DSM-IV Mania Symptoms in a Prepubertal and Early Adolescent Bipolar Disorder Phenotype Compared to Attention-Deficit Hyperactive and Normal Controls
Abstract
Introduction
Methods
Study inclusion and exclusion criteria
Subject ascertainment
Assessment instruments
Data analyses
Results
Characteristics of the study sample
Comparisons of DSM-IV mania symptoms
Concurrent elation and irritability
Suicidality, psychosis, mixed mania, and rapid cycling
Discussion
Limitations
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Mean | SD | Mean | SD | Mean | SD | F | p | t | p | t | p | t | p |
| Baseline age | 10.9 | 2.6 | 9.7 | 2.0 | 11.0 | 2.6 | 7.5 | 0.0007 | 3.3 | 0.0012 | 0.5 | n.s. | 3.9 | 0.0002 |
| Onset age of current bipolar episode | 7.3 | 3.5 | N/A | N/A | N/A | N/A | — | — | — | — | — | — | ||
| Years of current bipolar episode duration | 3.6 | 2.5 | N/A | N/A | N/A | N/A | — | — | — | — | — | — | ||
| CGAS score | 43.3 | 7.6 | 55.7 | 4.2 | 84.1 | 4.6 | 1237.5 | <0.0001 | 13.5 | <0.0001 | 44.2 | <0.0001 | 42.3 | <0.0001 |
| % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pubertal status | ||||||||||||||
