To the Editor: Atypical antipsychotic drugs are widely used in the treatment of schizophrenia. These agents are discovered to have some additional benefits beyond their effectiveness as antipsychotic drugs. Among these initially unexpected effects are their potential effects as mood stabilizers in bipolar disorder and their efficacy in improving long-term outcome in schizophrenia. Neuroanatomical and neuroimaging studies of schizophrenia suggest that progressive neuropathological changes (such as neuronal atrophy and/or cell death) occur over the lifetime course of the disease.
1 Early intervention with atypical neuroleptics has been shown to prevent progression of at least some symptoms,
2 although the mechanisms by which neuroleptics may do this remain unknown. However, recent developments in basic neuroscience research suggest that atypical antipsychotics, with their potential to stimulate neuronal replacement and repair,
3 may also be promising in other neurodegenerative diseases. These effects recently raised the question as to whether these drugs may also have some neuroprotective effect in the brain. To examine this matter we evaluated the neuroprotective effect of olanzapine after permanent focal cerebral ischemia. Anesthetized adult male C57BL/6j mice (21g-25g) were submitted to permanent thread occlusion of the middle cerebral artery (MCA) using an intraluminal filament technique.
4 The rectal temperature was maintained between 36.5 and 37.0°C using a feedback-controlled heating system. The cerebral blood flow was measured by Laser Doppler Flowmetry (LDF) which was declined as to ∼15% of preischemic control levels immediately after thread insertion in all animal groups. Olanzapine (0.1 mg/kg and 10 mg/kg) or vehicle was applied intraperitoneally just after permanent ischemia.
Twenty-four hours after permanent ischemia, the area of infarction was measured by 2% 2,3,5-triphenyltetrazolium chloride (TTC) staining. This study was interesting with regard to poststroke depression, which is seen in about 20%–40% of all patients,
5 whereas a mood stabilizator with neuroprotective property would be preferable. However, with regard to controversial results about the increased rate of cerebrovascular events in patients who are under the treatment of atypical antipsychotics,
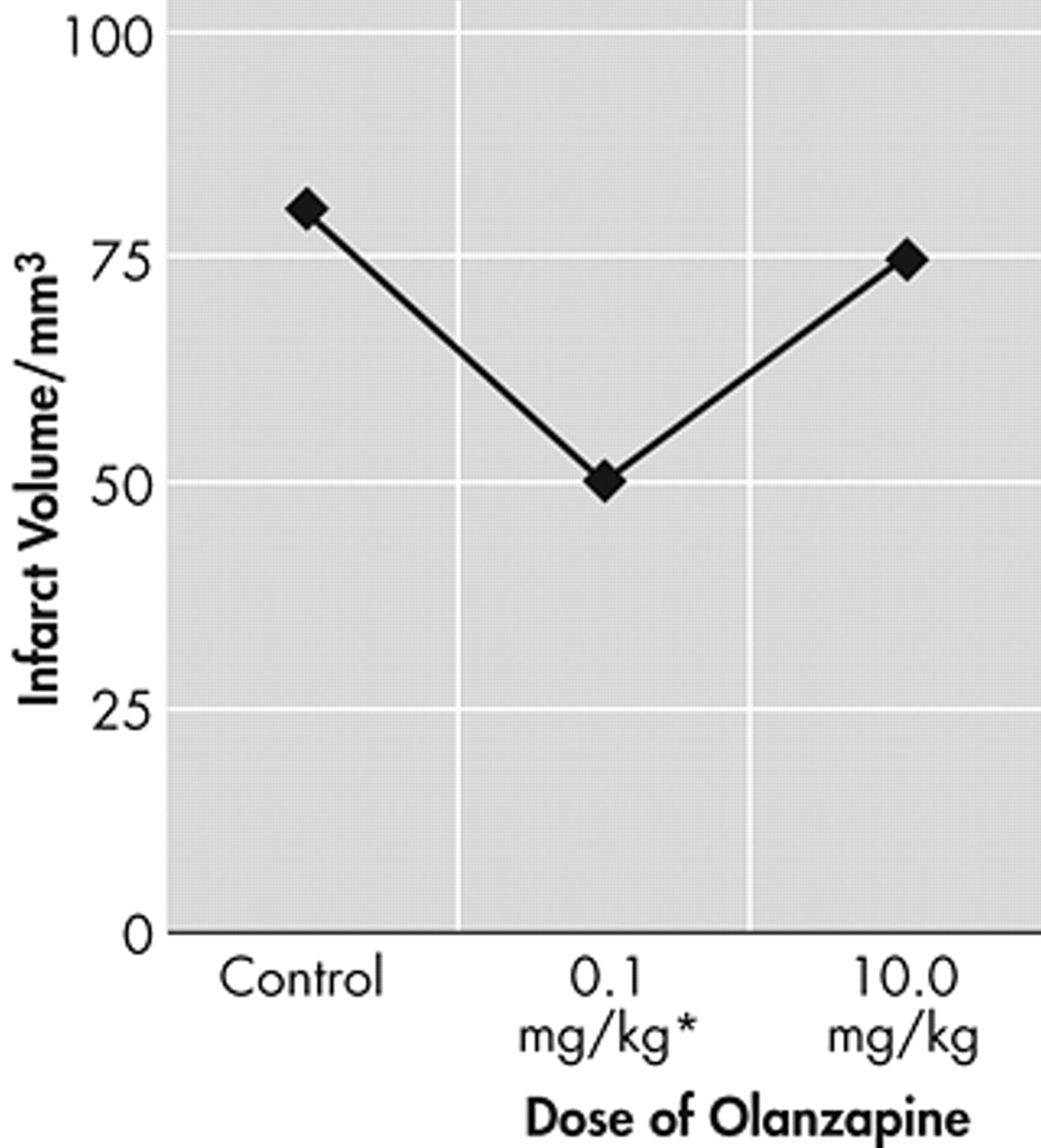
6 a safety treatment modality is also very important. Olanzapine showed (at 0.1 mg/kg) a significant neuroprotection (p<0.05, ANOVA analysis followed by LSD tests) after permanent focal cerebral ischemia whereas the 10 mg/kg was not neuroprotective or neurotoxic (
Figure 1 ).
It is difficult to estimate what caused the decrease of neuroprotective effect of olanzapine at its higher doses. It can be hypothesized, however, that the anticholinergic activity which increases with the higher doses of olanzapine could have restricted the neuroprotective activity of olanzapine. Moreover, the limited size of penumbra could have an additional restrictive effect on neuroprotection. In summary, this study indicates that even by a serious brain injury model olanzapine is not a neurotoxic agent and could exert, in specific dose range, a significant neuroprotective effect. However, further experiments to evaluate the long-term clinical reflections of such neuroprotective effects of atypical neuroleptics in bipolar and schizophrenia patients via MRI and spectroscopy studies would be the logical future step in the field of psychiatric research.