S evere cognitive impairment in the elderly has been found to be associated with higher mortality, even after controlling for sociodemographic characteristics, comorbid health conditions, and other clinical variables.
1 Several community-based studies have specifically investigated mortality in dementia and reported an increased risk of death in demented compared with nondemented subjects.
2 –
6 However, few studies have utilized a validated neuropsychological battery to ascertain “caseness” of dementia or mild cognitive impairment in the community setting. Even fewer studies have examined the effect of less-severe cognitive disorders, such as mild cognitive impairment, on mortality risk in a community setting.
The Memory and Medical Care Study (MMCS) conducted at the Johns Hopkins Medical Institutions is a prospective observational cohort study which examined variations in the practice of caring for cognitively impaired elders living in the community. Specifically, this study analyzed whether these variations affected important outcomes, such as nursing home placement, quality of life, medical care expenditures, morbidity, and mortality. The objective of this report was to investigate the relationship between levels of cognitive impairment, including mild cognitive impairment, and 3-year mortality in a community-based, longitudinal study of elders at risk for dementia.
METHOD
The protocol for the MMCS was approved by the Committee on Human Research, the Institutional Review Board for the Johns Hopkins Bloomberg School of Public Health. The MMCS identified subjects from three previously established, community-based study samples conducted in Maryland.
7 –
10 Among the 1,802 subjects from these studies, 724 persons had Mini-Mental State Examination (MMSE) scores less than 24, or a decline of four or more points over two administrations, and were living in the community at the start of the MMCS. Each of the 512 subjects (71%) who consented to enrollment in the MMCS identified an individual who helped them most often with any daily activities and was most knowledgeable about the subject’s health status. These individuals also were asked to participate in the study and are referred to as the subject’s knowledgeable informant. Overall, knowledgeable informants were spouses (18.3%), adult children (45.0%), siblings (6.4%), other relatives (18.1%) or nonrelatives (12.3%) and lived in the same geographic area as the subject. Knowledgeable informants completed a baseline interview and three subsequent annual follow-up interviews, which consisted of the collection of demographics, general health information, and health service utilization information on the subject. In addition, the knowledgeable informant rated the subject’s behavioral and psychiatric symptoms based on the depression subscale of the Neuropsychiatric Inventory (NPI),
11 and the agitation and psychosis subscales of Behavior Symptom Rating Scale (BSRS).
12 Medicare records for each subject were available to corroborate data gathered from the knowledgeable informant. In case of discrepancy between the Medicare records and the knowledgeable informant’s report, the Medicare records were preferentially used.
Out of 512 subjects, 498 subjects were classified as either having no cognitive disorder (N=16), mild cognitive impairment (N=133) or dementia (N=349) using a validated diagnostic method based on a battery of four neuropsychological tests (Boston Naming Test, Word List Memory Test, Verbal Fluency Test, and the digit symbol subset of the Wechscler Adult Intelligence Scale—Revised).
13 A determination of dementia was made if the subject scored at or below a 2-point standard deviation from the mean for normal subjects of comparable age and education on at least two of four tests. A classification of mild cognitive impairment was made if the subject scored at or below a 1.5-point standard deviation from the mean on at least one test or scored at or below a 1-point standard deviation from the mean on two tests, and did not meet the criteria for dementia. Tests were administered in the same order to all subjects by trained interviewers. Participants diagnosed with probable dementia were further subcategorized based on their baseline MMSE score as mild (MMSE score: above 20), moderate (MMSE score: 11–20) and severe (MMSE score: 0–10) dementia.
13 Mortality was monitored for the following 3 years for these subjects through Medicare records and knowledgebale informant reports.
All statistical analyses were carried out with SPSS version 12.0 for Windows. Continuous data were expressed as mean values plus/minus standard deviations. We used analysis of variance to analyze continuous data, and the chi-square test for differences between categorical variables. The probability of survival was calculated using the Kaplan-Meier method, and survival curves were compared using the log-rank test. A p value<0.05 was considered statistically significant. Multivariate Cox proportional hazard regression models were used to identify independent predictors of all-cause mortality.
