D reaming has been defined as a mental activity characterized by vivid sensorimotor imagery that is experienced as waking reality despite such distinctive cognitive features as impossibility or improbability of time, place, characters, and related actions.
1 Such features have been grouped under the term cognitive bizarreness, a structural property of dreams that seems to distinguish it from other types of physiological mentation.
As far as pathological forms of mental activity are concerned, several clinical aspects of psychosis have been extensively related over time to various aspects of the subjective experience of dreams,
2 –
4 and various lines of research seem to indicate that dreaming and psychosis share some common neurobiological substrates.
5 –
7 As a result of these observations, the dreaming mind-brain has been proposed as an experimental model for psychosis.
7,
8 Several authors have interpreted this similarity in terms of a primary form of mental expression found in dreams and psychosis that can be understood by analyzing formal aspects of thought processes.
9,
10 In an experiment specifically designed to test this hypothesis, we were able to demonstrate that cognitive bizarreness is equally high in the dream and waking mentation of actively psychotic schizophrenia patients and in the dream mentation of a control population
11 : these results suggest that the functional organization of the psychotic mind mimics that of the dreaming mind in some way.
Bizarreness in dreams has been interpreted as a phenomenological aspect of a specific activation pattern occurring in the cholinergic system during REM sleep, where dream imagery is more vivid and story lines more articulate and incongruous.
1 Increases in cholinergic firing have been extensively correlated to REM sleep, whereas the role of dopamine in this stage remains unclear, though some experimental data seem to point to a complementary dopaminergic activation in the mesolimbic and mesocortical systems.
1,
12 –
13 Parkinson’s disease is a neurodegenerative disorder that is currently thought to involve an imbalance in several neurochemical pathways, most prominently the dopaminergic and cholinergic systems in the striatum.
14,
15Within this framework, it seems useful to assess cognitive bizarreness in the dream and waking mentation of patients with Parkinson’s disease, with reference to possible implications of the dopaminergic-cholinergic interaction in dreaming and in the waking cognition of this population.
In summary, the objectives of this study were to determine cognitive bizarreness in the dream and waking mentation of Parkinson’s disease patients without psychotic symptoms relative to a comparison population and to determine whether doses of dopaminergic drugs correlate with the level of cognitive bizarreness expressed in the dream and waking mentation of the patients.
METHODS
Participants
Twenty patients with a diagnosis of idiopathic Parkinson’s disease were selected at the Parkinson Institute of the Istituti Clinici di Perfezionamento Hospital in Milan, from September 2007 to September 2008. Exclusion criteria were a Mini-Mental State Examination (MMSE) score below 24, the presence of psychiatric disorders (DSM-IV-TR criteria), a score of 3 or more in three Symptom Checklist—90 (SCL-90) subscales (obsessive-compulsive, psychoticism, paranoid ideation), a significantly impaired motor function for reasons other than Parkinson’s disease, and a duration of disease longer than 15 years. The MMSE score of at least 24 was used in order to exclude patients with moderate and severe cognitive impairment. The SCL-90 was administered in order to rule out subthreshold psychiatric symptoms such as compulsive behavior and psychosis that have been extensively described in patients treated with dopaminergic drugs.
16 A group of 20 healthy comparison subjects were selected in the general population in order to match the pathological group in terms of age, sex, and education. Exclusion criteria for healthy participants were alcohol and substance abuse, the presence of any neurological or psychiatric disorder, or any other medical condition that may cause psychiatric symptoms. All participants were unpaid volunteers, and informed consent was obtained after full explanation of the study purpose and design.
