participant B this would be 0.42). Either of these measures might provide insight into whether concordance improves during treatment or is an indication of therapeutically important sessions.
Importantly, as demonstrated by participant C, this approach is limited when participants lack variability in their reported distress level. Despite this limitation, clinicians examining psychophysiological reactivity during PE may use concordance as a way to objectively assess cognitive awareness of emotional engagement during exposure procedures. That is, concordance provides a measure of avoidance, suppression, and possibly emotional numbing during exposure, particularly with individuals who are over- or underengaged. With specific knowledge regarding the discordance between subjective units of distress and physiological reactivity, the clinician may be able to adjust therapy procedures to increase engagement by integrating trauma-specific external stimuli (e.g., sounds, sights, smells) into the session. The level of concordance could also be used as a sign that the participant may be reporting greater emotional distress than is physiologically expressed—illuminating potential physiological blunting, overengagement, or extreme discomfort with emotional experiences. This discordance between HR (and other physiological measures) and self-reported distress may signal the need to reiterate psychoeducation regarding the normalcy of emotional experiences and expressions to further facilitate emotional awareness, comfort with experiencing negative emotions, and self-efficacy in coping with strong emotional experiences. As such, this analytic approach may be most helpful for clients who lack emotional awareness, experience emotional numbing, or have alexithymia. Furthermore, many mobile physiological devices offer real-time assessment of biomarkers such as HR. One advantage of this procedure is that, like those used in biofeedback (
26), a therapist may be able to observe clients’ physiological responses during sessions to gain an understanding of clients’ emotional engagement with the trauma memory and awareness of their own distress.
Mechanistically, a measure of emotional engagement concordance provides an opportunity to compare pivotal clinical sessions to other sessions to gain a greater understanding of treatment response and gains. For example, therapists could elicit distress ratings throughout the entire therapy session (a minimal protocol change) and use concordance to compare the specific contributions of psychoeducation, imaginal exposure, and processing procedures. Furthermore, as a specific measure of emotional engagement throughout treatment, concordance provides an avenue to elucidate the integration and understanding of emotional processes over time. For example, concordance may be used to differentiate the effects of processing specific trauma-related emotions (e.g., fear, disgust, shame, and guilt), some of which do not fit in the traditional fear-extinction model of PTSD treatment because of low physiological activation. Thus, examining emotional engagement during PE via concordance could help integrate affective science theories into the clinic, with the goal of facilitating greater understanding of PTSD and its treatment. Finally, because concordance can be measured repeatedly over the course of treatment, it can be examined as a predictor of early response, change throughout treatment, and pre-post outcomes by administering a weekly PTSD symptom measure. Each of these outcome analyses would expand the field’s understanding of, and ability to effectively treat, PTSD.
Approach 2: Initial Emotion Activation
Statistical analysis for initial emotion activation.
To assess initial emotion activation, the binned HR values from the participants’ first imaginal exposure (session 3 for participants A and C and session 4 for participant B) were examined. Because participant B participated in imaginal exposures to a second trauma, the first imaginal exposure to that trauma was also analyzed separately (session 16). Maximum values of HR and subjective units of distress were extracted, along with corresponding time (in minutes), for each measure from the start of each imaginal exposure, in line with published procedures (
15). Importantly, although the therapists largely asked for distress ratings every 5 minutes, as indicated in the protocol, participants’ first narratives were purposely not interrupted for distress ratings, as suggested in the protocol, to ensure that participants completed one full narrative. Thus, particularly during the first imaginal exposure session, distress ratings were not evenly spaced over time.
Potential benefits and limitations of the initial emotion activation approach.
