Dementia Associated With Vitamin B12 Deficiency: Presentation of Two Cases and Review of the Literature
Abstract
CASE REPORTS
Patient 1. Patient O.F., male, was referred to a hospital at the age of 64 years because of confusion and collapse. According to relatives and colleagues from work, O.F. had shown a slowly progressive change of behavior and deterioration of working efficiency as an administrative employee over the previous 5 years. Recently he had been able to manage only the workload of a part-time employee, although he voluntarily worked additional hours on Saturdays. Several times he was sent home from work because of confused speech, walking impediment, and inability to complete his work correctly. Additionally, he showed an increasing withdrawal from social activities and a loss of interest in previous hobbies.On admission to the hospital he was awake and cooperative, but disoriented. He showed serious impairment of cognitive functions and short-term and long-term memory. Formal thinking was slowed. Drive, facial expression, spontaneous movements, and abstract thinking ability were reduced. He frequently complained of memory deficits, and he had a lack of appetite resulting in a weight loss of 11 kg over a period of 6 weeks.Physical examination revealed a pale and dry skin and emphysematic lungs. The neurological examination showed diminished tendon reflexes and a reduced sense of posture and vibration of the legs. Primitive reflexes (palmomental and snout reflexes) were positive. CT scan and MRI of the brain showed a generalized cerebral atrophy. EEG, cerebrospinal fluid, Doppler sonography of the cerebral arteries, and xenon SPECT for the measurement of cerebral blood flow did not show any abnormalities. The serum vitamin B12 level was in the lower normal range (307 pg/ml). The red blood count was normal. The Schilling test was pathological (9% absorption of cobalamin), but normalized after substitution of intrinsic factor (18% absorption), indicating a lack of intrinsic factor. Gastroscopy revealed atrophic gastritis, which was confirmed by biopsy. Serum titers of antibodies specific for parietal cells were not elevated, however.Detailed psychological testing (complete Wechsler Adult Intelligence Scale–Revised, Benton Visual Retention Test, Trail Making Test, and Mini-Mental State Examination [MMSE]) reflected an average overall IQ (102). Concentration and the ability to solve complex cognitive tasks were reduced, however. At the retest approximately 5 weeks later (under substitution of vitamin B12 and additional therapy with doxepin and lorazepam), the patient showed a significantly better performance IQ (112) and improved cognitive speed.
Patient 2. Patient A.H., male, was admitted to our psychiatric clinic at the age of 77 years. For the previous 13 years he had had the delusional fear of impoverishment. However, when he encountered special offers, he bought unnecessary amounts of cheap and often useless items, which he then collected in his apartment. For the past 11 years he had been known to suffer from pernicious anemia, yet he had only rarely accepted parenteral vitamin B12 substitutions.On admission he was disoriented to time and situation, was afraid of impoverishment, and had a depressed mood. Neurological examination revealed bilaterally reduced visual acuity, reduced ankle jerks, and a markedly diminished sense of posture and vibration. CT scan of the brain showed generalized atrophy. Doppler/duplex sonography of the cerebral arteries did not indicate significant stenosis. Visual evoked potentials were normal; somatosensory evoked potentials were pathologically delayed. Nerve conduction studies measured delayed and reduced action potentials, indicating polyneuropathy.The red blood count revealed a macrocytosis with elevated mean corpuscular hemoglobin concentration (36.1 g/dl) and volume (102 fl μm3). The vitamin B12 level was borderline low (203 pg/ml), with a borderline pathological Schilling test (9.85% absorption; after substitution of intrinsic factor, 12.38% absorption). Antibodies specific for thyroglobulin, parietal cells, and microsomes were not detectable. Stool tests for parasites were negative. A gastroscopy was refused by the patient. The CSF had a normal cell count but an elevated protein content (59 mg/100ml), indicating a disturbed blood–CSF barrier.Psychological testing was difficult to perform and revealed an average overall IQ (104). Short-term memory was severely impaired and cognitive flexibility was reduced. The patient was treated with vitamin B12 in combination with an antidepressant (clomipramine) and initial anxiolytic medication (lorazepam). A second psychological testing was refused by the patient. On dismissal from the clinic, in contrast to the time of admission, he was fully oriented and his mood was balanced.