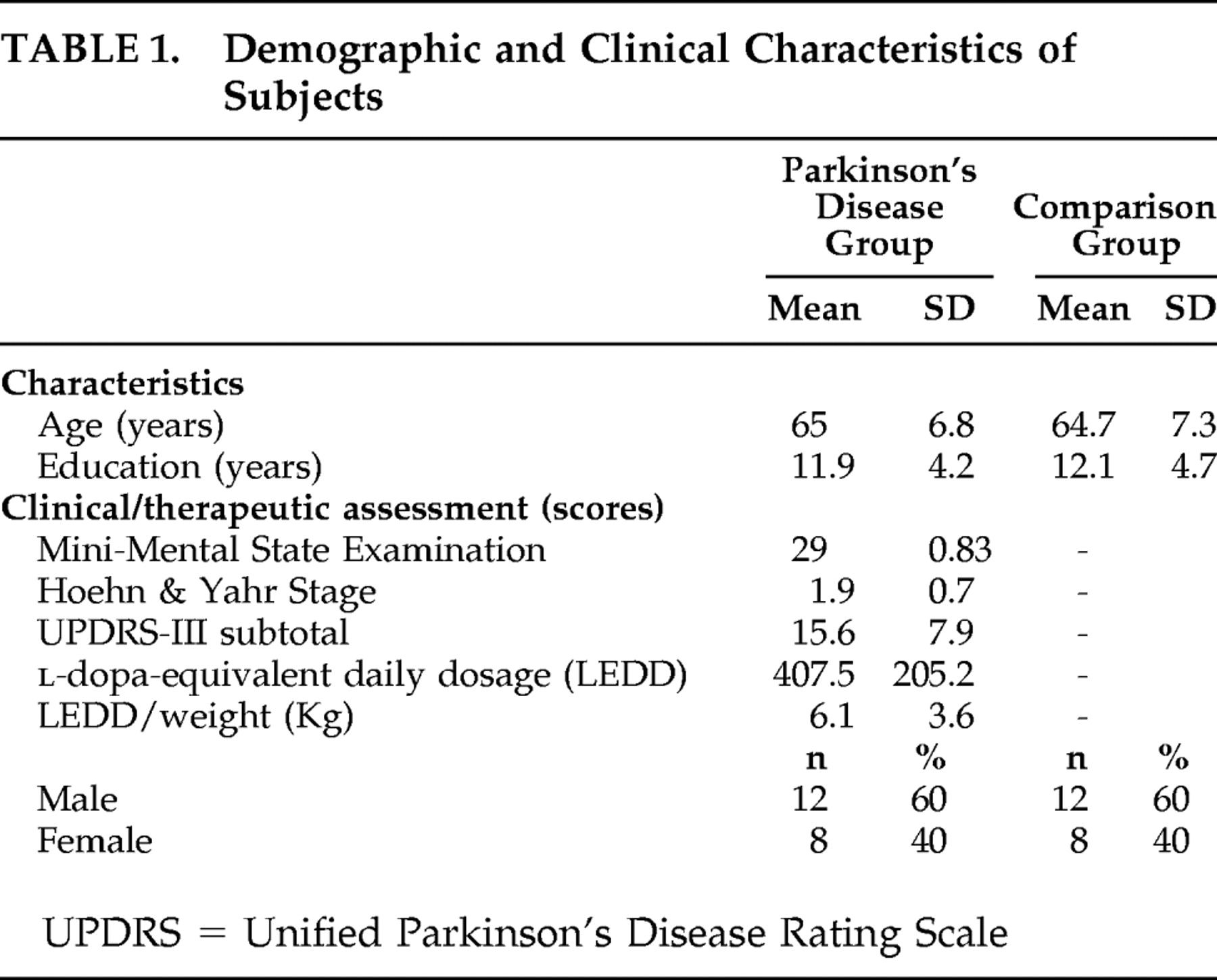
Table 1 shows a summary of the demographic characteristics of the two samples and of the clinical and therapeutic patterns of patients in treatment with prodopaminergic drugs. We performed a clinical assessment in the Parkinson’s disease group using the Unified Parkinson’s Disease Rating Scale (UPDRS)
17 and the Hoehn & Yahr Staging of Parkinson’s Disease
18 ; UPDRS-III scores were generally low, as confirmed by the mean Stage Two of the Hoehn & Yahr assessment. The mean
l -dopa equivalent daily dose divided by the mean weight of patients in the Parkinson’s disease group are also reported, with
l -dopa equivalent daily dose values having been calculated for each participant according to standardized criteria.
