Erotomania After Aneurysmal Subarachnoid Hemorrhage: Case Report and Literature Review
Abstract
CASE REPORT
This 48-year-old right-handed Korean-born woman presented in 1987, at age 39, with sudden onset of headache and alteration of consciousness. Computed tomography (CT) of the head showed extensive subarachnoid hemorrhage, and cerebral arteriography demonstrated an aneurysm of the tip of the basilar artery. Subsequently, the aneurysm was surgically clipped via a right subfrontal craniotomy. A CT scan on the first postoperative day showed a right frontoparietal subdural hematoma, which was evacuated via the same craniotomy. One week later, a left frontal ventriculoperitoneal shunt was placed for persisting hydrocephalus. The patient recovered and was able to return to work after several months.Four years after the hospitalization, the patient was treated for depression and was noted to comment about a romantic relationship that was “not working out.” It became evident she believed that a physician at the hospital where she worked was in love with her. She based this belief on the “special” look he had given her in the hospital cafeteria. There was no known prior contact between the patient and this physician. He denied any romantic inclinations, but the patient persisted in her belief. She sent gifts, made phone calls, and visited the office where he practiced. This behavior continued despite ongoing psychotherapy, treatment with neuroleptics, and a restraining order. After multiple violations of the restraining order, she was committed to a psychiatric hospital.On admission in 1996, she was neat in appearance and had good eye contact. She steadfastly held to her belief that the physician loved her and would return her affections if he were not constrained by his job and family. She complained of recurring depressive symptoms with fleeting suicidal ideation, and dull, diffuse headaches. She denied appetite or sleep disturbance, anhedonia, crying spells, manic symptoms, anxiety, hallucinations, thought broadcasting, or thought insertion. She had some difficulty maintaining a coherent train of thought, but memory was intact, and language was normal in both Korean and English. Simple calculations, limb and facial praxis, figure and clock drawing, cortical sensory testing, Luria maneuvers, and alternating sequences were normal. Cranial nerves, power, tone, coordination, gait, reflexes, and sensation were intact.Neuropsychological testing included the Wechsler Adult Intelligence Scale–Revised (WAIS-R), which revealed a Verbal IQ (VIQ) of 75, Performance IQ (PIQ) of 89, and Full Scale IQ (FSIQ) of 81. Testing with the Wechsler Memory Scale (WMS) yielded a memory quotient of 87. She obtained a score of 5 (borderline performance) on the Memory for Designs test. Evaluation with the Bender-Gestalt suggested difficulties with organizational abilities, and she had mild deficits with visual memory. Performance on the Trail Making Test was impaired, more so on Part B than Part A. The neuropsychologist who performed the tests felt these results represented the patient's premorbid level of function, based on her education, employment, and the fact that English was her second language.CT scans were available from the initial illness and from 8 years later, when erotomania was fully established. The original scans indicated diffuse cerebral involvement from subarachnoid hemorrhage and hydrocephalus that was later corrected by a ventriculoperitoneal shunt.Concurrent medical problems included non–insulin-dependent diabetes mellitus and peptic ulcer disease. Medications included risperidone, sertraline, metformin, and ranitidine. Past medical history included high blood pressure, osteoarthritis, cholecystectomy, and hysterectomy. She did not smoke and denied alcohol or drug use. She denied any family history of neurologic or psychiatric illness.The patient was born in rural South Korea and received only 4 years of education before the outbreak of the Korean War. She had been hospitalized at the ages of 16 and 20 after suicide attempts by pill overdose. After marrying an American serviceman and coming to the United States at age 26 she had two children, and she later divorced this husband after 17 years of marriage. She remarried a year later, only to have her second husband die in 1995. She reported chronic feelings of loneliness and depression, leading to the psychiatric hospitalization 4 years earlier at the onset of her erotomanic delusion.The patient also reported vivid memories of three near-death experiences. The first occurred when she was 8 years old; all of the children in the home, including the patient, were very ill with high fever, and one sister died. The second near-death experience occurred with a pill overdose at age 21, and the third with her ruptured aneurysm. She repeatedly stated her belief that God had worked through American doctors to make her live.
