About 30% of psychiatric out-patients report residual depressive symptoms following treatment for acute depression (
Paykel et al, 1995). These symptoms are frequently drug refractory (
Cornwall & Scott, 1997). Our recent large, randomised controlled trial of 18 sessions of cognitive therapy (CT) with clinical management (CM) versus clinical management alone in 158 subjects with residual depressive symptoms who were receiving antidepressants (
Paykel et al, 1999) demonstrated that remission rates at 20 weeks were significantly greater in the CT plus CM group (24%) than in the CM alone group (11%). Cumulative rates of persistent symptoms or relapse were also significantly lower in the CT that in the control group: 10%
v. 18% at 20 weeks, 24%
v. 40% at 44 weeks, and 29%
v. 47% at 68.
This study explores whether the addition of CT to CM plus medication has any differential effects on the psychological and social functioning of individuals with residual depression and how any changes relate to the reduced relapse rates.
Method
The methodology has been described in detail by
Paykel et al (1999). Key aspects are highlighted here.
Subjects
Subjects were psychiatric out-patients aged 21–65 years, who had satisfied DSM-III-R (
American Psychiatric Association, 1987) criteria for major depression within the last 18 months. At randomisation, subjects were required to have current residual symptoms of at least 8 weeks’ duration. At entry, these symptoms needed to reach both: (a) a score of eight or more on the 17-item Hamilton Rating Scale for Depression (HRSD;
Hamilton, 1967) and (b) nine or more on the Beck Depression Inventory (BDI;
Beck et al, 1961). These criteria were modified from
Frank et al (1991).
Patients were excluded if they had a history of manic episodes, cyclothymia, schizoaffective disorder, definite drug or alcohol dependence, persistent antisocial behaviour or organic brain damage and where any other Axis I disorder was primary at the time of the index illness. Also excluded were patients meeting DSM-III-R criteria for borderline personality disorder, patients who persistently repeated self-harm, those with learning disabilities (IQ estimated clinically to be below 70), or other intellectual or linguistic factors precluding participation in the study and patients currently receiving formal psychotherapy. Patients who had previously received CT for more than five sessions were also excluded. Patients with DSM-III-R dysthymia were included, provided that the criteria for major depression were satisfied and the onset of dysthymia was not before age 20 years.
Patients were required to have been taking antidepressant medication for at least the previous 8 weeks, with at least 4 weeks at an adequate dose, defined as a minimum equivalent to 125 mg per day of amitriptyline and to have definite current side-effects, or to have refused explicitly to increase the dose of medication. Most doses and lengths of treatment were far in excess of this.
Study design
The study was a parallel two group trial employing 20 weeks’ treatment and 1-year follow-up. The treatment phase comprised 20 weeks of randomised treatment, during which all patients received drug continuation and CM, and one group received additional CT. Following this was a followup phase of 48 weeks, during which antidepressants, CM and rating procedures were continued.
After written informed consent, patients provided a full set of baseline ratings and were then randomised. Assignments in consecutively numbered sealed envelopes were prepared by the trial statistician (A.L.J.) stratified by centre, previous major depressive episodes (two or more v. fewer); length of present illness, including both index major depression and residual symptoms (1 year or more v. less); and severity of index major depression (global ratings of mild or moderate v. severe or psychotic).
The pre-set sample size was 160 subjects (80 per treatment group), which gave 80% power to detect by the log-rank test at P=0.05 (two-tailed) a 50% reduction in relapse rates for 40 to 20% and an effect size of 0.45 in two-tailed parametric tests of continuous measures.
Treatment
Drug continuation and CM involved sessions of about 30 minutes each with a study psychiatrist every 4 weeks during the treatment phase, and every 8 weeks during the follow-up phase. The content of interviews was modified from
Elkin et al (1989). In our model, symptoms were rated, limited support provided and drugs prescribed. Use of specific cognitive and behavioural techniques was not allowed. Patients were continued on the same anti-depressant as at inclusion, but a dosage increase was permitted to 30% greater than at the point of inclusion and up to a total of two consecutive extra out-patient sessions once weekly. No formal psychotherapy was permitted without withdrawal from the study. Sessions were audiotaped and monitored to ensure protocol compliance and absence of cognitive therapy.
