Procedure Efficacy
Previous anterior capsulotomy techniques produced a relatively high incidence of side effects, possibly as a consequence of larger lesions.
20,
21 Aiming to improve results and reduce side effects, smaller and standardized capsulotomy lesions were developed (the VC/VS gamma capsulotomy).
8 This improved procedure is based on a more precise target definition within the internal capsule, employing smaller collimator sizes (4 mm), consequently aimed at producing smaller lesions albeit not compromising efficacy.
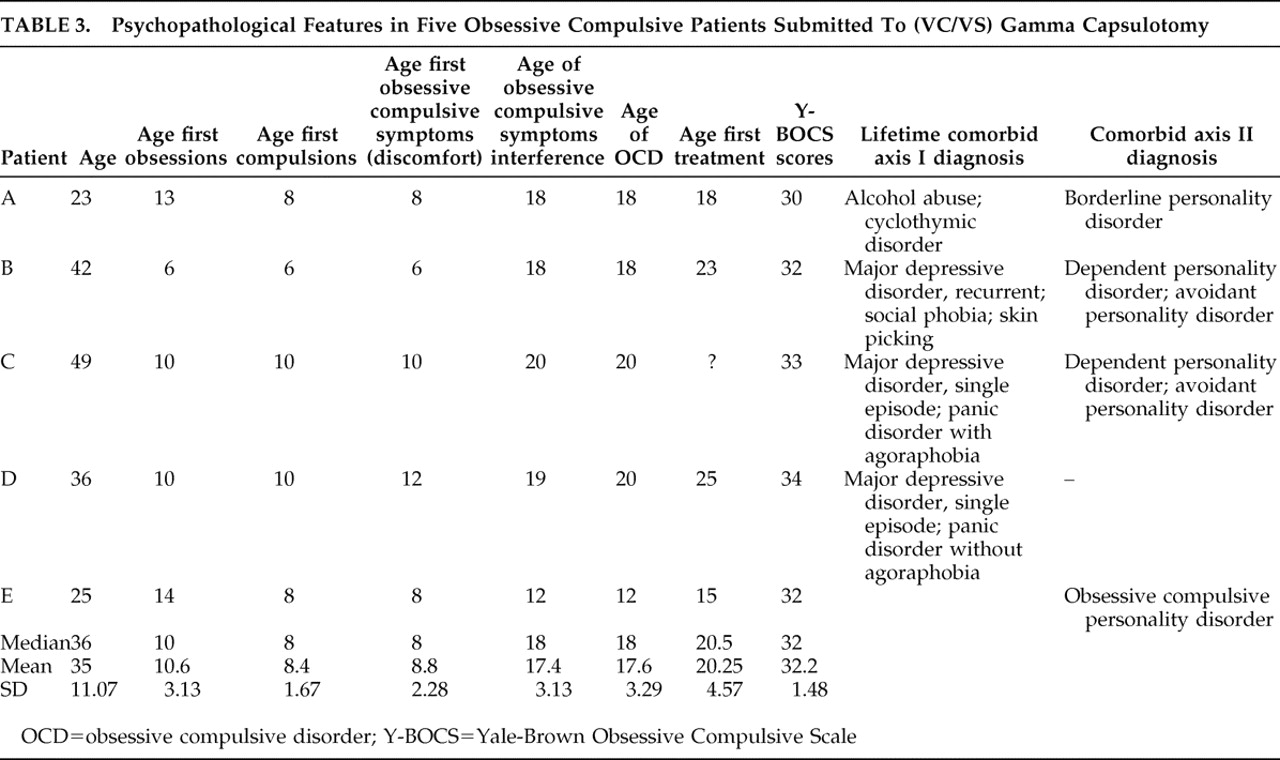
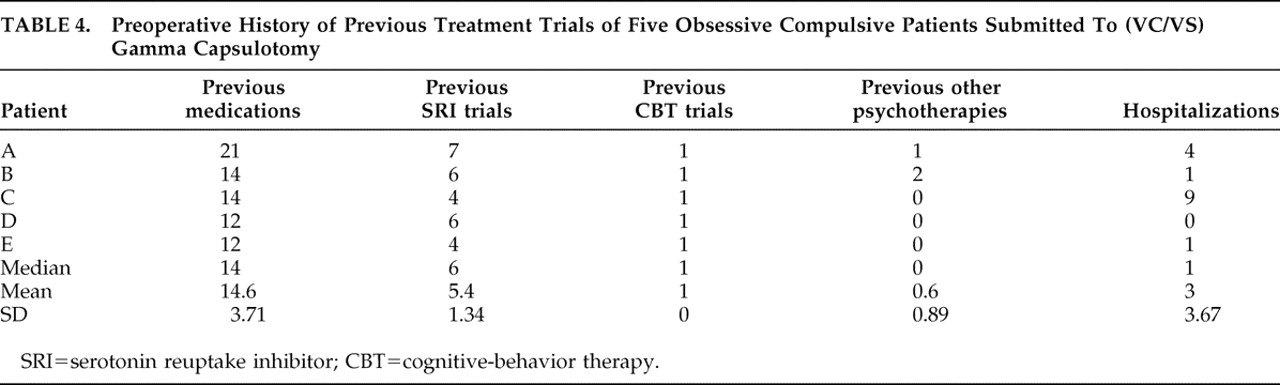
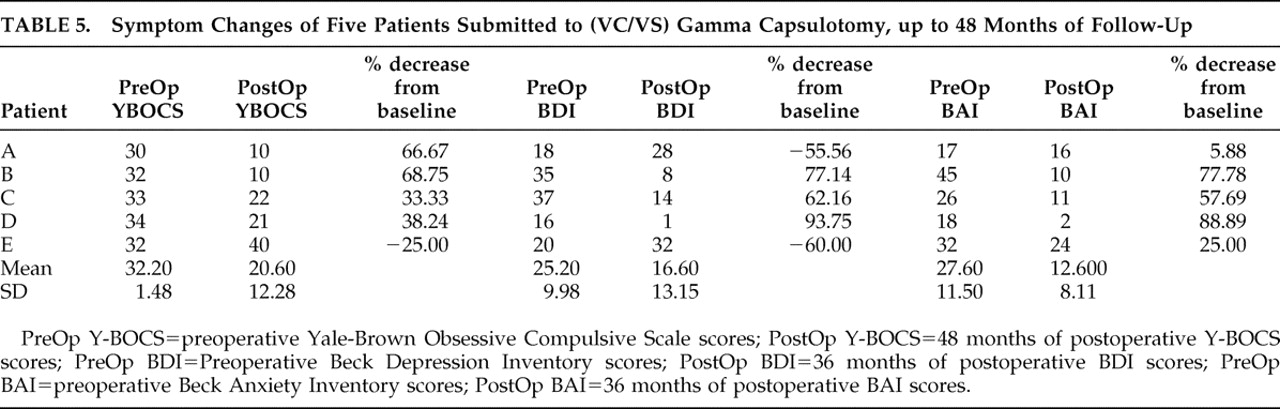