19Thematic Apperception Test
The Thematic Apperception Test (TAT) is a projective test widely acknowledged as one of the most useful psychodiagnostic tools in clinical settings, consisting of a broad set of figures, differentiated into groups of 20 according to sex and age.
20 Each figure of the test shows an enigmatic interaction among people, depicting various types of contexts from concrete real-life to slightly surreal situations. Usually, only some of the figures are administered for the test, and seven—chosen progressively from the full set—were used in this study according to a previously published scheme.
11 Participants were handed one card at a time and asked to create a fantasy story that clearly contained a beginning, a plot development, and an end based on the visualized figure. An important part of the instructions was to look at the figure for no longer than 5 minutes and then turn the card over in order to eliminate the stimulus upon responding; the narratives the participants created in response to the fixed stimulus were tape-recorded and then transcribed:
F, a 65-year-old female comparison subject (shown figure 6gf, showing a woman turned toward a man behind her), said the following:
Brother and sister. She listens incredulous as he tells her that their old horse…of which both are very fond…that had disappeared 2 days before, was stolen by their neighbor, the spoiled and careless son of a couple of friends. She asks herself, how will they ever be able to get the horse back: it would be a great mistake for the parents to be told their son is also a thief! They are talking about it. He suggests they face the problem openly with the boy himself, hoping he will give the horse back acknowledging their tact.
This example clearly shows the development of a brief, imaginative story containing an interactive plot among characters. Whereas in clinical settings this verbal production would be interpreted in terms of peculiar aspects emerging from its contents, such as the subject’s needs or identification with the characters,
21 in our experimental setting the material was used for the formal analysis of thought processes.
Dream Collection
All participants were instructed to keep a dream log where they could report each morning the dream they had had the night before. We usually collected the written material within a month of the first interview in which the TAT was administered.
