Tardive dyskinesia (TD) is a movement disorder that affects approximately 20%–60% of people continually treated with conventional antipsychotics.
1,2 It has an unknown pathophysiological basis. Dopamine (D
2) receptor supersensitivity, gamma aminobutyric acid (GABA)-ergic hypofunction, excitotoxicity, and oxidative stress have all been implicated in the pathophysiology of TD.
3–5 However, the D
2 hypothesis has been widely accepted as a major contributing factor to this movement disorder. Long-term administration of conventional antipsychotics increases D
2 receptor sensitivity and D
2 turnover. These changes are believed to be associated with the development of TD.
6 However, this is not consistently reported, and some investigators have found no significant association between the D
2 system and TD.
7–11 Methodological issues have contributed to these reported differences. First, medication effects relating to the evaluation of TD are a primary consideration. Because most people with schizophrenia need to take antipsychotics throughout their entire life, one must consider the influence of antipsychotics on the severity and clinical course of TD, including covert or withdrawal TD. Second, TD is a dynamic disorder associated with changes in both severity and pattern over time, possibly unrelated to medication treatment. To have confidence in the TD diagnosis, the evaluation should be conducted consecutively.
12 Third, because antipsychotics may induce other motor side effects and other neurological disorders are frequently combined with TD, false positive diagnoses are common.
Buspirone is an azaspirodecanedione derivative that has affinity for both 5-HT
1A as a partial agonist and D
2 receptors as an antagonist.
13 Buspirone evokes the release of prolactin through both mechanisms.
14–17 Prolactin provocation to buspirone has been considered useful in evaluating serotonin and D
2 receptor function. We evaluated D
2 and 5HT
1A receptor sensitivity in people with stringently evaluated TD, using prolactin responses to buspirone in order to assess the underlying physiology of vulnerability to TD. Prolactin response to buspirone varies in many psychiatric disorders, and buspirone challenge studies are uncomplicated. Differences in response to buspirone, if present, may also lead to a useful predictive test of vulnerability to dyskinesia. Second generation antipsychotics have lowered but not eliminated the risk of dyskinesia, particularly in sensitive populations such as the elderly.
18 Therefore, accurate assessments of risk and greater understanding of pathophysiology in this area are still critically needed.
METHOD
Subjects
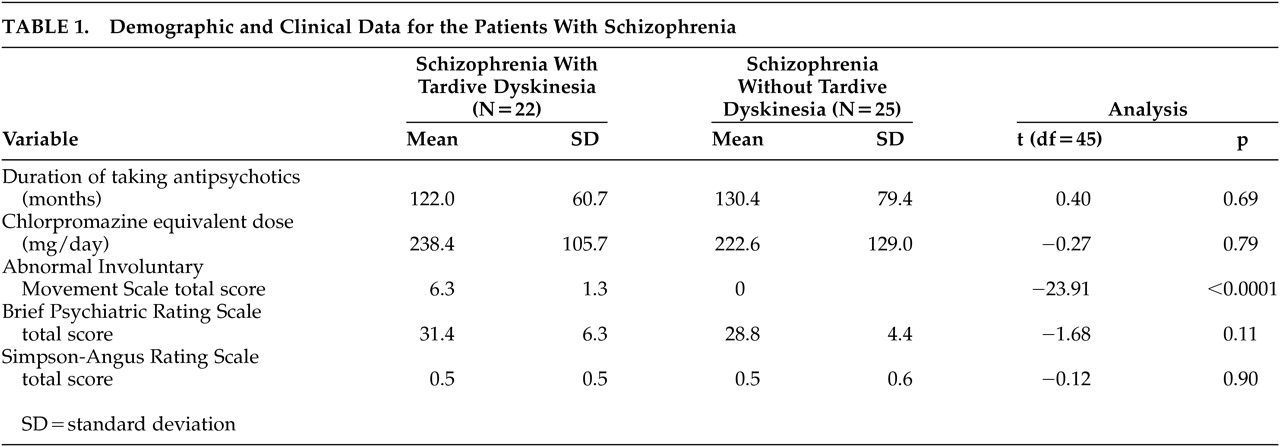
In this study, 87 Korean male subjects participated: 22 subjects with schizophrenia and TD; 28 subjects with schizophrenia but without TD; and 37 healthy comparison subjects. All patients were recruited through Dongsuh Hospital Inpatient Unit. Women were not included in this study, and we wanted to avoid the confounding effect of the difference of baseline prolactin level on the prolactin response to buspirone because prolactin levels in women can be influenced by their menstrual cycle. All patients met DSM-IV criteria for a schizophrenia diagnosis, and all were considered clinically stable. No subjects met DSM-IV criteria for any other axis I or II disorder, as determined by means of psychiatric interview and the Structured Clinical Interview for DSM-IV, which were conducted by a psychiatrist. Subjects who had a history of neurological and endocrine disorders, recent dental problems or artificial teeth were excluded. Comparison subjects were healthy volunteers, with no history of major psychiatric disorder and no family history of major psychiatric disorder in first-degree relatives.