Patients allocated to CT in addition to CM plus medication were seen for 16 CT sessions over 20 weeks plus two booster sessions at approximately Week 26 and Week 32. The therapy was modified from Beck’s original model (
Beck et al, 1979) and a manual was used (
Scott, 1998). Therapists were already trained and experienced in CT and during the study there was regular joint supervision of the two therapists by J.S.
Sessions were audiotaped and assessed by an independent rater to ensure therapist competency and fidelity to the CT.
Assessments
Subjects were assessed every 4 weeks until Week 20 and every 8 weeks thereafter by the study psychiatrist, and at baseline, 8, 20 and 68 weeks by a research assistant. Both were blind to treatment group and patients were requested not to reveal any details that might prejudice blindness. As total blindness is difficult to achieve, we incorporated three additional strategies. First, we gave subjects clear instructions that they should try to avoid revealing information about which group they had been allocated to. Second, we asked the raters to make guesses of group allocation. Third, all potential cases of relapse or withdrawal from the study were subjected to independent rating by a rater who was blind to treatment.
Baseline clinical assessments are described in detail elsewhere (
Paykel et al, 1999), and included: history of present and previous episodes; personal history; premorbid personality functioning (including the Eysenck Personality Inventory); Schedule for Affective Disorders and Schizophrenia modified for DSM-III-R criteria; treatments received and levels of adherence. The symptom measures described below were rated at baseline and at follow-up assessments.
Ratings on the HRSD and BDI were used to categorise subjects into pre-defined remission, persistent symptoms and relapse groups in our previous paper (see
Paykel et al, 1999), but group mean scores over time were not described. As these scales are the most widely used observer and self-rating measures of depression, the repeated ratings are reported here. The other repeated ratings included the following.
The Raskin Depression Scale (RDS) was used as a global rating of depression severity. It explores the extent to which an individual demonstrates depression on three sub-scales (rated 1–5): verbal self-report, behaviour and secondary symptoms of depression. Scores range from 3–15, with higher scores indicating greater severity.
Clinical Interview for Depression (Paykel, 1985)
The Clinical Interview for Depression (CID) is a 36-item scale which also provides separate total scores for anxiety (four items) and depression (10 items). The CID was used as it is particularly useful for discriminating between treatment effects on individual symptoms. Each item is rated on a seven-point scale (1, absent; 7, severe) making the CID more sensitive than other depression rating scales. The items included in the depression rating were: depressed mood, depressed appearance, guilt and self-esteem, hopelessness and pessimism, suicide risk, work interests, anorexia, delayed insomnia, retardation and agitation. We also included initial insomnia as this may be important in residual depression (
Paykel et al, 1995;
Fava, 1999).
The Social Adjustment Scale (SAS) was rated less frequently (at Week 0, 20 and 68). The SAS is an established measure of social and vocational functioning, using a semi-structured interview to assess areas such as work and leisure activities as well as assessing behaviours across these different domains such as dependency, interpersonal interactions and friction in relationships. Each item is rated on a five-point scale. Mean sub-scale scores were derived by summing scores on each relevant item and then dividing by the number of items rated. Scores ranged from 1 to 5, with lower scores indicating a higher level of functioning. An overall social adjustment rating is derived from the scores on each of the nine sub-scales.
Data analysis
An intention to treat analysis (including all randomised patients) was undertaken. Repeated measures analysis included as covariates the five stratification variables used in randomisation, and five additional variables considered possibly important: HRSD at entry, Eysenck Personality Inventory, neuroticism sub-scale (EPI-N) score, age at entry, gender and presence of melancholia at index major depressive episode. In addition, initial ratings on the specific item being analysed were included as a covariate.