Table 2 shows a comprehensive view of the material collected in our sample.
Scoring Bizarreness
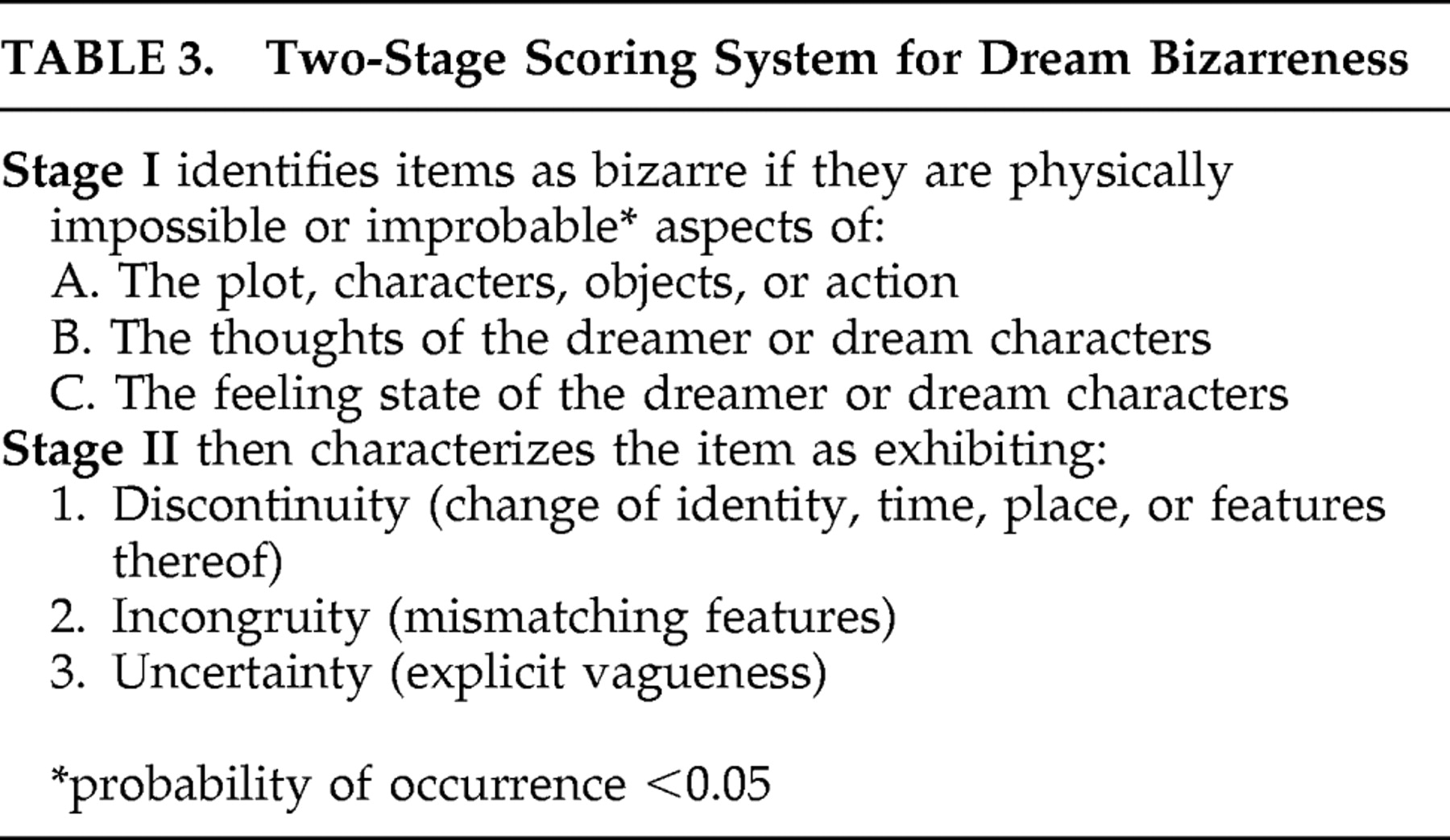
The standard criteria for measuring bizarreness are shown in
Table 3 and the scoring procedures are extensively reported elsewhere.
11,
22 In brief, two highly trained judges from our group with an interrater reliability coefficient of 0.92 for the TAT reports and 0.89 for the dream reports
11 scored the material according to the dream bizarreness scale as shown in the following example:
AA, a 57-year-old male patient affected by Parkinson’s disease [dream excerpt] said the following:
Looking at the water of the aquarium I realize there is a green fish, as large as a trout, dead. This fish was very strange, it was inside out (A2), it was not tapered but flat (A2), with a green-blue eye. There were also many fries, around 40 newborn little fish. There was a well-known blind grandpa (A1) who gave suggestions on how to manage the aquarium, and he himself had never seen such a thing.
For each dream and TAT response, the density of bizarreness was calculated by dividing the number of bizarre events by the report’s number of words. We then calculated two indexes for each participant: the Bizarreness Density Index (BDI) for dreams calculated as the mean density of bizarreness found in the subject’s dreams and the BDI for TAT tables calculated as the mean density of bizarreness found in the subject’s TAT reports. We finally calculated the square root of the BDIs to normalize data distribution.
In order to assess the effect of diagnosis and experimental conditions (TAT stories and dream reports) on bizarreness, we applied a two-way analysis of variance (ANOVA) for repeated measures
23 with diagnosis as the independent variable and the experimental conditions as the within-subject factor. Employing this type of analysis we were able to independently estimate the effects of diagnosis and test conditions and the interaction between them. Pearson regression was applied to correlate measures of bizarreness in the dream and waking cognition of Parkinson’s disease patients with an index of their motor disability (UPDRS-III) and with their
l -dopa equivalent daily dose per kg indexes.