| Prepubertal | 57.0 | 53 | 80.2 | 65 | 58.5 | 55 | 12.5 | 0.002 | 10.7 | 0.001 | 0.04 | ns | 9.5 | 0.002 |
| Pubertal | 43.0 | 40 | 19.8 | 16 | 41.5 | 39 | ||||||||
| Gender | ||||||||||||||
| Male | 61.3 | 57 | 79.0 | 64 | 61.7 | 58 | 7.8 | 0.02 | 6.4 | 0.011 | 0.003 | ns | 6.2 | 0.013 |
| Female | 38.7 | 36 | 21.0 | 17 | 38.3 | 36 | ||||||||
| Race | ||||||||||||||
| White | 89.2 | 83 | 87.6 | 71 | 90.4 | 85 | 0.3 | ns | 0.1 | ns | 0.1 | ns | 0.3 | ns |
| Other | 10.8 | 10 | 12.4 | 10 | 9.6 | 9 | ||||||||
| SES class | 2nd highesta | 2nd highesta | 2nd highesta | |||||||||||
ADHD=attention deficit hyperactivity disorder; CC=normal community control; ns=not significant; PEA-BP=prepubertal and early adolescent bipolar disorder phenotype a Subjects were in 2nd highest of five classes.
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom | % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p |
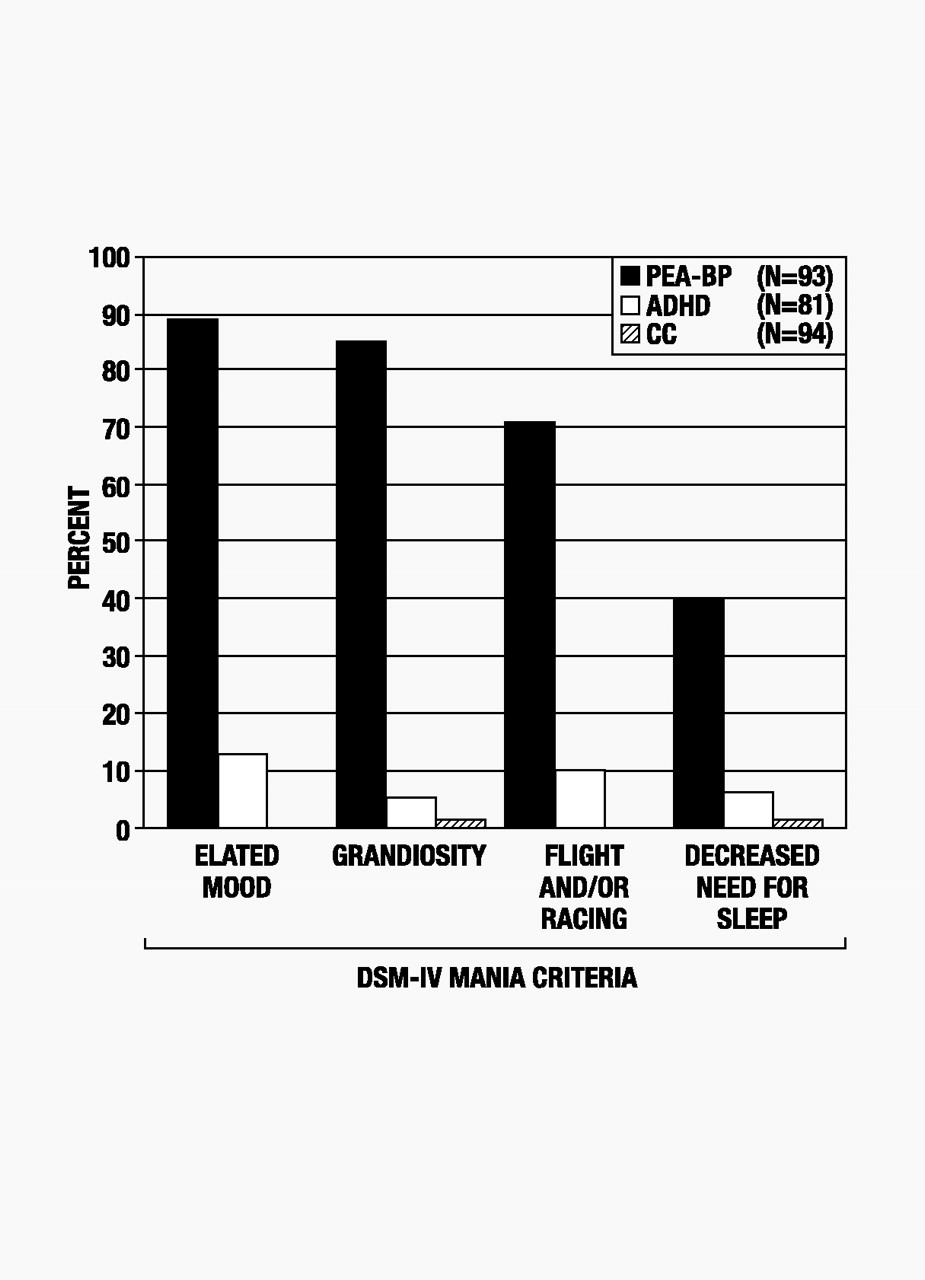
| Elated mood | 89.3 | 83 | 13.6 | 11 | 0.0 | 0 | — | — | 64.2 | <0.0001 | — | — | — | — |
| Grandiosity | 86.0 | 80 | 4.9 | 4 | 1.1 | 1 | 85.7 | <0.0001 | 61.0 | <0.0001 | 36.6 | <0.0001 | — | — |
| Flight and/or racing | 71.0 | 66 | 9.9 | 8 | 0.0 | 0 | — | — | 47.0 | <0.0001 | — | — | — | — |