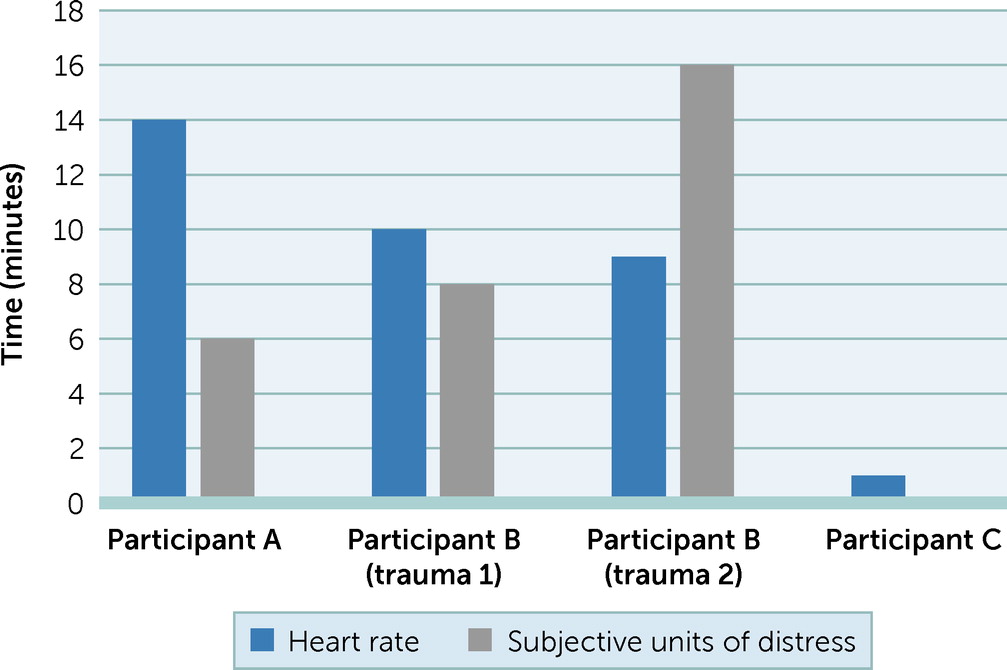
Results for initial emotion activation indicated that time to reach peak HR ranged from 1 to 14 minutes, whereas time to reach peak subjective units of distress ranged from 0 to 16 minutes (see
Figure 2). The difference in time to peak reactivity between self-reported distress units and HR suggested that these measures did not always correspond. This result was particularly striking, because we expected these measures to at least be close in time, if not similar in activation. The difference between peak distress ratings and peak HR suggested lower subjective distress thresholds among our sample, or perhaps some parasympathetic influence when working to answer the distress-level prompt. As such, one measure may be more predictive of treatment outcome than the other.
Initial emotion activation provided a measure of engagement during the first exposure to the trauma memory. This measure is particularly relevant for EPT (
3), because reactivating the emotion structure is the first step in memory reconsolidation and integration. Previously examined via subjective units of distress (
12–
14) and HR (
15), this measure provides an observable datapoint of how quickly someone emotionally engages with the trauma memory. Furthermore, although participant C’s consistent report of a single distress level throughout the session inhibited emotional engagement concordance analyses, the initial emotion activation analysis presented a slightly different picture. Although this participant did not report changes in distress, he did demonstrate HR changes, including discordance between his peak reported distress and his peak HR. Participant C demonstrated how reliance on subjective units of distress alone may miss capturing initial emotion activation during PE treatment.
Previous studies have examined fear response specifically in the initial exposure session (as presented here); however, the same analytical approach applied across sessions may be able to provide a measure to determine in which treatment session emotion activation first occurs. That is, applying this measure across sessions may provide insight into when a participant first engages with a trauma memory—rather than only a measurement of whether or not engagement occurred during the first imaginary exposure session. Such a measure would allow for comparisons between individuals and would provide an understanding of the relationship between emotion structure activation, length of treatment, and treatment outcomes. Notably, this expansion of the measure would allow for comparisons between those quick and slow to approach the emotion structure and between different levels of activation, and it would indicate individuals who never activate it. Each of these avenues may provide valuable data for how to increase engagement in PE as well as for whom PE is the best trauma-focused therapy option.
When applied to the first exposure session only, measurement of initial emotion activation can be used as a treatment response predictor that also provides insight into early treatment engagement and the patient’s ability or willingness to access emotional content, and can act as an early sign of overengagement (e.g., peak subjective units of distress occurring significantly earlier than peak HR) or underengagement (e.g., peak subjective units of distress being low or occurring significantly later than peak HR). As a critical mechanism for PTSD treatment response, examining when initial emotion activation occurs (i.e., determining in which session the emotion is initially activated) can predict treatment length and provide insight into treatment response rates (
12–
14). Because different physiological profiles of specific emotional reactions differ to some extent (
27), it may be fruitful to examine initial emotion activation in terms of specific emotion profiles as well as in terms of a measure of exposure engagement. Expanding our understanding of emotion activation from fear activation to other trauma-related emotions may increase our understanding of a number of phenomena, including differentiating acute, chronic, and complex PTSD.