RESULTS
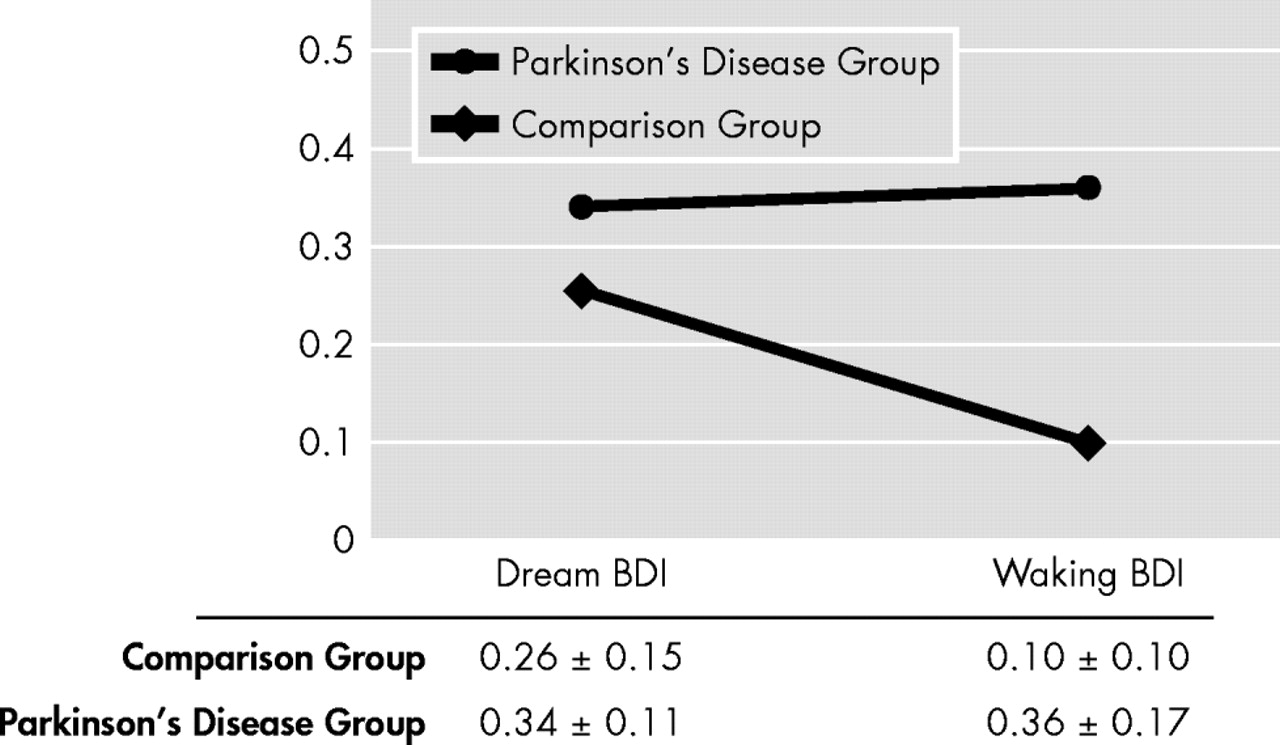
Figure 1 shows the means of the dream and TAT BDI values in patients with Parkinson’s disease and healthy comparison subjects. Analysis of the data revealed the following:
(a) The effect of the experimental conditions (i.e., TAT and dream reports) was significant (F=5.061, df=1, 38, p=0.030).
(b) The effect of diagnosis was significant: BDI was higher in patients with Parkinson’s disease than in healthy comparison subjects (F=33.232, df=1, 38, p<0.05).
(c) The interaction experimental conditions by diagnosis was significant (F=9.046, df=1, 38, p=0.005): The two groups show roughly the same level of cognitive bizarreness in their dreams (mean=0.26 [SD=0.15] and mean=0.34 [SD=0.11]), whereas this is significantly higher—and similar to that of dreams—in the TAT stories of patients with Parkinson’s disease relative to healthy comparison subjects (mean=0.36 [SD=0.17] compared with mean=0.10 [SD=0.10]).
(d) In the Parkinson’s disease population, Pearson regression yielded no significant correlations between the l -dopa equivalent daily dose per kg index and BDI nor between UPDRS-III and BDI in both the dream and waking mentation.