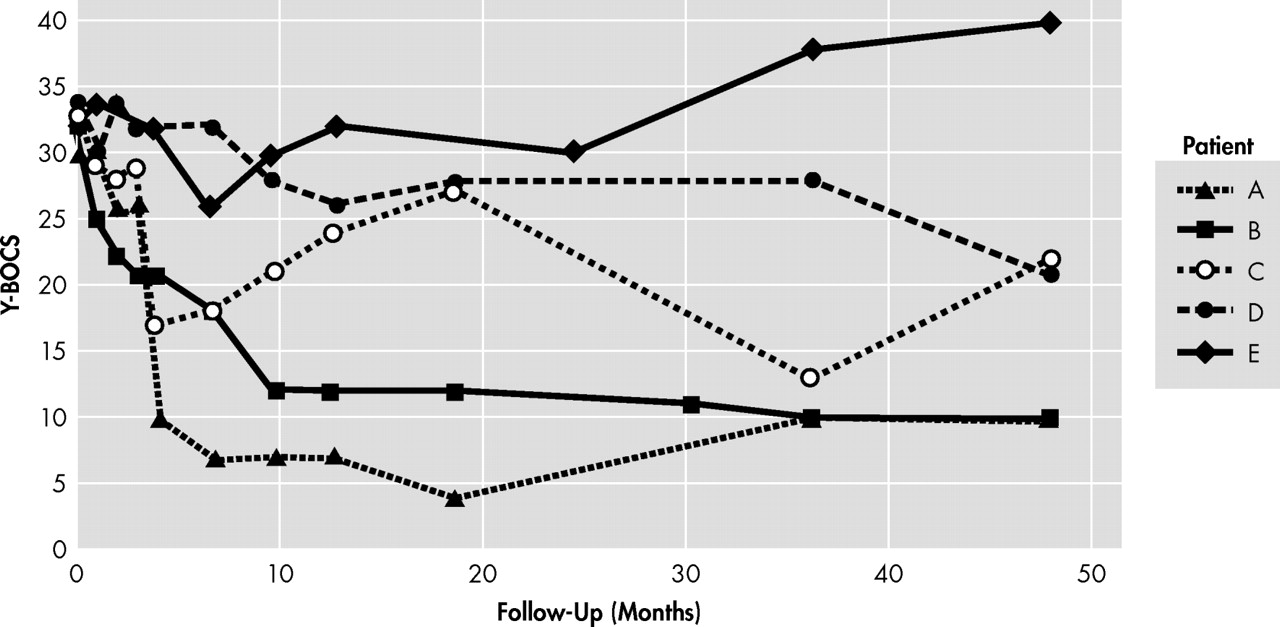
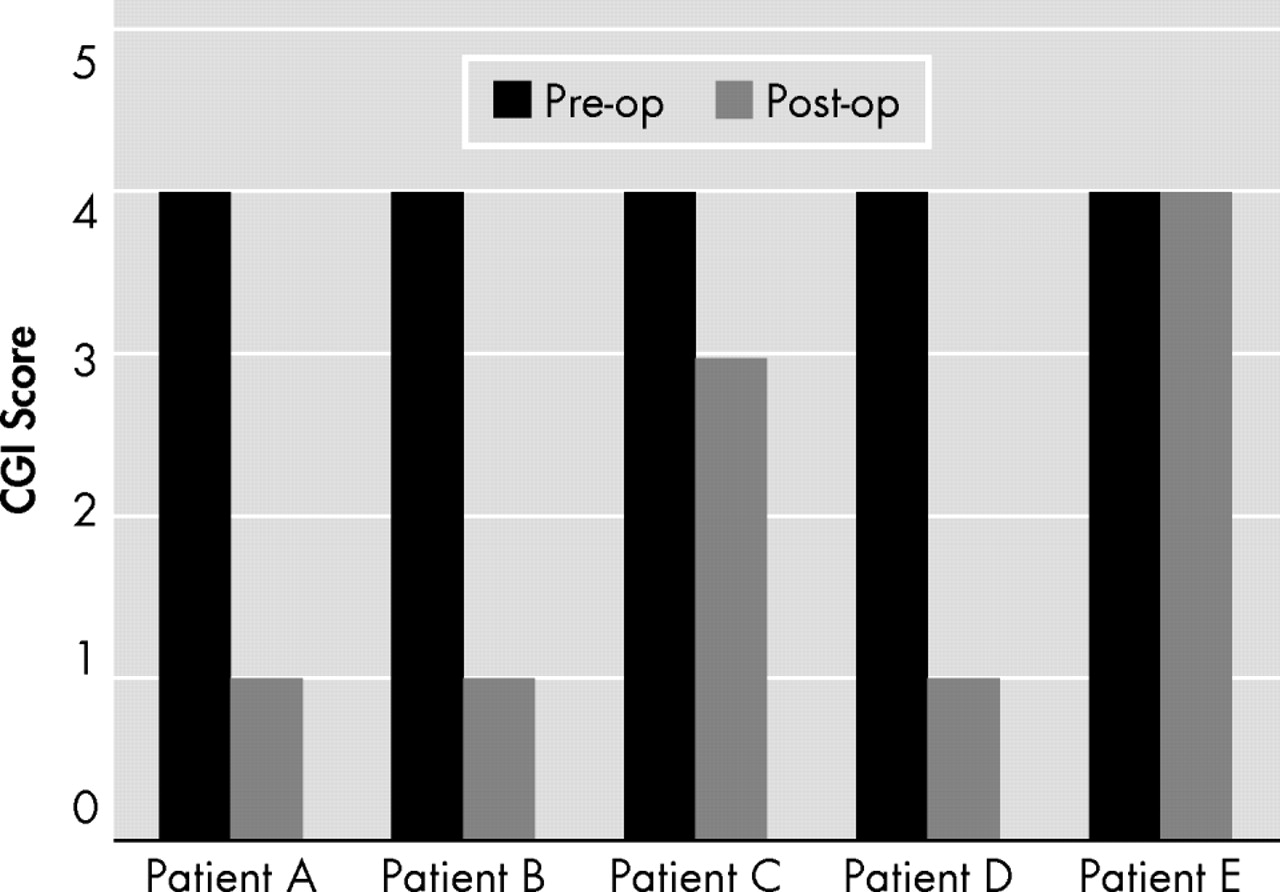
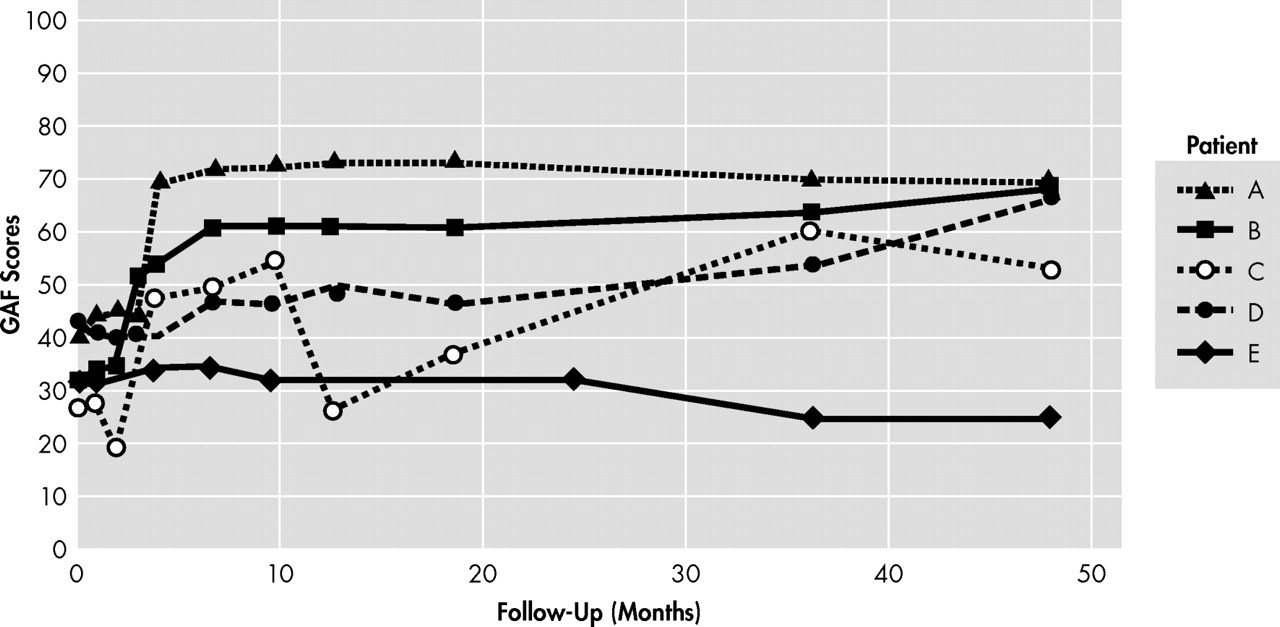
Our preliminary findings suggest that this procedure holds promise for selected severe and treatment resistant OCD patients. Among the five patients enrolled in this study, at the end of a 3-year follow-up period, three (60%) presented full response after surgery (67%, 69% and 38% reductions in Y-BOCS severity), and one had a partial response (33%). On the other hand, the one patient who was a nonresponder to surgery also developed worse OCD symptoms in the long-term follow-up, though maintaining his previous psychosocial impairment.
The three patients who improved the most and the partial responder showed markedly increased personal autonomy and reintegration into society, in addition to relief of persistent subjective distress.
Although comparison across studies is limited for methodological reasons (see Greenberg et al.
22 for discussion), clinically significant improvement after larger capsulotomy lesions (including an earlier gamma capsulotomy technique) was previously reported in five out of nine patients (55%) and seven out of 10 patients (70%).
6,
7 These rates are comparable to ours (3 out of 5 patients or 60%). However, we used more stringent response criteria. Previous studies were less rigorous regarding OC symptom amelioration and did not include measures of global improvements (such as CGI scores). Analyzing data from previous Gamma Knife techniques, but response criteria similar to ours, Rück
21 described response rates similar to ours (five out of eight patients, 62.5%).
The delayed amelioration of symptoms observed in our study could result from multiple sources and even be unrelated to the surgery. However, the latter interpretation is less likely, since OCD in the overwhelming majority of our patients was a chronic illness (mean OCD duration of 17.4 years), unresponsive to multiple conventional treatment schemes.