VITAMIN B12 DEFICIENCY: LITERATURE REVIEW
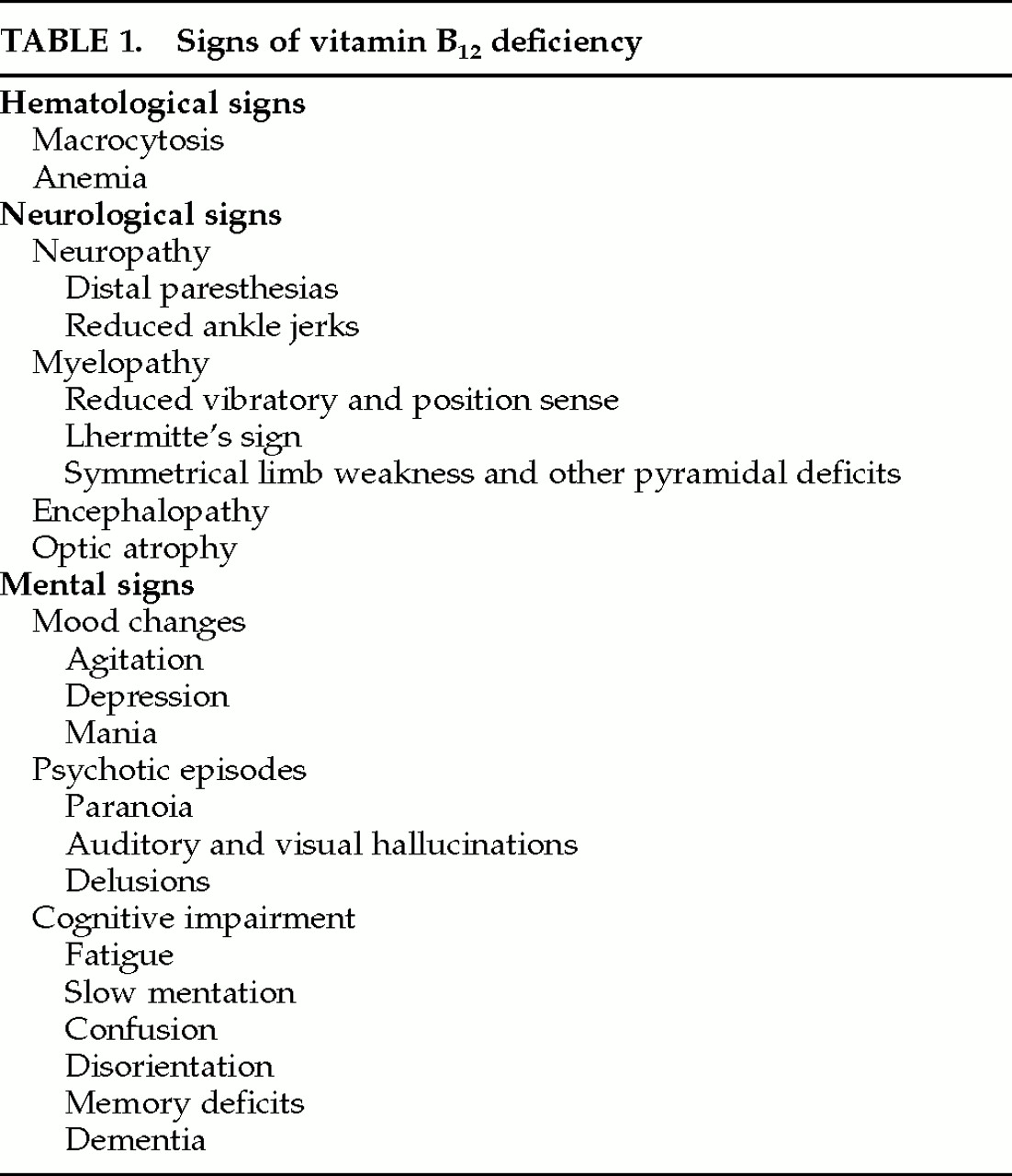
Clinical Features
Associated Mental Changes
Pathophysiology
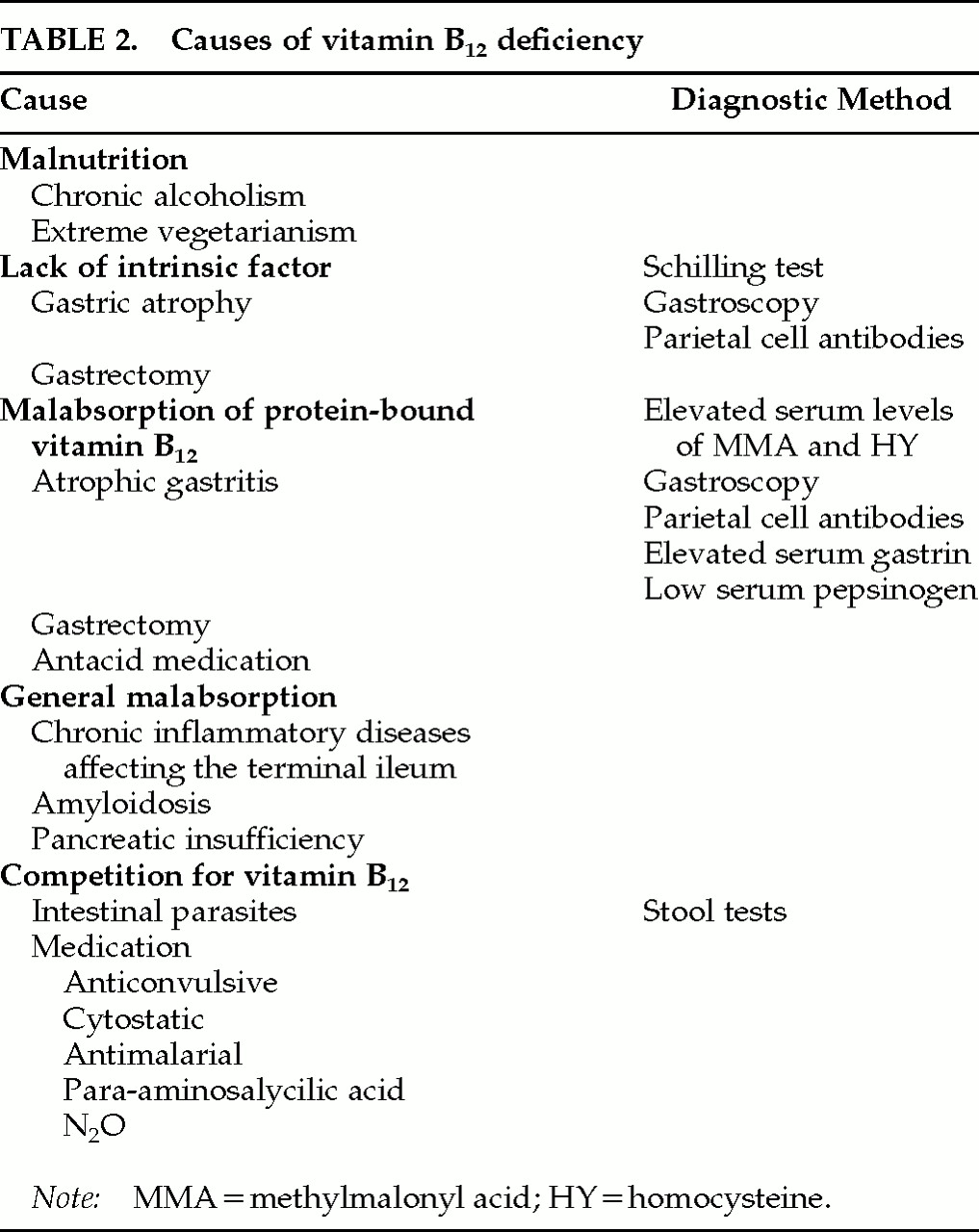
Causes
Diagnostic Aspects
Treatment
Prognosis
DISCUSSION
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
There are no citations for this item
View Options
View options
PDF/ePub
View PDF/ePubGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).