DISCUSSION
The theoretical framework in which our study is set defines cognitive bizarreness as a measurable aspect of dream and waking mentation, and our results show some consistency of this measure across the two states in the experimental sample: cognitive bizarreness was roughly the same in the TAT stories and dream reports of Parkinson’s disease patients and was similar to that found in the dream reports of the comparison group, but was almost completely absent in the TAT stories of the comparison group.
Whereas it is not surprising to find high levels of cognitive bizarreness in the dream narratives of pathological and nonpathological populations, similarly high levels in the TAT-elicited waking fantasy reports of nonpsychotic Parkinson’s disease patients certainly warrant an interpretation. Neither were significant signs of cognitive impairment that could account for several types of abnormalities in the reports of both the dream and waking experience present in this population, nor were any of the patients psychotic at the time of data collection. Cognitive bizarreness in dreams and fantasies did not statistically correlate with motor disability as measured by the UPDRS-III subscale, indicating no significant relationship between the severity of the motor disturbance in these patients and the intensity of their bizarre mentation. Likewise, no significant association was found between the orally administered daily dose of prodopaminergic drugs and bizarreness in both states of the brain-mind. Therefore, bizarreness may be an inherent quality of these patients’ mentation, similar to what has been described in psychotic thought as a form of paralogical or paleological thinking, with errors in syllogistic reasoning derived from the identification of things on the basis of common predicates as opposed to similar subjects.
9 The cholinergic/dopaminergic balance that is thought to play a central role in Parkinson’s disease and schizophrenia as well as in dream sleep may in part account for the similar bizarre cognition we found across these conditions.
15,
24Comparison in terms of cognitive bizarreness in the dream and waking mentation of psychotic and nonpsychotic Parkinson’s disease patients may prove useful in elucidating the brain-mind mechanisms studied here; a further direction in research could also be the longitudinal follow-up in order to evaluate whether or not higher levels of waking bizarreness have some relation to the development of psychotic symptoms in our study population.
The scientific validity of the construct of cognitive bizarreness itself must be addressed as a possible limitation of the study. In general, the concept of bizarreness is poorly defined in psychopathology, and the scoring system used in this study was developed to quantify bizarre elements within dreams, so its use in the quantification of TAT responses must be interpreted cautiously. In our study, this projective test was used as a fixed stimulus for the production of fantasies, possibly implying that specifically fantasies, as opposed to waking cognition in general, have a dreamlike level of bizarreness in Parkinson’s disease patients. In order to compare formal aspects of waking mentation to dreams, fantasy was chosen here as the physiological condition which most closely mimics the fully elaborate, internally generated cognition typically found in dream sleep, and freely collected imaginative narratives have been found to be experimentally less reliable.
25 Another significant limitation of this study is that patients were not differentiated in terms of specific sleep disturbances that are known to be found in 80% to 90% of patients diagnosed with Parkinson’s disease
26 ; these include sleep fragmentation, sleep apnea, restless legs syndrome, REM behavior disorder (RBD), daytime somnolence, and vivid or disturbing dreams.
27 REM behavior disorder is thought to be caused by nondopaminergic pontine lesions in the REM sleep atonia system and has been found to often emerge in the context of neurodegenerative disorders; it occurs in approximately one-third of Parkinson’s disease patients and may precede motor signs by 3 to 13 years.
28 This condition may expose patients with Parkinson’s disease to a higher risk of daytime and nighttime hallucinations,
29 so a more detailed evaluation of cognitive bizarreness within the context of this sleep disorder may prove of interest. Another caveat of the present study is that dream reports were recorded spontaneously by participants upon awakening, with no external monitoring of the type of sleep from which the reports derived. Previous experimental data have, however, identified highly bizarre, vivid, hallucinoid dreams similar to those collected from our participants with REM sleep periods, and REM-like neurobiological modifications may underlie similar subjective experiences during different EEG-defined stages of sleep.
30Finally, the numerical limitation of our sample suggests cautious interpretation of our data, and this preliminary study requires replication.