Clinical Ratings
To avoid the compounding effect of extrapyramidal symptoms, subjects who showed overt parkinsonian symptoms (rated more than two points on Simpson-Angus Rating Scale
26) were excluded. Diagnosis for TD was based on DSM-IV and Schooler and Kane criteria for TD.
19 Two experienced psychiatrists performed the research ratings independently, and interrater reliability was greater than r=0.90 (p<0.001), with standard videotape ratings. To confirm the presence of TD, three consecutive evaluations were performed for each subject: at baseline, 3-month follow-up, and after the drug washout period. Subjects who met the criteria for TD on all three occasions were classified as having TD. Stringent characterization of the non-TD subjects included a total score of less than 2 points on the Abnormal Involuntary Movement Scale (AIMS)
27and less than 1-point on each individual AIMS item on three consecutive evaluations. The physical health of each subject was confirmed by medical examination, standard laboratory tests, a chest X-ray, electrocardiogram (ECG), and electroencephalogram (EEG) prior to participation. The Institutional Review Board approved the study, and all subjects gave informed consent prior to study participation.
Neuroendocrine Testing
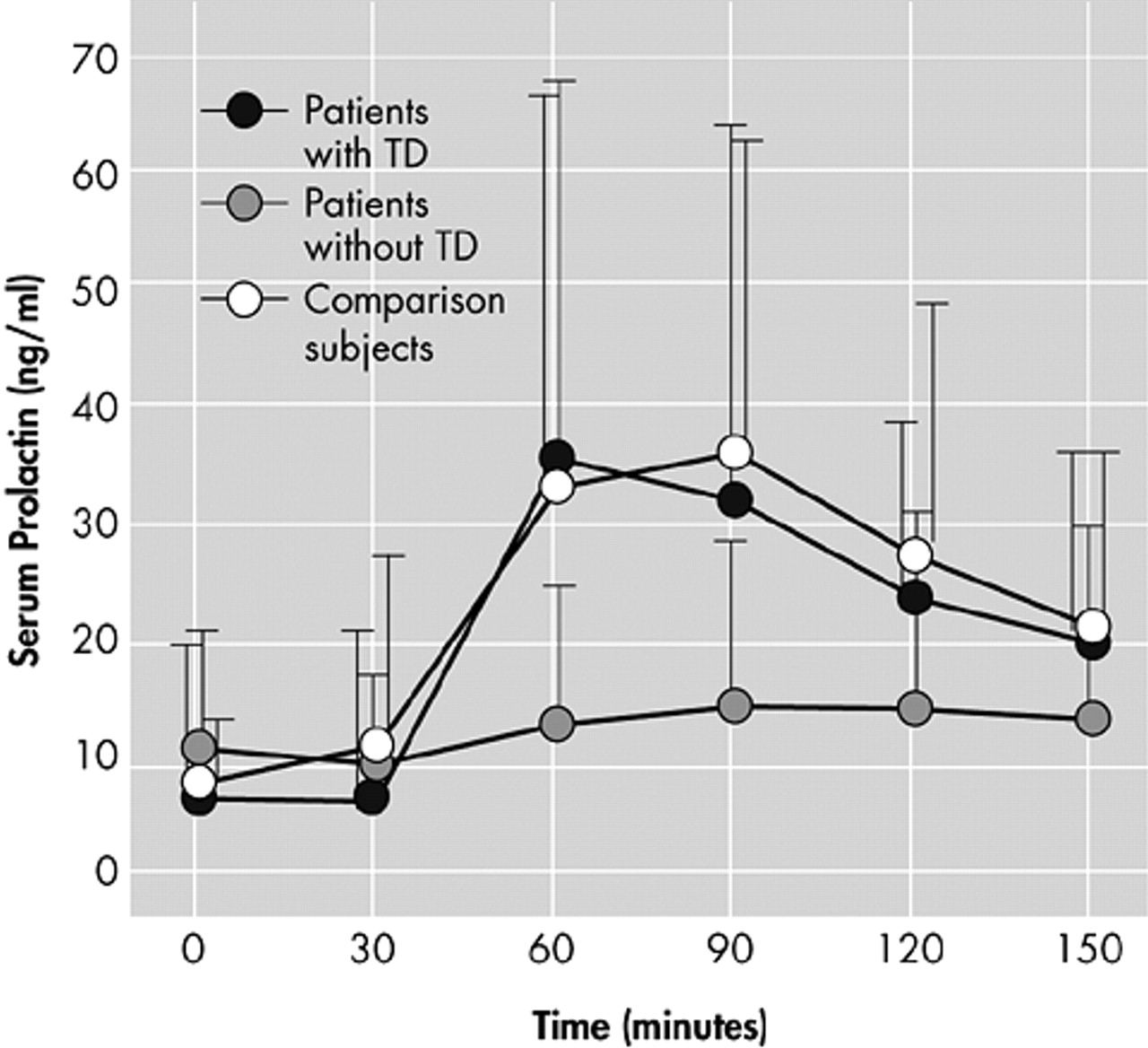
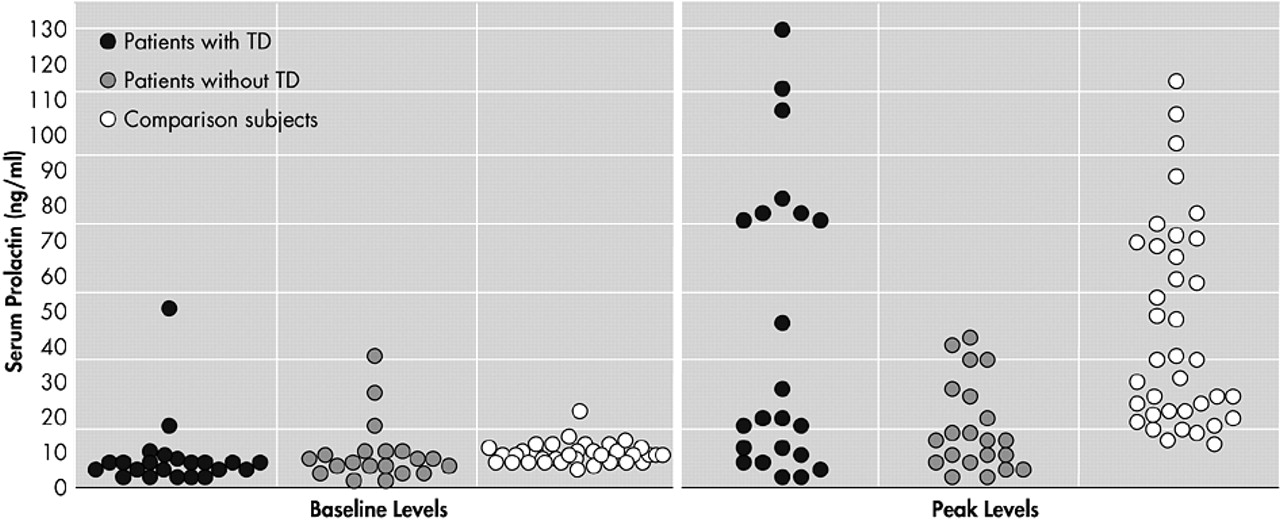
All subjects had been taking conventional antipsychotics (haloperidol, chlorpromazine, thioridazine, trifluoperazine, fluphenazine) and were withdrawn from their medication 1 week prior to study. Five people without TD were withdrawn from the study after drug washout because of newly onset dyskinetic movements and refusal of cannular insertion for blood