| Flight of ideas | 57.0 | 53 | 8.6 | 7 | 0.0 | 0 | — | — | 32.0 | <0.0001 | — | — | — | — |
| Racing thoughts | 49.5 | 46 | 1.2 | 1 | 0.0 | 0 | — | — | 17.6 | <0.0001 | — | — | — | — |
| Decreased need for sleep | 39.8 | 37 | 6.2 | 5 | 1.1 | 1 | 33.3 | <0.0001 | 19.9 | <0.0001 | 16.0 | <0.0001 | 3.5 | ns |
ADHD=attention deficit hyperactivity disorder; CC=normal community control; DSM-IV=Diagnostic and Statistical Manual of Mental Disorders, 4th edition; ns=not significant; PEA-BP=prepubertal and early adolescent bipolar disorder phenotype a Controlled for age and gender and corrected for multiple comparisons (p=0.0021)
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom | % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p |
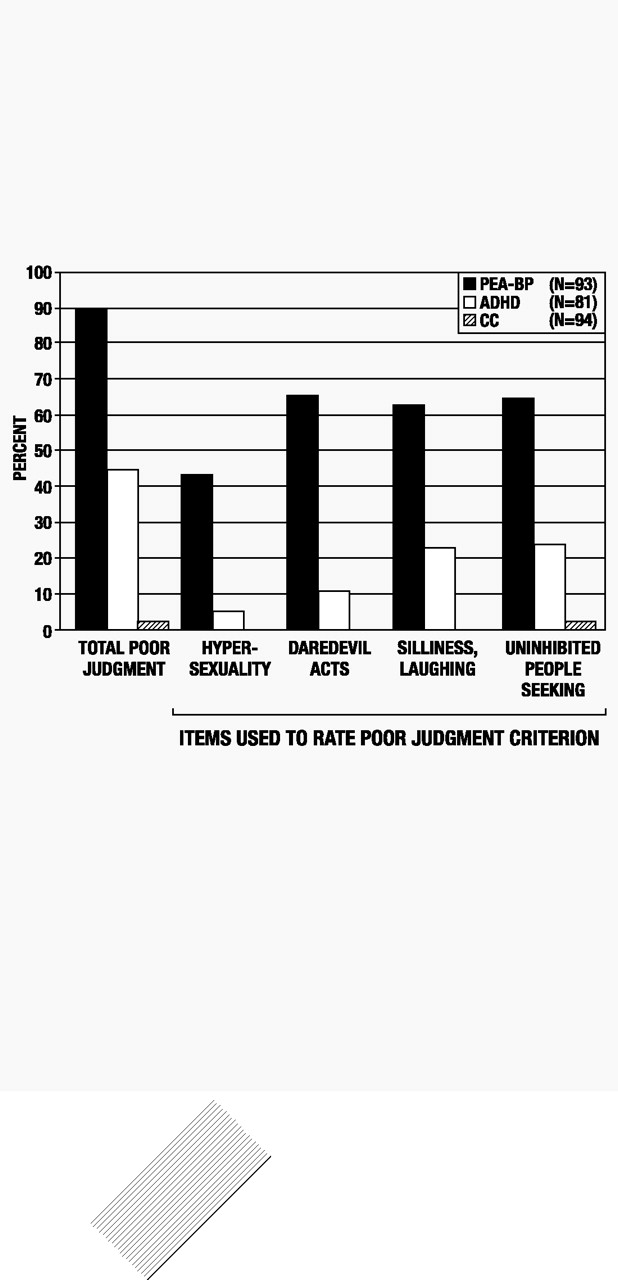
| Poor judgment | 90.3 | 84 | 44.4 | 36 | 3.2 | 3 | 74.3 | <0.0001 | 32.2 | <0.0001 | 65.1 | <0.0001 | 23.9 | <0.0001 |
| Hypersexuality | 43.0 | 40 | 6.2 | 5 | 0.0 | 0 | — | — | 20.8 | <0.0001 | — | — | — | — |
| Daredevil acts | 65.6 | 61 | 11.1 | 9 | 0.0 | 0 | — | — | 38.5 | <0.0001 | — | — | — | — |