Approach 3: Extinction
Statistical analysis for extinction.
Between- and within-session analyses for extinction were conducted by using mixed-effects multilevel models (MLMs). These models enable examination of within- and between-person effects, while minimizing residual errors and accounting for the high correlation between observed HR datapoints over time. Notably, this approach allows for comparison of sessions within individuals, sessions between individuals, and overall treatment trajectory changes between individuals. To find the observed intercept, therapeutic sessions were renumbered such that the first imaginal exposure session was session 0. Models were structured such that HR was the outcome variable predicted by fixed effects of linear and quadratic time (to model the expected extinction curve) and random effects of session nested within each participant. All models used restricted maximum-likelihood estimation, with an autoregressive covariance structure to account for the high level of homoscedasticity (i.e., homogeneity of variances) expected in the high-density repeated HR measure. Importantly, whereas an MLM is necessary for between-person comparisons when using highly correlated data (e.g., HR) over time, when looking for statistically significant changes, a clinician could examine a patient’s HR trajectory over time by using simple linear or quadratic regressions after each session and could compare the R2 statistic from each session to assess changes over time.
Potential benefits and limitations of the extinction approach.
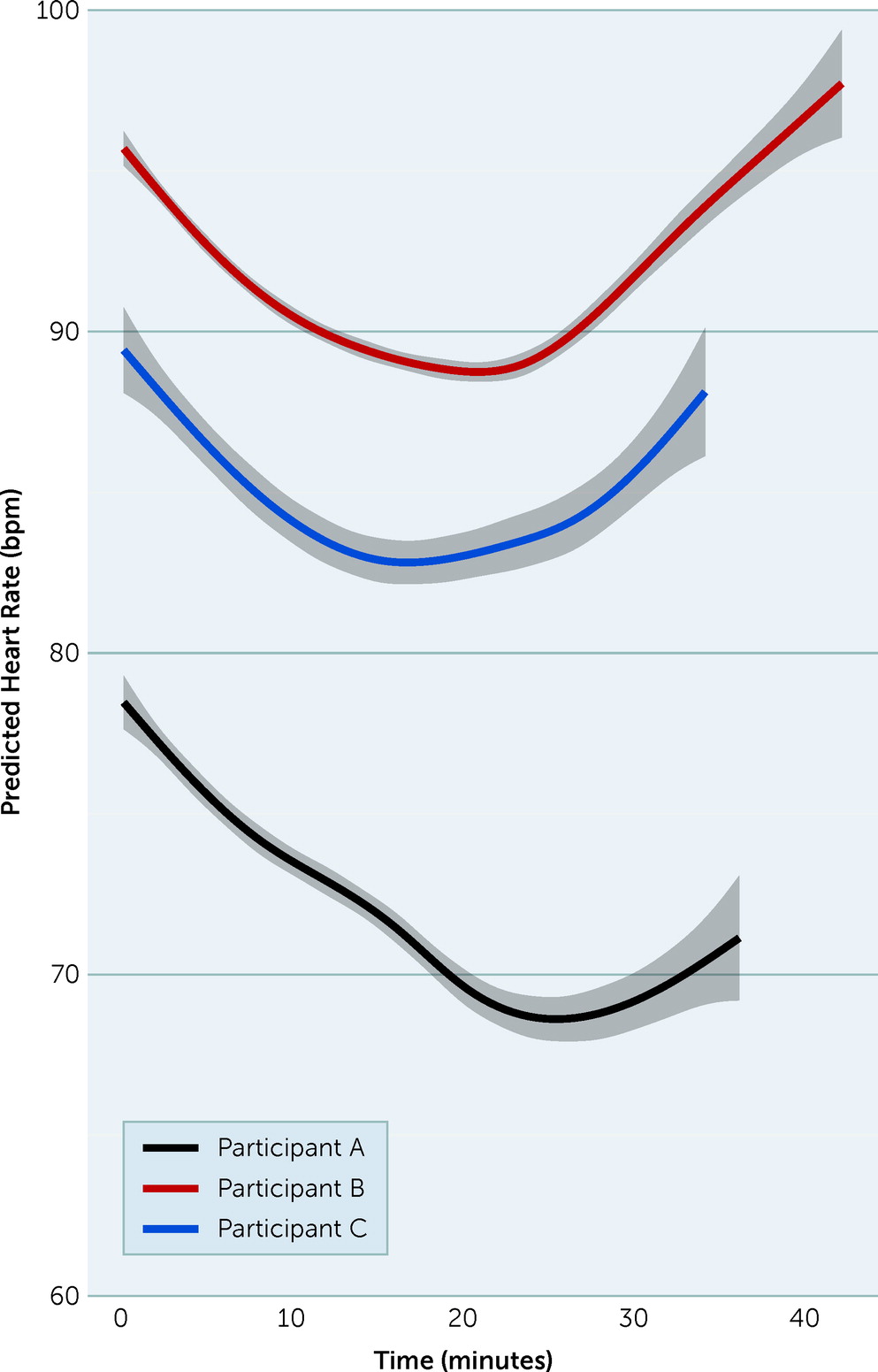
To compare participants, we included a time × session × subject interaction effect and all lower-order interactions in the models. There were no significant interaction effects in our sample (all p>0.491). Given our small sample, we did not expect significant effects, and we discuss these effects only for demonstration purposes (
Figure 3). Although this model did not reveal differences between participants in our sample, it did indicate significant linear and quadratic time effects—but no main effect of session or participant. These results suggested that across participants, there were significant changes in HR within sessions, although the pattern of these curves was similar across sessions and participants. Significant quadratic time effects suggested that the participants displayed the expected extinction curves within sessions, whereas nonsignificant session effects indicated that these curves did not differ between sessions, either within or between participants.