Variables investigated were: 1) age at initial interview; 2) ethnicity (dichotomous: white=0, nonwhite=1); 3) gender (dichotomous: male=0, female=1); 4) marital status (dichotomous: married=0, not married=1); 5) education (continuous; years of school); 6) general physical health rating (ordinal: rated by the knowledgebale informant as excellent, very good, good, fair, or poor); 7) heart disease (dichotomous: absence=0, presence=1 based on whether one or more of the following diagnoses was present: aortic aneurysm, arrhythmia, coronary artery disease, congestive heart failure, or valvular disease); 8) cancer; 9) stroke; 10) diabetes; 11) chronic obstructive pulmonary disease or asthma; 12) NPI-depression rating (as rated by the knowledgebale informant); and 13) BSRS psychosis and agitation rating by the knowledgebale informant; and finally, 14) MMSE score or level of cognitive impairment (ordinal: no cognitive disorder, mild cognitive impairment, mild dementia, moderate dementia, and severe dementia).
RESULTS
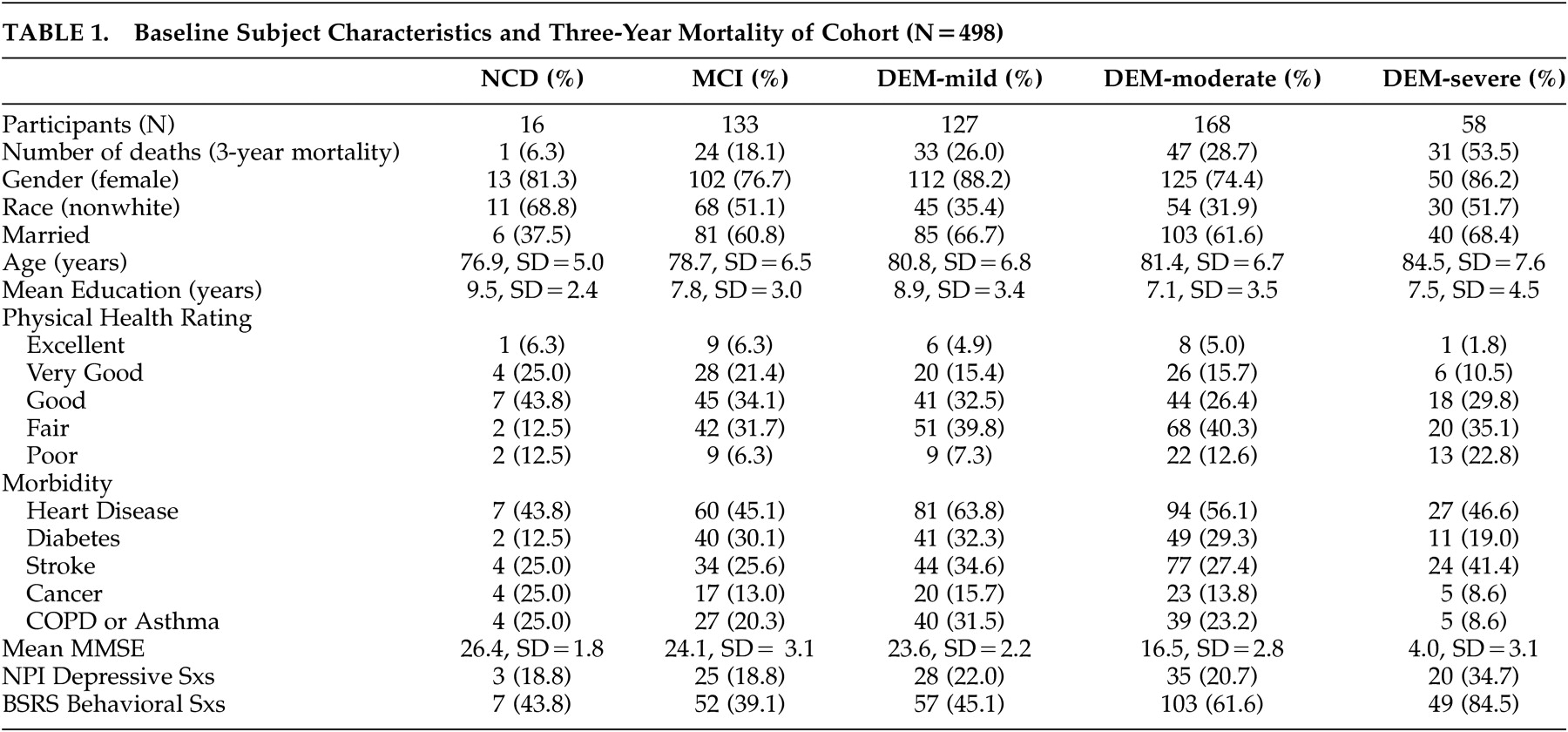
Demographic and clinical information are displayed in
Table 1 . A total of 136 subjects died during the period of analysis (October 1998 to October 2002; mean observation days: 1128 [SD=235] days). Their average age at the time of death was 83.1 (SD=7.5) years and the average time to death was 699.5 (SD=324.5) days after initial evaluation. The deceased included one participant with no cognitive diagnosis, 24 participants with mild cognitive impairment, and 111 participants with probable dementia. The cause of