| Silliness, laughing | 63.4 | 59 | 23.5 | 19 | 0.0 | 0 | — | — | 26.8 | <0.0001 | — | — | — | — |
| Uninhibited people seeking | 65.6 | 61 | 24.7 | 20 | 3.2 | 3 | 55.1 | <0.0001 | 22.7 | <0.0001 | 42.4 | <0.0001 | 11.8 | 0.0006 |
ADHD=attention deficit hyperactivity disorder; CC=normal community control; DSM-IV=Diagnostic and Statistical Manual of Mental Disorders, 4th edition; PEA-BP=prepubertal and early adolescent bipolar disorder phenotype a Controlled for age and gender and corrected for multiple comparisons (p=0.0025)
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptom | % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p |
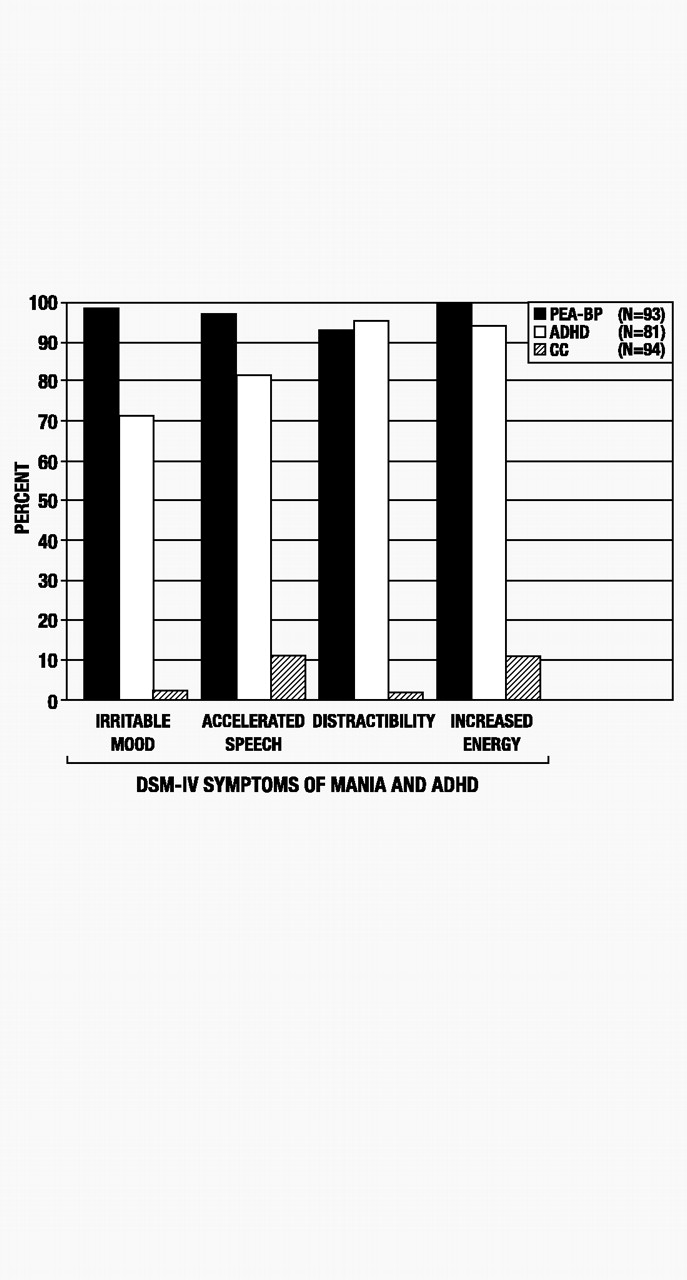
| Irritable mood | 97.9 | 91 | 71.6 | 58 | 3.2 | 3 | 68.0 | <0.0001 | 13.6 | 0.0002 | 45.7 | <0.0001 | 42.8 | <0.0001 |
| Accelerated speech | 96.8 | 90 | 81.5 | 66 | 11.7 | 11 | 84.8 | <0.0001 | 6.7 | ns | 62.9 | <0.0001 | 56.7 | <0.0001 |
| Distractibility | 93.6 | 87 | 96.3 | 78 | 2.1 | 2 | 64.8 | <0.0001 | 0.2 | ns | 40.0 | <0.0001 | 45.8 | <0.0001 |
| Increased energy | 100.0 | 93 | 95.1 | 77 | 11.7 | 11 | — | — | — | — | — | — | 62.6 | <0.0001 |
| Hyperenergetic | 94.6 | 88 | 88.9 | 72 | 6.4 | 6 | 97.3 | <0.0001 | 3.1 | ns | 53.8 | <0.0001 | 65.8 | <0.0001 |