drawing. No subjects showed aggravated psychotic symptoms during the washout. Thus, data were analyzed for 82 Korean, male subjects: 22 with schizophrenia and TD; 25 with schizophrenia but without TD; and 37 healthy comparison subjects. At baseline, subjects were required to attend the laboratory at 7:00 a.m. after an overnight fast. Between 7:30 a.m. and 8:00 a.m., an indwelling venous cannular was inserted into the superficial forearm vein. For the duration of the test, subjects rested and remained fasting except for water. To measure serum prolactin concentrations, blood was drawn at 0, 30, 60, 90, 120 and 150 minutes after oral administration of 30 mg buspirone hydrochloride, which was administered at 9:00 a.m. Serum was stored at −20°C until assayed. Serum concentrations of prolactin were determined by Electrochemiluminoscence assay, using a commercial kit (Boehringer Mannheim). Inter- and intraassay coefficients of variation were 4.8% and 2.8%, respectively.
Statistical Analysis
Two-tailed student’s t test and analysis of variance (ANOVA) were used to characterize differences between demographic and clinical variables. Prolactin levels in healthy comparison subjects were compared with subjects with and without TD separately. Repeated measures ANOVA was used to evaluate the effect of time and time-by-group interaction between groups. Analysis of covariance (ANCOVA) was used to determine the significance of difference between groups in prolactin levels at each time point following buspirone administration. Analysis of variance was used to compare the peak levels among the groups. An alpha level of 0.05 was considered statistically significant, and all tests were two-tailed.