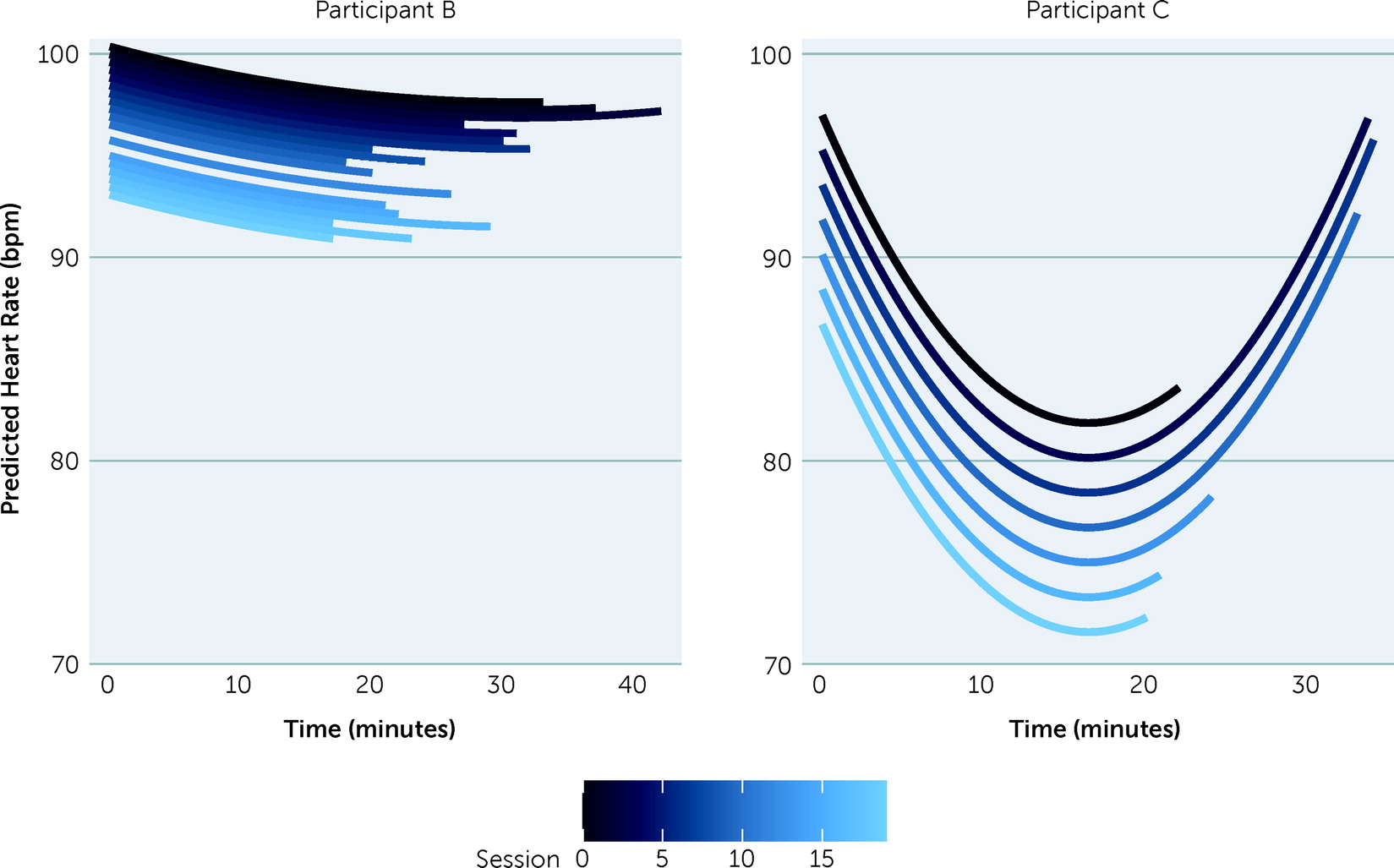
To examine within-person extinction patterns, data were divided into subsets so that models were analyzed for each participant separately (see
Figure 3). This model failed to converge (i.e., could not produce valid results) for participant A, suggesting there may have been too little variability (or complexity) between sessions for this participant’s data to be examined through an MLM. We therefore do not present model data from participant A. This model yielded nonsignificant results for participant B, indicating that the participant did not demonstrate within- or between-session extinction in terms of HR. However, for participant C, there were significant effects for both linear and quadratic time, although there was no effect of session. These results indicated that participant C demonstrated a pattern reflecting extinction within sessions, although there were no physiological differences between sessions. Participant C did make clinical gains over the course of treatment, suggesting that between-session extinction may not be a complete measure of treatment response.
Figure 4 displays model-predicted session curves for participants B and C.
Extinction is a measure of decreasing reactivity over time. Extinction is perhaps the best formulated measure of PTSD treatment engagement and response. Within-session extinction may provide insight into client progress toward processing the trauma memory, whereas between-session extinction may indicate processing over the course of treatment. In the present study, there was evidence for within-session extinction, particularly for participant C, who was a partial treatment responder. However, the MLM analysis provided no evidence of statistically significant between-session extinction. Importantly, clinical use of simpler statistics may reveal different extinction patterns, particularly when used with a larger sample.
Mechanistically, extinction measures may be used to assess the contributions of fear-extinction (
16) and inhibitory learning (
28) processes to PTSD treatment response. Within-session extinction may indicate a participant becoming less reactive to the trauma memory, without the therapist having to rely on distress ratings, which could be misleading if the individual has a low general distress tolerance or is emotionally numb (