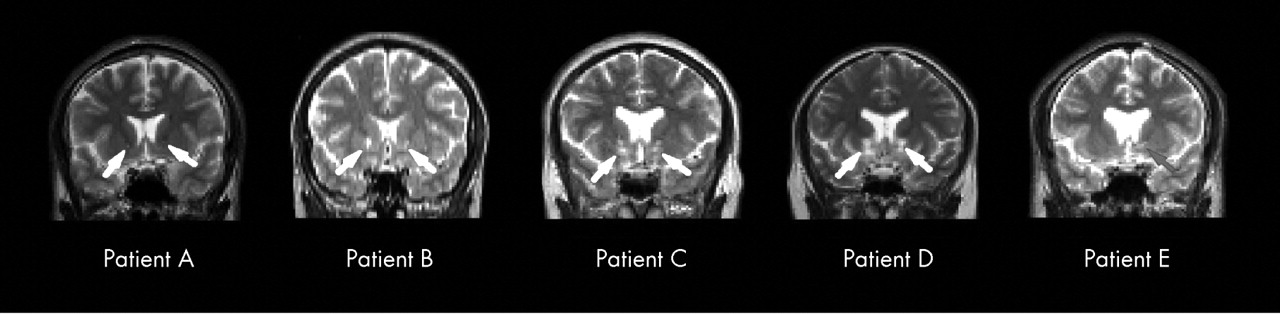
It remains unclear how gamma capsulotomy lesions result in OCD symptom improvement. One hypothesis is that bilateral lesions of the anterior capsule could alter information flow in thalamo-orbital and thalamo-cingulate neuronal circuitry (particularly the subgenual cingulate), which is related to the pathophysiology of OCD, and thus be involved in the changes in OCD symptoms observed after surgery. Interestingly, functional imaging data from a small cohort of patients with severe anxiety disorders undergoing this type of neurosurgery showed reduced activity within medial orbitofrontal cortex after the intervention.
22,
23In addition, edema and necrosis produced by gamma radiation surrounding the targets may compromise the adjacent striatum
24 and nucleus accumbens. Therefore, it is possible that additional cortico-striato-pallido-thalamico-cortical circuits are interrupted, especially those involving the ventral striatal-pallidal system and the extended amygdala.
25 –
27It is unknown whether unilateral lesions would be as efficacious as bilateral targeting. One previous MRI study of anterior capsulotomy for OCD suggested that appropriate lesioning of the right anterior capsule
might be critical to subsequent therapeutic response.
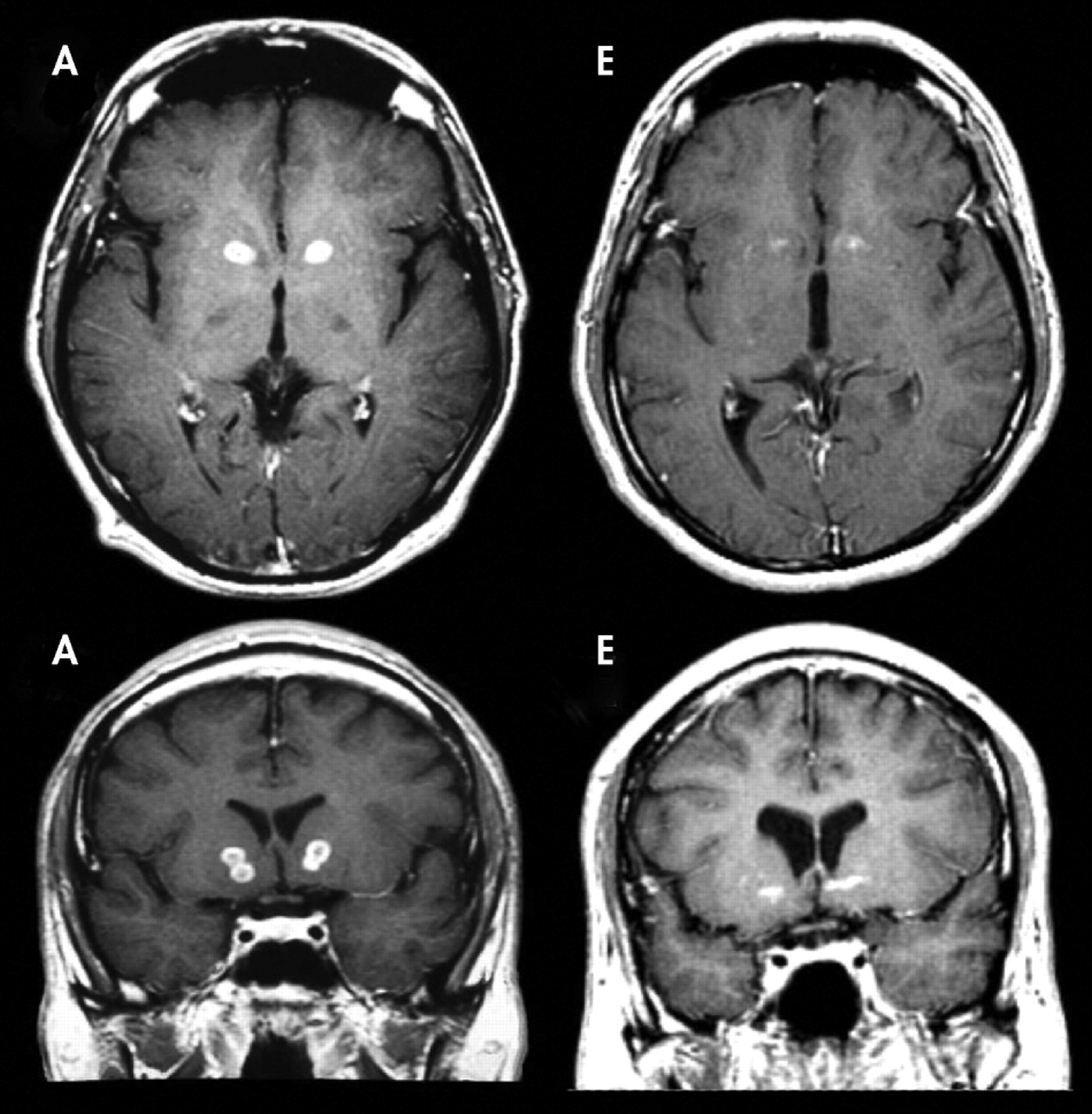
