To the Editor: Catatonia is a movement disorder defined primarily by a cluster of signs including immobility, mutism, and withdrawal or refusal of food and water,
1 and its presence in the elderly patient can lead to rapid medical decompensation necessitating rapid and effective treatment for this condition. Catatonia may arise from GABA-
A hypoactivity, dopamine (D
2 ) hypoactivity and possibly glutamate
N -methyl-D-aspartic acid (NMDA) hyperactivity.
2 Ms. A, an 80-year-old female, was admitted to a geriatric psychiatry residential unit presenting with depressive symptoms. She had been a widow for 3 years and was brought to the hospital at the request of her four sons because they felt that she could no longer care for herself. The patient had no prior episodes of depression or any other psychiatric disorder.
Her medical history was significant for hypertension, pacemaker placement, chronic renal failure, hiatal hernia, and gastritis. She was being treated for cognitive dysfunction. Medications prior to admission were enalapril, 20 mg/day, memantine, 10 mg/day, zolpidem, 10 mg/day, risperidone, 0.5 mg/day, and omeprazole, 20 mg/day.
A clinical and neurological exam showed no additional findings. Laboratory studies did not reveal significant abnormalities, creatinine was 1.2 on admission and remained at 1.1, and BUN was 41. CT of the brain was performed without contrast and revealed decreased attenuation consistent with chronic ischemic changes of the white matter.
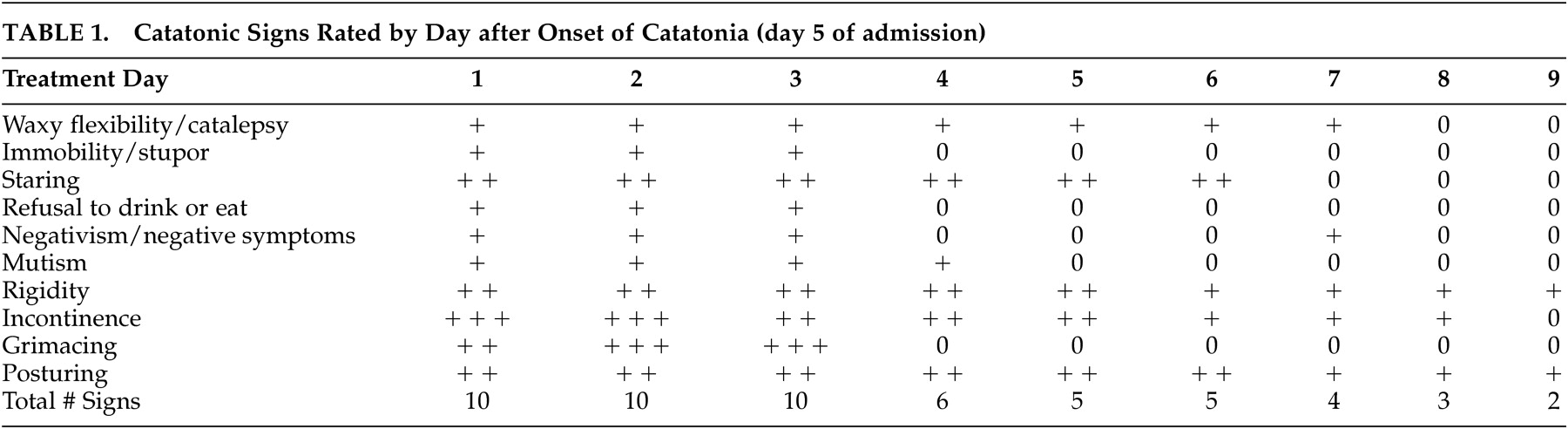
Five days after the admission she developed negativism, mutism, and akinesia, made no eye contact with others, and had perioral dyskinetic movements, waxy flexibility, and catalepsy (
Table 1 ). After clinical evaluation at 5 days after the admission, lorazepam, 2 mg i.m., and memantine, 5 mg p.o., were given. The patient responded quickly and gave coherent responses to what was asked, walked and interacted with other patients, and was able to take care of herself. Risperidone and zolpidem were discontinued at this point. However, this improvement lasted for 24 hours but once again catatonia returned. The dose of lorazepam was changed to 2 mg i.m. b.i.d. and memantine to 7.5 mg p.o. b.i.d.
Gradual improvement in catatonic signs was seen with reduced severity of some signs and a 50% reduction in catatonic signs by the 5th day of treatment (
Table 1 ).
Two weeks after admission the patient was free of most catatonic signs and symptoms. In addition, she was alert, fully oriented, and without significant evidence of cognitive dysfunction on mental status exam. Lorazepam was converted to 3.75 mg p.o. b.i.d. and memantine to 7.5 mg p.o. b.i.d. The patient remained on this medication regimen for 1 year without the return of significant catatonic signs or symptoms.
This patient’s presentation for major depression was complicated by catatonia. She had cerebrovascular disease which may have contributed.
3 However, the treatment of major depression with catatonia in this case is interesting because of the combined use of lorazepam, a GABA
A promoter, and memantine, an NMDA antagonist.
2 We feel that this case may suggest a useful treatment approach for major depression with catatonic features.
4