Initially, for each of the five assessment scales (HRSD, BDI, RDS, CID, SAS) plots of standard deviation against mean for each group at each visit were produced to assess the relationship between the two. In most instances these plots indicated that analysis of raw (untransformed) data was appropriate; others, however, required log transformation. Repeated measures analyses of variance of the separate assessment scales of depressive symptoms were carried out in SAS version 3.2 for Windows using a mixed model (PROC MIXED) which can cope with the unbalanced effect that arises from missing observation. The analysis incorporated two between-subject effects (between groups and between subjects within groups) and three within-subject effects (between times, group by time interactions and random variation). The time effect and its interaction with group were broken down into linear, quadratic and cubic components. The advantages of using mixed models for the analysis of repeated measures with missing data over the more traditional approaches using general linear models have recently been documented (
Cnann et al, 1997;
Everitt, 1998;
Albert, 1999). The mixed model also requires specification of the within-subject covariance structure, that is, the way in which both the variation within subjects and the correlation between measures assessed at different time points change with time. To assess this, analyses were produced using three separate structures: compound symmetric, where the variation between subjects (within treatment groups) at each time point and the correlation between measures at different time points (irrespective of the interval between them) are both constant; first-order autoregressive (AR(1)), where the variation within subjects at each time point is constant and the correlation between measures at two different time points decays (in a structured way) with separation; and unstructured, where no pattern is imposed. Type III hypotheses for fixed effects were incorporated to ensure that all baseline covariates were adjusted for simultaneously.
Nominal study weeks were used as the measure of time, with the initial interview taken as baseline. Comparative runs were undertaken for the treatment phase (Weeks 4–20), follow-up phase (Weeks 28–68) and whole study (Weeks 4–68).
As social adjustment was assessed on only three occasions, two separate analyses of variance were used to assess changes in ratings by group and time (at Week 20 and Week 68 with baseline ratings as a covariate).
One subject from the control group was excluded from all analyses because of insufficient baseline data. In all other cases, missing baseline values were replaced by treatment group means. The 5% level was used for deciding statistical significance.
Results
Study flow and drop-out
Two hundred and thirty patients appeared to meet criteria for the study, but 72 individuals refused full assessment or randomisation. Of the 158 subjects who agreed to participate, 78 subjects were randomised to CM alone and 80 to CT plus CM. In the CM only group 66 subjects (85%) adhered to protocol until the end of the study or until relapse, while 61 of the CT plus CM group (76%) did so. Full or fairly complete ratings to relapse or end of study were obtained for all except six subjects in the CM and 10 in the CT plus CM groups (see
Paykel et al, 1999).
Initial characteristics of treatment groups
Initial characteristics of the two treatment groups demonstrated that they were closely comparable on key variables (see Table 1). Subjects had a mean age of 43 years and, unusually for a depression study, about 50% were male. The majority of index episodes (including residual symptoms) were over 1 year in duration, and the index major depressive episodes were rated as severe in over 50% of cases. Two-thirds of subjects had a history of depression. Mean symptom ratings at baseline were in the middle of the residual depression range (
Paykel et al, 1995): HRSD (12.2; s.d.=2.8), BDI (22.1; s.d.=7.9), RDS (6.4; s.d.=1.4) and CID depression total (25.0; s.d.=3.7) respectively. The mean CID anxiety score was 9.6 (s.d.=3.8). The mean SAS score was 2.1 (s.d.=0.5), suggesting moderate levels of social impairment.
Changes in depression
Over the 20-week acute treatment phase, the HRSD, BDI, RDS, CID depression and CID anxiety scores fell by about 20% (see Table 2). There were no statistically significant between-group differences or group by time interactions.