7 It is noteworthy in our study that the only patient who did not show any clinical response to surgery had a minimal left anterior capsule lesion, whereas all the other patients showed clear bilateral lesions.
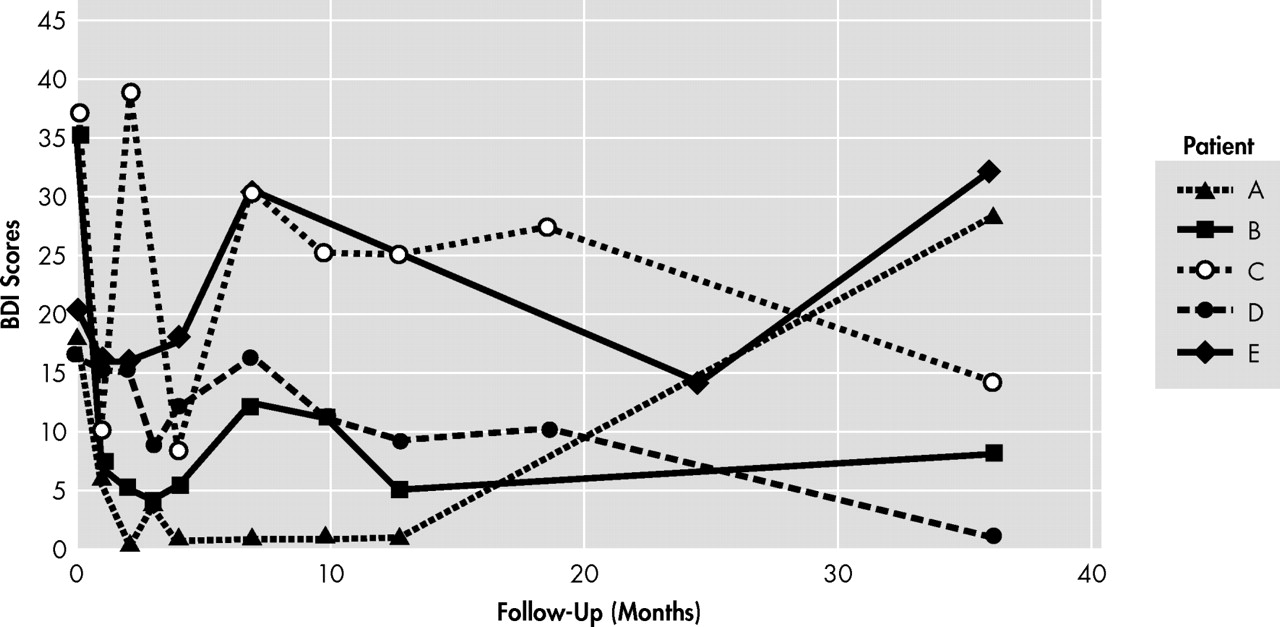
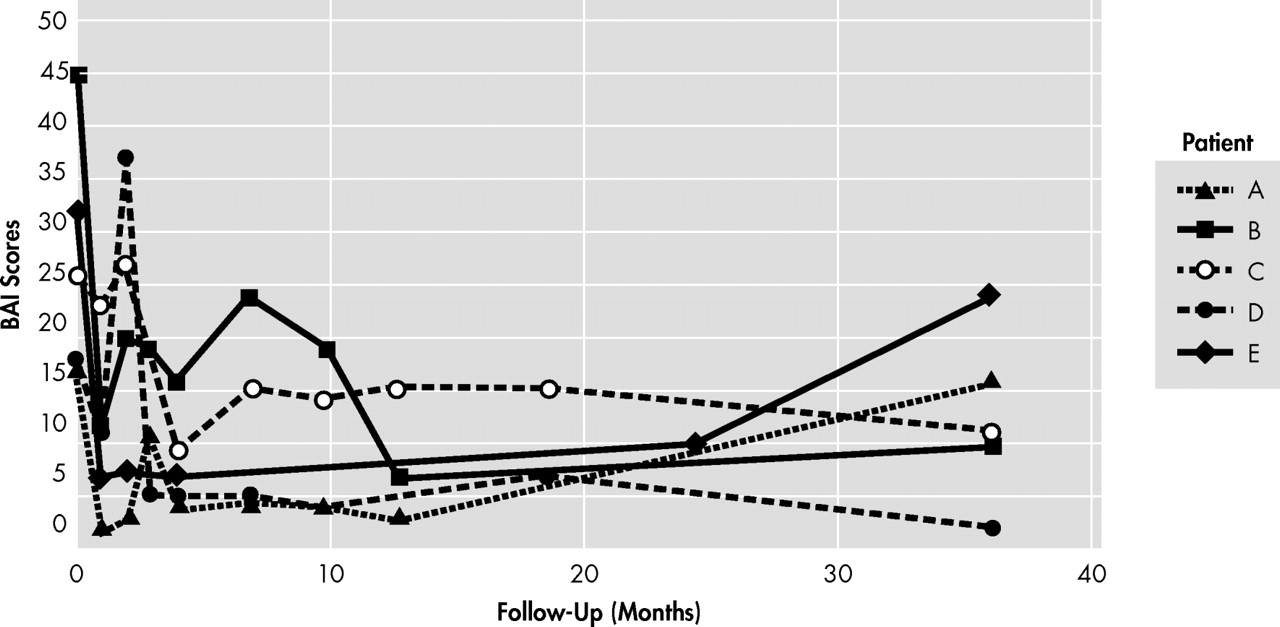
It is not surprising that most of our patients also reported postoperative reductions in anxiety and depression scores. Anxiety disorders and refractory depression have been successfully treated with anterior capsulotomy by thermolesion.
28,
29 In our sample, persisting reductions in anxiety scores were more prominent than reductions in depressive symptoms (mean reduction of 15 score points or 54%, versus 8.6 score points or 34%). Patient A presented with worse scores on BDI and BAI in his last follow-up visit, and this may be attributed to his inadequate compliance with medications. He nonetheless maintained low Y-BOCS scores. Patient E, a treatment nonresponder, showed marked worsening of BDI and BAI scores, and OCD symptoms deteriorated. Therefore, it is possible that the improvement in anxiety and depressive symptoms by surgical intervention may contribute to the amelioration of OCD symptoms directly or indirectly, although not explaining the maintenance of low Y-BOCS scores in the postoperative follow-up period.
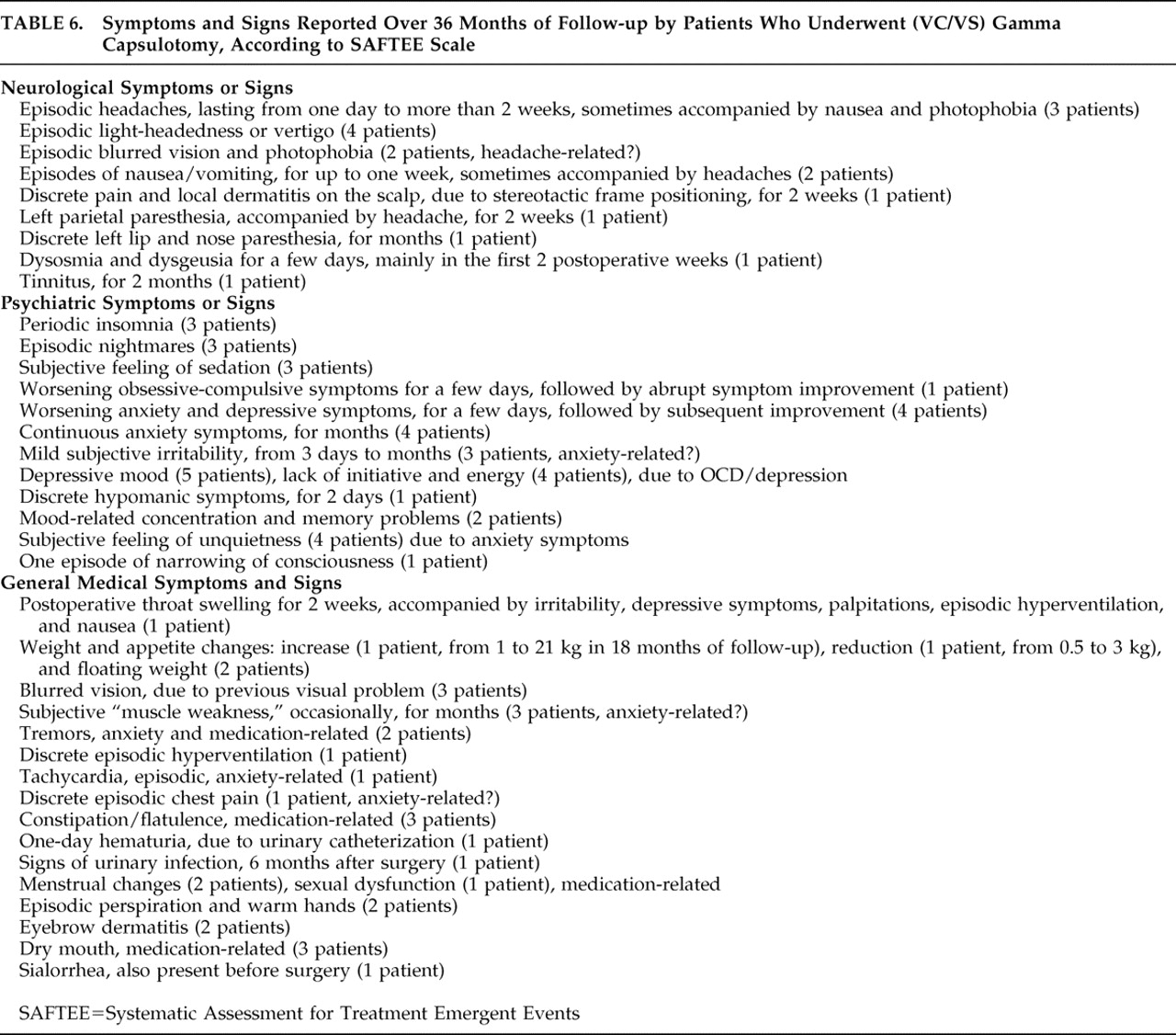
