Case Report
We report on a 41-year-old woman with mild to moderate intellectual disability as well as severe challenging behavior. She has been living in a sheltered home supervised by one of the authors for about 6 years; previously she was living in other institutions. Originating from another part of the country, she has no relatives living nearby, and knowledge about her medical history (e.g., documentation of former hospital treatments) is very limited.
In 2003, she was admitted to our hospital for the first time on a special ward for people with intellectual disability and acute psychiatric disorder in 5-point-fixation due to severe challenging behavior which consisted of crying, spitting, and biting herself and caregivers. She had been placed in a new sheltered home just a few weeks before. In situations without fixation (e.g., during meals or personal hygiene) we saw her beating herself and others and throwing things (up to the size of a TV set) around and on people with no comprehensible reason. During the following years, this “psychopathology” alternated with phases of withdrawal, mutism, sleepiness, and anergia, leaving her with the need to be fed and assisted in almost all activities of daily living.
Because of this, phasic occurrence of the impairment bipolar affective disorder had been discussed; however, classical treatment showed no improvement. Diverse medication over time was applied but no general improvement was achievable; the same could be considered for pedagogical and psychotherapeutical approaches.
Since 2006, six inpatient treatments occurred due to the intolerable aggravation of her symptoms. Living conditions could be improved by moving to a more suitable sheltered home. During the following years, it was possible to reduce fixation down to an average of 2 points. The first author (KH) visits her weekly as a consultant.
In March 2009, the patient was admitted to the hospital due to a slightly longer period of withdrawal with moderately aggravated sleepiness. She developed a progressive loss of consciousness over the next few days which led to referral to the neurological department.
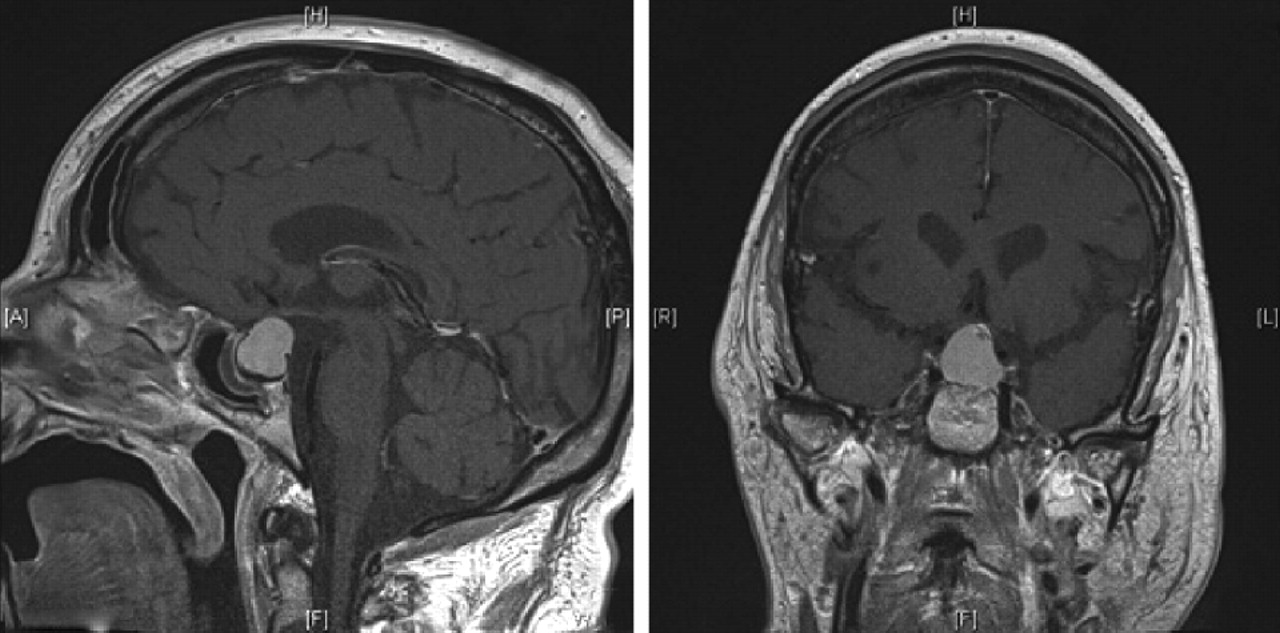
Upon admission, the patient was in a coma with a Glasgow Coma Scale score of 6, showing spontaneous ventilation, intact brain stem reflexes, nondirectional but symmetric pain response, and normal reflexes without Babinski sign. Secondary signs of pituitary gland insufficiency or increased hormone production were lacking. Cranial CT scan showed no signs of ischemia or hemorrhage but a suspected pituitary gland adenoma was confirmed by MR imaging (
Figure 1 ). EEG examination showed continuous, generalized delta activity together with the neuroradiological findings, suggesting coma due to insufficiency of the pituitary gland. Consequently, we started high-dose substitution of hydrocortisone.
Pituitary gland dysfunction could be confirmed by blood tests revealing slightly increased sodium levels (147 mmol/liter) as well as substantially decreased levels of thyroid hormones (thyroid-stimulating hormone: normal; free T 3 : 1.3 ng/liter; free T 4 : 5.7 ng/liter), luteinizing hormone (1.6 U/liter), cortisol (7.8 μg/liter), IGF-1 (<20 μg/liter), and ACTH (<1.0 ng/liter). Under substitution of hydrocortisone and thyroid hormones, the patient regained consciousness within 2 days. The tumor was removed by the neurosurgeon five days after admission to the neurological department. Surprisingly, neuropathological examination revealed craniopharyngioma WHO grade I instead of pituitary gland adenoma. No additional treatment was necessary and neuroradiological control was recommended. One week after intervention the patient was released to her sheltered home, where she very soon displayed the well-known psychopathology again. Medical findings, including cerebral CT scans in 2003, were all inconspicuous.
Conclusion
Psychopathology in people with intellectual disability can be caused by many reasons, even physical illness. Changes in psychopathology may also be a sign of or induced by physical illness. The construct of diagnostic overshadowing made by Reiss et al.
1 and the subsequent modifications by Sovner
2 and Emerson
3 can be transferred to physical illness. Physicians treating people with intellectual disability have to be aware not to miss or to misinterpret such symptoms and to initiate adequate diagnostics and treatment if there is a slight cause for suspicion.
In the case of our patient, missed diagnostics most probably would have resulted in a fatal course of the disease. Hence, in cases of unexpected or unclear death of patients with intellectual disability, an autopsy appears reasonable to broaden that knowledge base.
Due to this fact and to deepen the knowledge concerning this matter, a multicenter study including all German special wards for people with intellectual disability and acute psychiatric disorder is projected; furthermore, everyone interested in this field is invited to take part.