Dentatorubral-Pallidoluysian Atrophy (DRPLA) Presenting With Psychosis
Abstract
CASE REPORTS
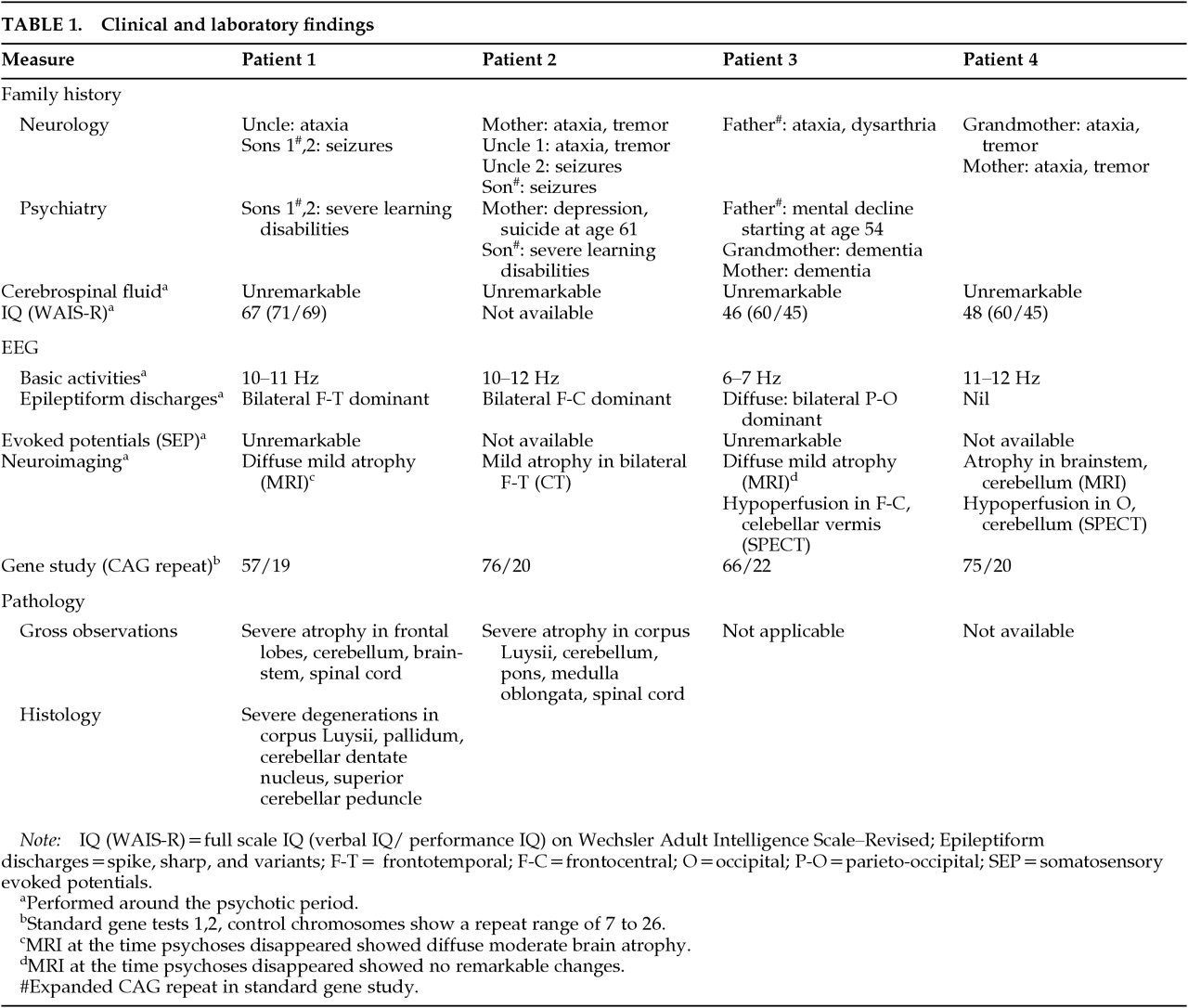
Patient 1 was a Japanese man who died of multiple organ failure at age 64. His clinical symptoms to age 56 have been reported in part elsewhere.8Neurological findings. The patient developed a finger tremor at age 40. By age 42, he showed mild dysarthria and unsteadiness. Cerebellar ataxia gradually progressed, his physical condition declined, and the patient was bedridden and required tube feeding by age 57. He demonstrated myoclonic seizures and generalized tonic-clonic convulsions at age 59.Psychiatric findings. Starting at age 40, he became short-tempered and careless. At age 46, he experienced persecutory delusions. He thought that neighbors were trying to sue him and that they had assembled a group of hooligans to assault him. Furthermore, he described delusions of grandeur, believing himself, for example, to have discovered a perfect treatment for tinea. When he expressed these delusions, he was agitated but conscious. The delusions disappeared within 3 months with administration of haloperidol 4 mg/ day.
Patient 2 was a Japanese man who died of acute pneumonia at age 56.Neurological findings. This patient showed fine finger tremor at age 39 and mild gait ataxia at age 43. He developed recurrent generalized seizures and severe truncal ataxia. He was bedridden by age 50 and was fed by gastric tube at age 52.Psychiatric findings. He became short-tempered and frequently exhibited brief delusional moods (Wahnspannung) starting at age 45. He developed persecutory delusions, believing that hospital personnel were reporting him to the police as a criminal, that he was being watched by fellow patients as well as the police, and that his personal affairs were reported in the newspaper. These delusions faded with haloperidol administration (1.5–3 mg/day). Thereafter, his cognitive function and daily activity level declined steadily.
Patient 3 is a 35-year-old Japanese woman.Neurological findings. This patient exhibited recurrent myoclonic seizures and mild gait ataxia starting at age 24. She had her first generalized seizure at age 25. At age 29, generalized seizures increased to one per day, and athetotic movements and dysarthria were noted.Psychiatric findings. She had been short-tempered and had exhibited eating disorders and school phobia since age 14. Beginning at age 18, she was subject to psychogenic faints and/or falls when faced with unpleasant circumstances. Since age 28, she demonstrated frequent brief delusional moods (Wahnspannung) and auditory hallucinations while clearly conscious. She experienced persecutory delusions, believing, for example, that someone in the hospital ward was telling wicked stories about her and had stolen her personal belongings. Her psychotic symptoms have been controlled by haloperidol (1.5 mg/day).
Patient 4 was a Japanese man who died of acute pneumonia at age 47.Neurological findings. This patient showed mild dysarthria and mild gait ataxia at age 30, both of which were slowly progressive. At age 39, he suffered from neuroleptic malignant syndrome resulting from administration of haloperidol and levomepromazine. He showed generalized tonic-clonic seizures and athetoid movements at age 41. He experienced generalized tonic-clonic status epilepticus repeatedly and became almost bedridden at age 45.Psychiatric findings. He showed aspontaneity, emotional withdrawal, and muttering starting at age 32. At age 38, he exhibited loss of association and self-mutilation, and was admitted to a psychiatric hospital with a diagnosis of schizophrenia. He developed delusions of persecution and reference in clear consciousness at age 39. He also expressed thoughts that unless he used the toilet frequently, his urine flowed backward and spurted from his mouth. These delusions lasted for 18 months. After these delusions disappeared, emotional instability, aggression, and behavioral disinhibition (sexual aberration) were preponderant. His memory function and daily activity level declined gradually but profoundly.
DISCUSSION
ACKNOWLEDGMENTS
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
There are no citations for this item
View Options
View options
PDF/ePub
View PDF/ePubGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).