General Medical and Neurological Adverse Events
According to the SAFTEE scale, most adverse events were transient, not interfering with functioning or requiring treatment or hospitalization. Only headache, in one patient, lasted more than a few weeks. In this only case with persistent headache (around 2 weeks’ duration), no evidence of brain swelling was found on MRI, although the patient was empirically treated with corticosteroids for a few weeks. None of these initial symptoms persisted 36 months after surgery. However, it is still early to draw definite conclusions regarding potential long-term adverse effects.
Some of the symptoms and signs assessed by the SAFTEE scale may be attributed either to the direct effects of radiation, or to the effects of anesthesia and head positioning in the Gamma Knife equipment or even be unrelated to surgery. Headaches, nausea, vertigo, weight changes, postoperative throat swelling, 1 day hematuria, local dermatitis, and discrete pain on the scalp were probably related to the surgical procedure. Even though weight changes were common in four patients, only one patient (C) developed a considerable weight gain. Most side effects were mild and lasted for only a few days. We suppose that other symptoms/signs may or may not have been related to surgery.
A less favorable profile of adverse events was reported in previous radiosurgical studies using larger targets.
21,
29 Rück
21 reported the results of nine patients with OCD submitted to Gamma Knife capsulotomies. Three to four bilateral isocenters and 4 mm collimators were used for lesions in five patients, delivering more than 200 Gy at the center of the lesion on each side.
21 Frontal lobe complications were evident in two patients, as well as urinary incontinence and seizures. It is unclear, however, if this was due to larger lesion volume, higher doses, and/or different targeting.
Limitations
This pilot study has several limitations. First, it included a small cohort and used an open design. Second, as patients came from regions distant to the study site, some follow-up data were obtained only by telephone interview (especially at 48 months of follow-up). For the same reason, postoperative MRI scans schedule was different among patients (range=9 months to 24 months postsurgery). It was not possible to control for medication changes. Furthermore , patient C presented a quite variable clinical course over the 48 months of follow-up, demanding further assessment to reassure her response condition. Finally, neuropsychological and personality changes associated with this surgical procedure are not provided in this article, but they will be described in other publications.