death based on the knowledgebale informant’s report and Medicare records were as following: cardiovascular or cerebrovascular events (40.1%), cancer (19.3%), infection (10.4%), physical complications of dementia (e.g., inability to swallow) (6%), kidney failure (3%), and unspecified causes (20%).
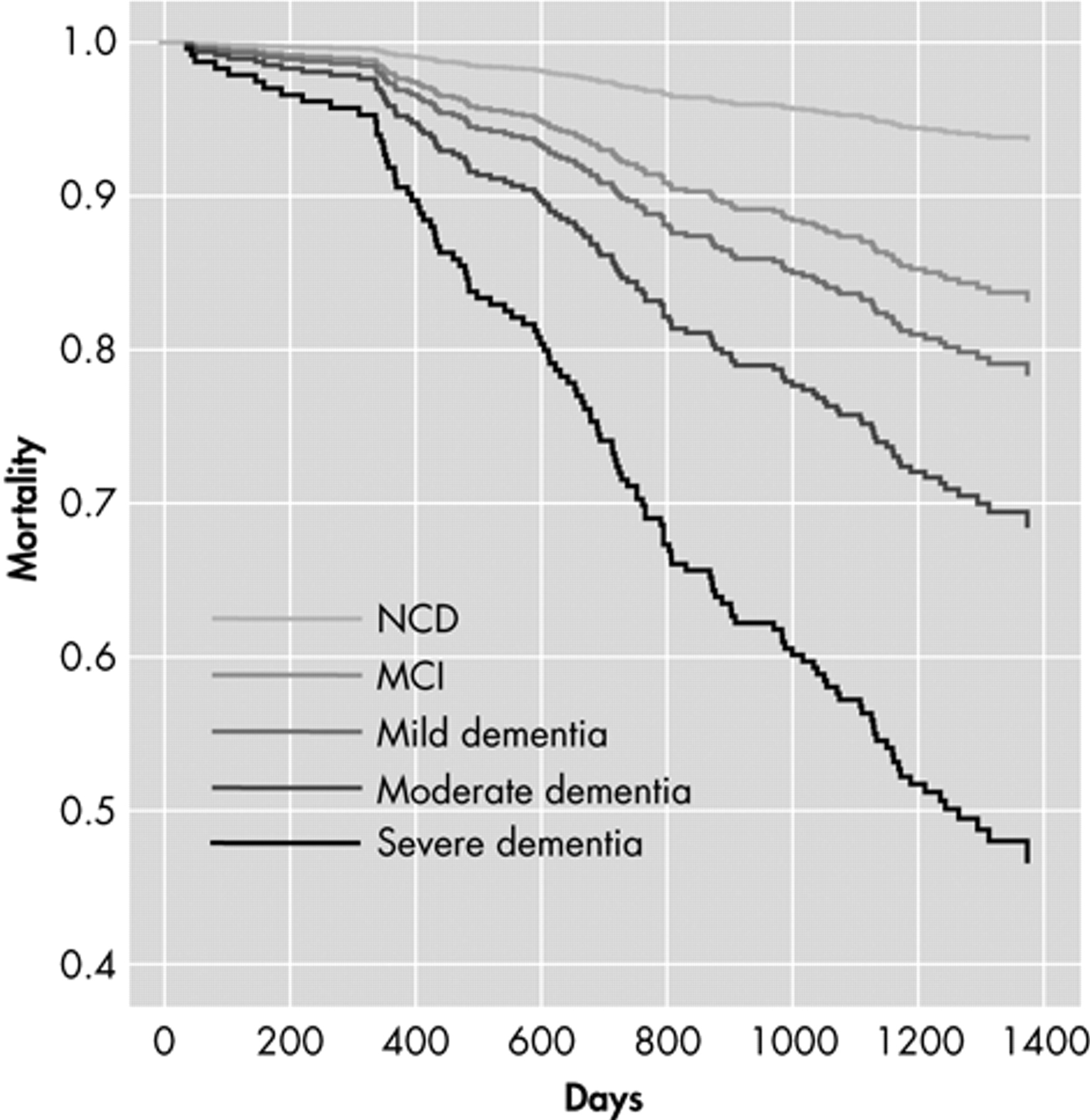
Kaplan-Meier survival estimates indicated higher mortality rates for those with more severe levels of cognitive impairment. Log rank test verified that the trend in mortality rates across the risk groups (no cognitive diorder, mild cognitive impairment, mild dementia, moderate dementia, and severe dementia) was statistically significant (chi
2 =30.87, df=4, p=0.0001). In the Cox hazard proportional model analysis that included all of the variables above, age (hazard ratio=1.05, 95% confidence interval [1.02, 1.08], p=0.001), gender (0.44 [0.27, 0.73], p=0.004), and MMSE (0.95, [0.92, 0.97], p=0.001) or level of cognition (1.512, [1.250, 1.852], p=0.001) were statistically significant. In contrast, measures of health and disease (physical health rating by the knowledgeable informant, presence of heart disease, stroke, diabetes, chronic obstructive pulmonary disease, asthma, and cancer) were not significant (p>0.05) as covariates. Cox regression survival plot for mortality by levels of cognitive impairment (
Figure 1 ) indicates that cognitive diagnosis is significantly associated with mortality among the participants.
DISCUSSION
In this analysis, all levels of cognitive impairment including mild cognitive impairment appeared to predict mortality among this community sample of elders. The presence of cognitive impairment measured by MMSE increased mortality in a graded fashion that parallels severity of cognitive impairment. This finding is consistent with previous studies that have reported the severity of cognitive impairment is predictive of mortality among the elders with dementia diagnosis
1 and extends the potential relationship to include elderly people with mild cognitive impairment.
Several methodological problems limit broad generalization of this study. First, the comparative group with no diagnosis of cognitive disorder was small (N=16) and does not represent the general population of elders without cognitive impairment. Second, the health-related variables may become more significant predictors in studies containing a larger sample size. Third, since participants were selected from a specific community, the results may not be representative of all elderly persons in the United States.
Nevertheless, this study suggests that measuring and categorizing the level of cognitive impairment with MMSE, a simple and popular cognitive assessment tool, is at least as useful in predicting longevity as the medical diagnoses in the community. Furthermore, even mild cognitive impairment seems to be associated with higher mortality among the elderly in the community. Future studies should examine the relationship between cognitive impairment and specific causes of mortality in order to identify preventive strategies to reduce mortality among cognitively impaired elderly persons.