DISCUSSION
The principal findings of this study indicate that schizophrenia subjects without TD showed a significantly decreased prolactin response, reflecting D2 receptor down-regulation and/or serotonergic system insensitivity. However, schizophrenia subjects with TD showed no significant difference in prolactin responses, when matched up against healthy comparison subjects.
Although D
2 receptor sensitivity is a leading hypothesis of the pathogenesis of TD, our results do not match the D
2 receptor supersensitivity theory. Although the D
2 supersensitivity hypothesis has been widely accepted as the leading theory of TD, it still has not been confirmed. Moreover, it should be noted that D
2 supersensitivity does not always follow long-term administration of antipsychotic drugs.
7–11,20The effects of previous antipsychotic drug treatment in subjects with schizophrenia may be a confounding factor and limitation to the study. Although all drugs were withdrawn at least 1 week prior to the study, this may have not been enough time to exclude persisting effects of antipsychotics on the brain. However, if effects of previous drug treatment were markedly persistent, baseline prolactin levels in the schizophrenia group should have been different from the healthy comparison subjects. This was not the case, however. Additionally, differences in the clinical characteristics of our subjects and those of patients in previous studies might produce different results, as dopaminergic transmission, D
2 synaptic concentration, and D
2 receptor occupancy by D
2 may differ, according to the severity and course of schizophrenic illness.
21 However, illness characteristics did not vary between our TD and non-TD group, which is probably an unlikely explanation of our findings. It is difficult to explain explicitly why schizophrenia subjects with TD showed no significant difference in prolactin responses, compared with healthy subjects.
It is interesting to note that subjects without TD in our study demonstrated blunted prolactin responses to buspirone, which may mean there was decreased D
2 receptor sensitivity in these subjects. It is well known that the prevalence of TD occurs in approximately 20%–60% of subjects treated continually with antipsychotic medication. This means that 40%–80% are relatively resistant to developing TD. There are few explanations as to why some patients remain free from TD, even though they have been taking antipsychotics for long periods. Previous studies indicate that decreased or absent D
2 receptor supersensitivity could be related to a reduction of TD risk. In animal studies, acute administration of sulpiride and clozapine, known not to produce TD, appear to act at D
2 receptor sites, but continuous chronic administration of these compounds does not result in the development of striatal D
2 receptor hypersensitivity.
22 Chronic administration of haloperidol increases striatal D
2 receptor hypersensitivity. For example, it enhances 3-hour spiroperidol binding in the striatum and in mesolimbic loci.
23 Other evidence demonstrates that certain drugs, such as carbamazepine, may improve haloperidol induced dyskinetic movement by reducing D
2 supersensitivity
24 or decreasing blood levels
25 and, as a result, brain exposure to haloperidol. Although these results cannot provide direct evidence to show that decreased D
2 receptor sensitivity is related to the low incidence of TD, they suggest that decreased D
2 receptor sensitivity may play an important role in reducing the development of TD. Therefore, we can propose that decreased D
2 receptor sensitivity may play a role in reducing the development of TD in some patients.
We do not know the mechanism by which people without TD in our study showed a decrease in D2 sensitivity. This may have been a result of individual variable compensation to the chronic administration of antipsychotics, reactions which could be influenced by genetic variability.
Our results, however, should be interpreted with caution due to other limitations. First, the effect of buspirone on prolactin response may not directly reflect the changes in central dopaminergic or serotonergic function but some combination of both. This nonspecificity challenges our result regarding the D2 receptor sensitivity-TD relationship. This work should be followed by a study of buspirone challenge with and without pindolol, a 5-HT1A agonist, which would help differentiate the dopaminergic versus serotonergic components of the response. Second, long-term administration of antipsychotics may change the D2 receptor sensitivity. However, it is not yet clear how well prolactin response to buspirone can reflect the functional state of D2 receptors. Third, medication-related effects, such as differences in the past history of antipsychotic medication and the potential role of drug metabolism, should be considered in interpreting our results, although there were no obvious differences between the TD and non-TD groups. All subjects were men and fairly young, limiting the generalizability of our results. Additionally, there was no placebo-control, although a stringent criterion was utilized for diagnosing TD. However, the inclusion of a healthy comparison group partially mitigates such a problem. These findings may yield more needed research in this area. This result may lead to a fuller understanding of the variable expression of D2-receptor mediated side effects in patients treated with antipsychotics.