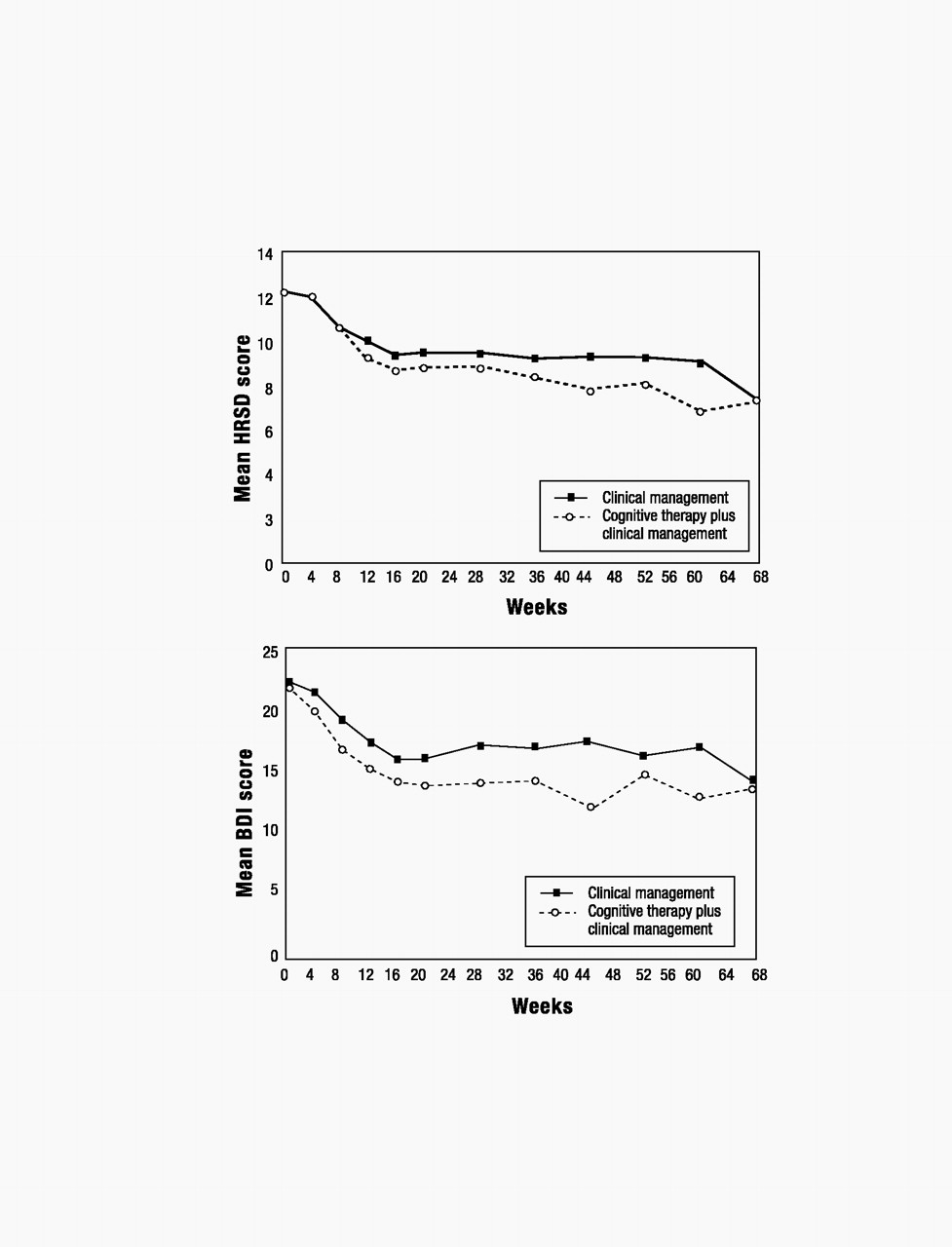
Throughout the treatment and follow-up phases, there was a non-significant trend toward lower HRSD, BDI and CID anxiety scores in the CT plus CM group as compared with the CM only group (see Fig. 1).
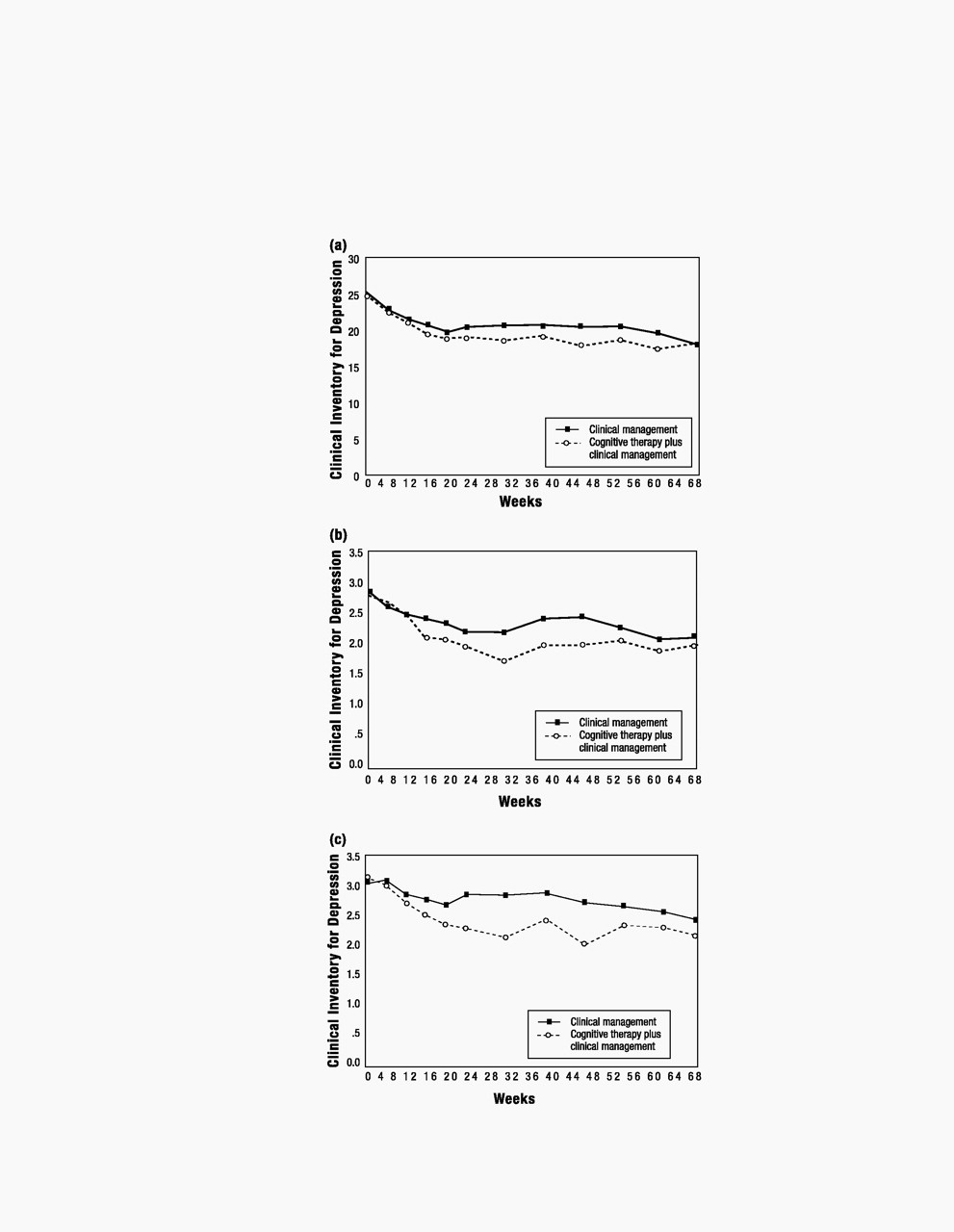
Over the whole study period there were significant group by time interactions for CID depression (F=4.6; d.f.=1323; P=0.03) and RDS scores (F=4.4; d.f.=1319; P=0.04) and two individual CID items measuring key psychological symptoms of depression (see Table 2). The first item assessed guilt and self-esteem (F=6.6; d.f.=1323; P=0.01), and the second item assessed hopelessness and pessimism (F=6.8; d.f.=1323; P=0.01). As shown in Fig. 2, differences between groups were most marked on all ratings in the first 6 months of follow-up (Weeks 20–44), but then converged by final follow-up (at Week 68). At Week 44 the mean difference between groups was 0.44 (95% CI 0.05–0.83) for guilt and self-esteem, and 0.65 (95% CI 0.28–1.01) for hopelessness and pessimism. There were no statistically significant between-group differences or group by time interactions for the other CID depression items.
Changes in social adjustment
The total SAS score and all sub-scale scores changed over time between baseline assessment and Week 20 and between baseline and Week 68. As shown in Table 3, significant between-group differences emerged by the end of the acute treatment phase for total SAS score (F=7.6; d.f.=1129; P=0.01) and for four of the sub-scale scores: dependency (F=4.2; d.f.=1127; P=0.04), friction (F=5.25; d.f.=1128; P=0.02), interpersonal behaviour (F=4.7; d.f.=1128; P=0.03) and interaction with extended family (F=4.1; d.f.=1123; P=0.04).
By Week 68 these between-group differences were no longer apparent. Neither group had returned to the baseline level of functioning. However, group means converged between Weeks 20 and 68.