| Increased productivity | 33.3 | 31 | 11.1 | 9 | 0.0 | 0 | — | — | 9.7 | ns | — | — | — | — |
| Sharpened thinking | 49.5 | 46 | 19.8 | 16 | 3.2 | 3 | 37.2 | <0.0001 | 13.5 | 0.0002 | 30.0 | <0.0001 | 11.0 | 0.0009 |
| Increased goal directed | 46.2 | 43 | 18.5 | 15 | 1.1 | 1 | 29.6 | <0.0001 | 14.8 | 0.0001 | 18.6 | <0.0001 | 8.5 | ns |
ADHD=attention deficit hyperactivity disorder; CC=normal community control; DSM-IV=Diagnostic and Statistical Manual of Mental Disorders, 4th edition; ns=not significant; PEA-BP=prepubertal and early adolescent bipolar disorder phenotype a Controlled for age and gender and corrected for multiple comparisons (p=0.0016)
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Feature | % | n | % | n | % | n | χ2 | p | χ2 | p | χ2 | p | χ2 | p |
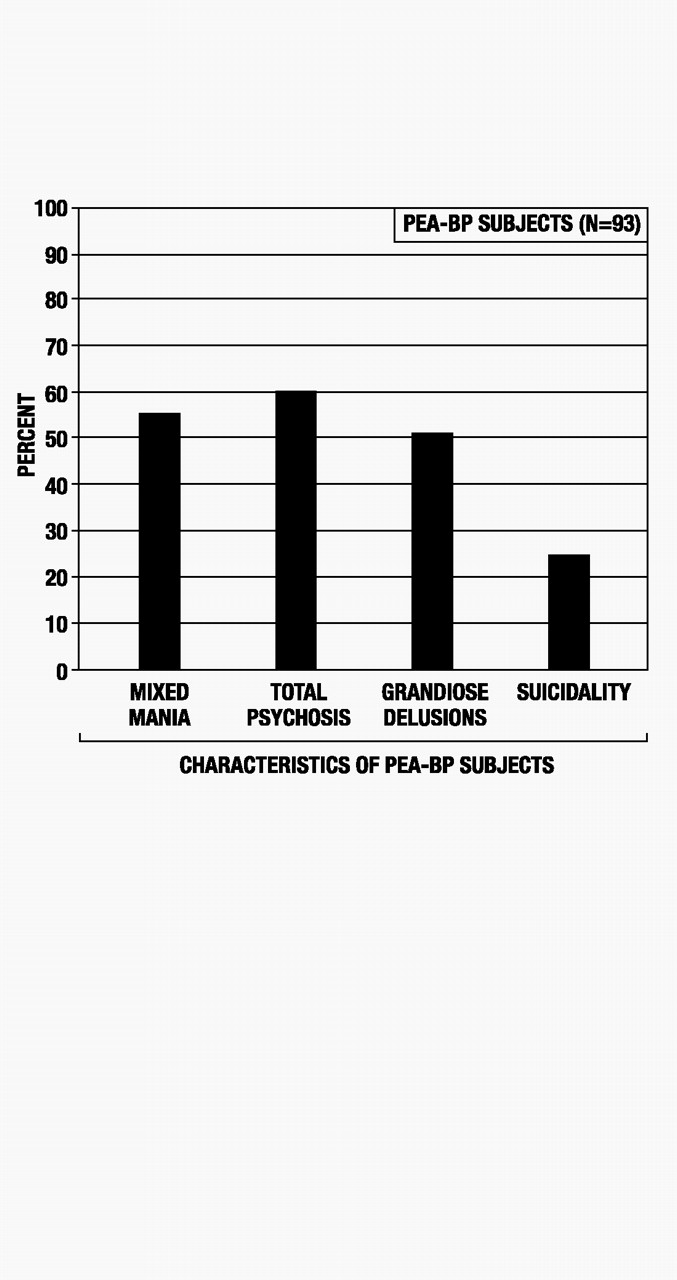
| Suicidality | 24.7 | 23 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
| Total psychosis | 60.2 | 56 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
| Grandiose delusions | 50.5 | 47 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
| Mixed mania | 54.8 | 51 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