11). Between-session extinction may provide evidence of processing and integration over time. Notably, previous studies (
6,
13,
17,
18) relying on self-reported data have suggested that between-session habituation, but not within-session habituation, predicts treatment response. Results from the present study indicated a variety of response trajectories, all of which can serve as useful predictors of treatment response in future work. Understanding the point at which extinction occurs during the course of treatment may provide clinicians with treatment response benchmarks, potentially indicating a need for protocol adjustments to facilitate extinction or inhibitory learning early during treatment, thereby decreasing treatment nonresponse rates.
Discussion and Conclusions
The primary aim of this study was to discuss three analytic approaches to incorporating mobile psychophysiological reactivity assessment during psychotherapy for PTSD. The overall goal of integrating psychophysiological measures into clinical practice is to improve treatment response via greater understanding of therapeutic mechanisms. Each approach to data analysis provides a different metric of psychotherapy engagement, process, and mechanism. However, all three measures could be used to predict treatment outcomes. Although the use of concordance between subjective units of distress and HR to measure emotional engagement is the newest approach, it offers an array of potential uses that may benefit individual patients and the field at large. However, as exemplified in our data from participant C, this measure is limited when working with individuals who lack emotional range or who may have a flat affect. Thus, it may be worthwhile to apply multiple approaches within the same study, because this participant’s data showed extinction over time via HR, despite no self-reported changes in distress.
Together, the three data analytic approaches to incorporating mobile psychophysiological assessment during psychotherapy for PTSD presented here can serve as a guide for clinicians and researchers in the future. By using these methods, researchers looking to further understand the mechanisms underlying exposure-based psychotherapy for PTSD can produce comparable studies, leading clinicians and researchers alike to a greater understanding of the best methods to treat PTSD.