DISCUSSION
Erotomania
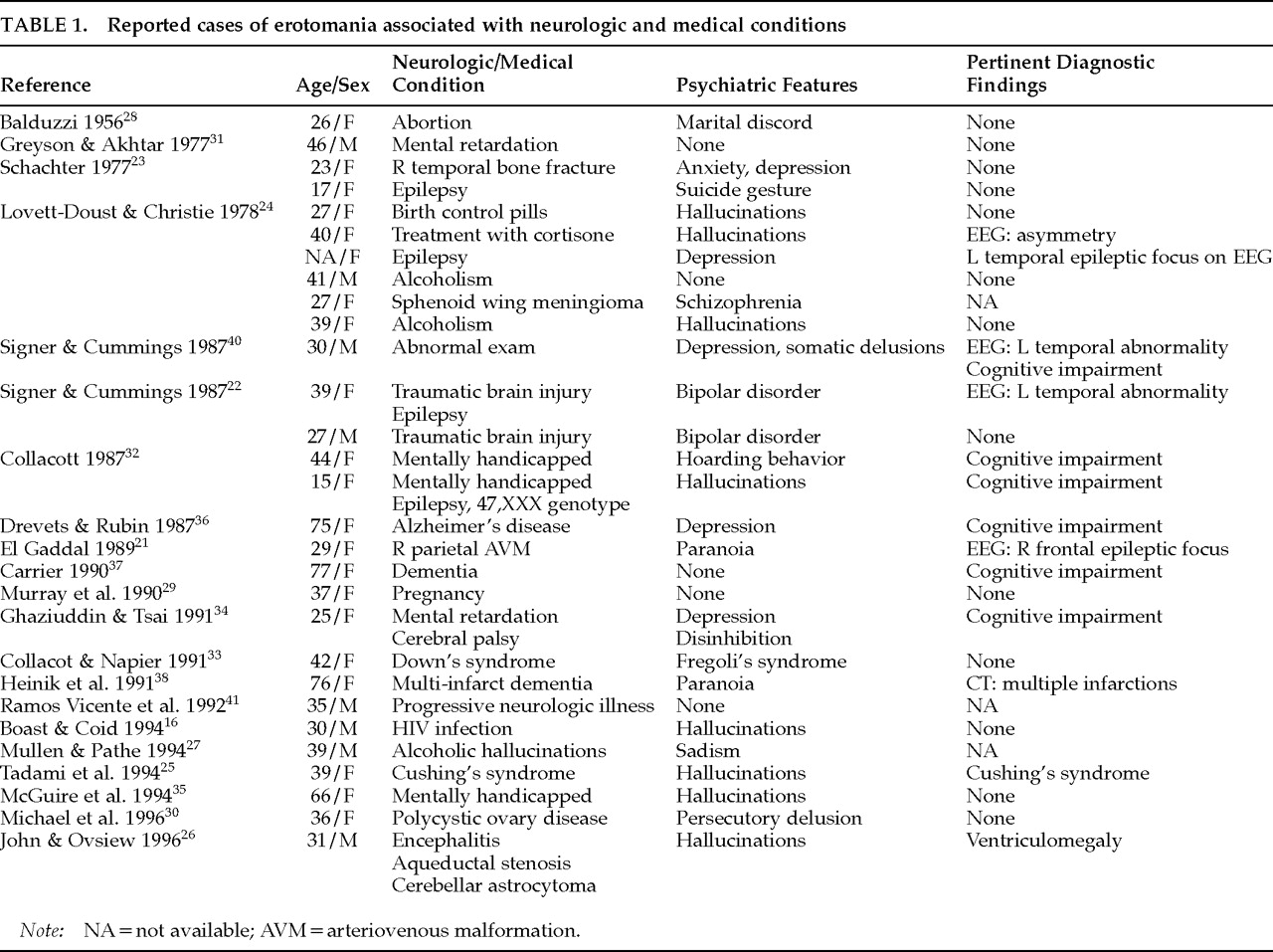
Neurologic and Medical Conditions
Subarachnoid Hemorrhage
Traumatic Brain Injury
Seizure Disorder
Endocrinologic Conditions
Brain Tumor
Alcohol Abuse
Gynecological Conditions
Infection
Developmental Delay
Dementia
Undefined Disorders
Neuropsychiatric Correlates
Representation of Emotion in the Brain
Misinterpretation and Abnormal Belief
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
There are no citations for this item
View Options
View options
PDF/ePub
View PDF/ePubGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).