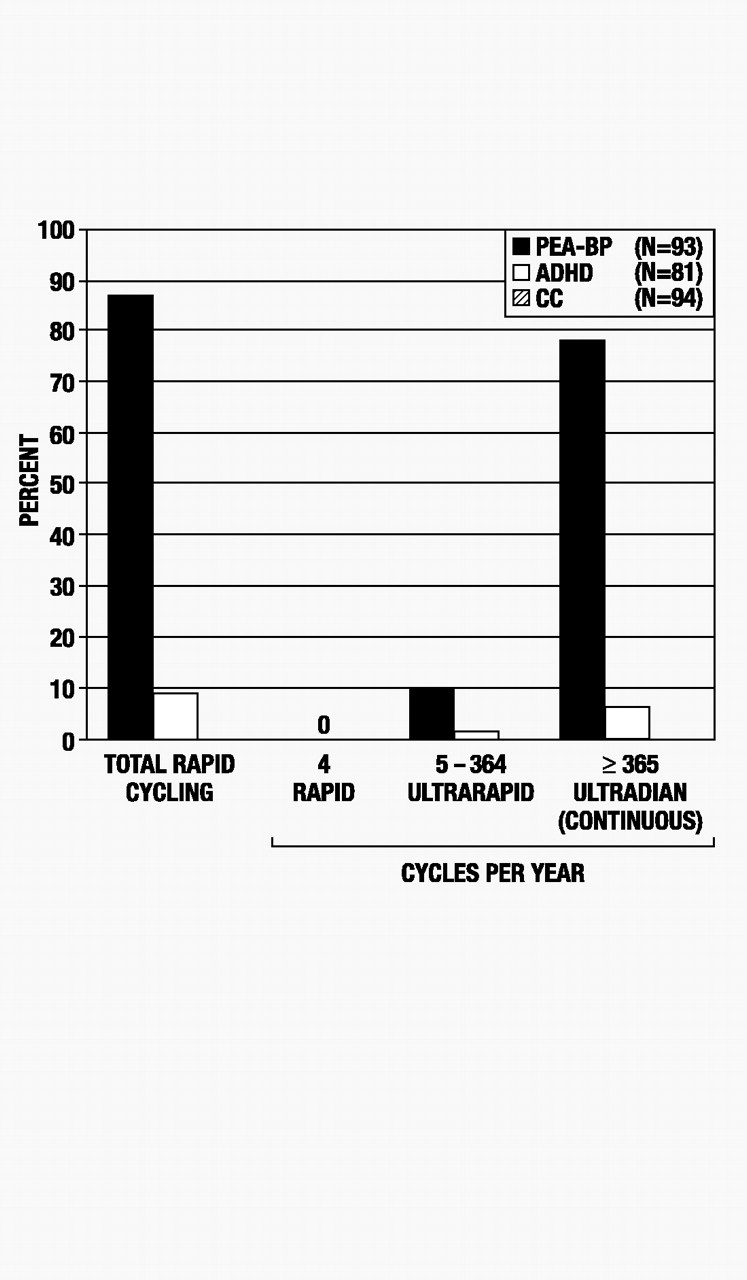
| Total rapid cycling | 87.1 | 81 | 8.6 | 7 | 0.0 | 0 | — | — | 66.1 | <0.0001 | — | — | — | — |
| Cycles/year | ||||||||||||||
| 4 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | — | — | — | — | — | — | — | — |
| 5–364 (ultrarapid) | 9.7 | 9 | 2.5 | 2 | 0.0 | 0 | — | — | 0.9 | ns | — | — | — | — |
| ≥365 (ultradian) | 77.4 | 72 | 6.2 | 5 | 0.0 | 0 | — | — | 55.1 | <0.0001 | — | — | — | — |
| PEA-BP | ADHD | CC | BP vs. ADHD vs. CC | BP vs. ADHD | BP vs. CC | ADHD vs. CC | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Feature | Mean | SD | Mean | SD | Mean | SD | F | p | t | p | t | p | t | p |
| Ultradian cycles/day | 3.7 | 2.1 | 3.0 | 1.8 | 0 | 0.0 | — | — | 8.1 | ns | — | — | — | — |
ADHD=attention deficit hyperactivity disorder; CC=normal community control; DSM-IV=Diagnostic and Statistical Manual of Mental Disorders, 4th edition; ns=not significant; PEA-BP=prepubertal and early adolescent bipolar disorder phenotype a Controlled for age and gender and corrected for multiple comparisons (p=0.0014)
Footnote
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).