Discussion
We have demonstrated that, in comparison with CM alone, CT plus CM may have a particular role in the prevention of relapse in subjects with residual depression (
Paykel et al, 1999). This paper shows that CT plus CM has statistically significant differential effects on some drug-refractory residual symptoms. Taken together, these data allow an exploration of how CT reduces relapse rates. There appear to be three potential mechanisms of relapse prevention: overall reduction in levels of depressive symptoms or social impairment, changes in specific symptoms associated with relapse, and changes in individual coping skills.
Overall reduction in depressive symptoms
Both the CM only and the CT plus CM groups showed statistically significant changes in overall levels of depressive symptoms and social adjustment over time. However, there were relatively few significant between-group differences in depressive symptom ratings and these only became significant when assessed over the 68-week study period. In comparison with control subjects, CT subjects showed greater reductions in RDS score and CID total depression score. While these differences were statistically significant, the actual differences in mean scores between groups were modest. Furthermore, similar trends on the HRSD and BDI scores did not reach statistical significance. It is feasible, but not proven, that there was less possibility of demonstrating treatment effects because patients had lower levels of baseline symptomatology than those reported in acute treatment studies. However, our findings do not demonstrate with any certainty that overall reduction in level of residual depressive symptoms is a clinically meaningful explanation of reduced relapse rates.
Significant between-group differences in social adjustment were most marked during the acute treatment phase. Improving social adjustment is important given the 60–80% prevalence of subjective impairment in partially remitted depression and its association with subsequent relapse (
Mintz et al, 1992;
Fava, 1999). The changes in SAS sub-scale scores may reflect the specific targeting with CT of certain personality traits that are often associated with persistent depression (e.g. dependency), while changes in interpersonal behaviour and reduced friction in relationships may reflect more explicit emphasis on interpersonal context when using CT in chronic affective disorders (
Markowitz, 1994;
Scott, 1995). However, by Week 68 there were no significant between-group differences on any SAS sub-scale score.
Changes in specific symptoms
The second hypothesis is that changes in specific symptomatology are critical in relapse prevention. The findings that there were significant group by time interactions for changes in CID item scores for guilt and self-esteem, and hopelessness and pessimism, replicate previous research. In one of the earliest studies,
Rush et al (1981) reported that CT was particularly associated with changes in mood, views of self and hopelessness. Furthermore, CT was associated with greater reductions in hopelessness and improvements in self-esteem than antidepressant medication (
Rush et al, 1982). Later studies comparing CT with medication that controlled for initial severity and/or chronicity of symptoms (e.g.
Imber et al, 1990) failed to find any mode-specific effects for the psychological and pharmacological interventions employed. However, none of the studies was of similar statistical power to the present one.
Given the explicit targeting in CT of symptoms such as low self-esteem and hopelessness (and of interpersonal problems in chronic depression), the specific symptom changes noted above are not unexpected. However, there is only limited evidence to support the view that low self-esteem and feelings of hopelessness predict future depressive relapse (e.g.
Evans et al, 1992;
Paykel et al, 1995). The known association between expressed emotion, marital dissatisfaction and depressive relapse (e.g.
Hooley & Teasdale, 1986) may mean that reducing friction in relationships was particularly beneficial. Interestingly,
Hayhurst et al (1997) noted higher levels of criticism when one partner had residual depressive symptoms. The most frequently reported critical comments were about depression and depressed mood in general (39%) and dependency in particular (15%).
Changes in individual coping skills
The final hypothesis takes into account that changes in residual symptoms alone may not be a sufficient explanation of the changes in relapse rates. In studies of the use of CT in panic disorders it has been demonstrated that, although CT reduces the risk of relapse, individuals are often left with substantial levels of residual symptoms of anxiety. It is suggested that CT may prevent relapse primarily by preventing the escalation of these anxiety symptoms to panic in response to internal or external stressors. Our data also appear to show that relapse rates can be significantly reduced without gross changes in depressive symptoms. In a comprehensive theoretical review,
Persons (1993) suggested that one mechanism of action of CT was that it taught people compensatory skills that allowed them to manage their symptoms and problems more effectively. In our studies, the significant association between CT and relapse prevention in the absence of a strong association between CT and symptom reduction suggests that, in residual depression at least, patients are learning how to cope with persistent symptoms so that they are less likely to escalate to relapse.