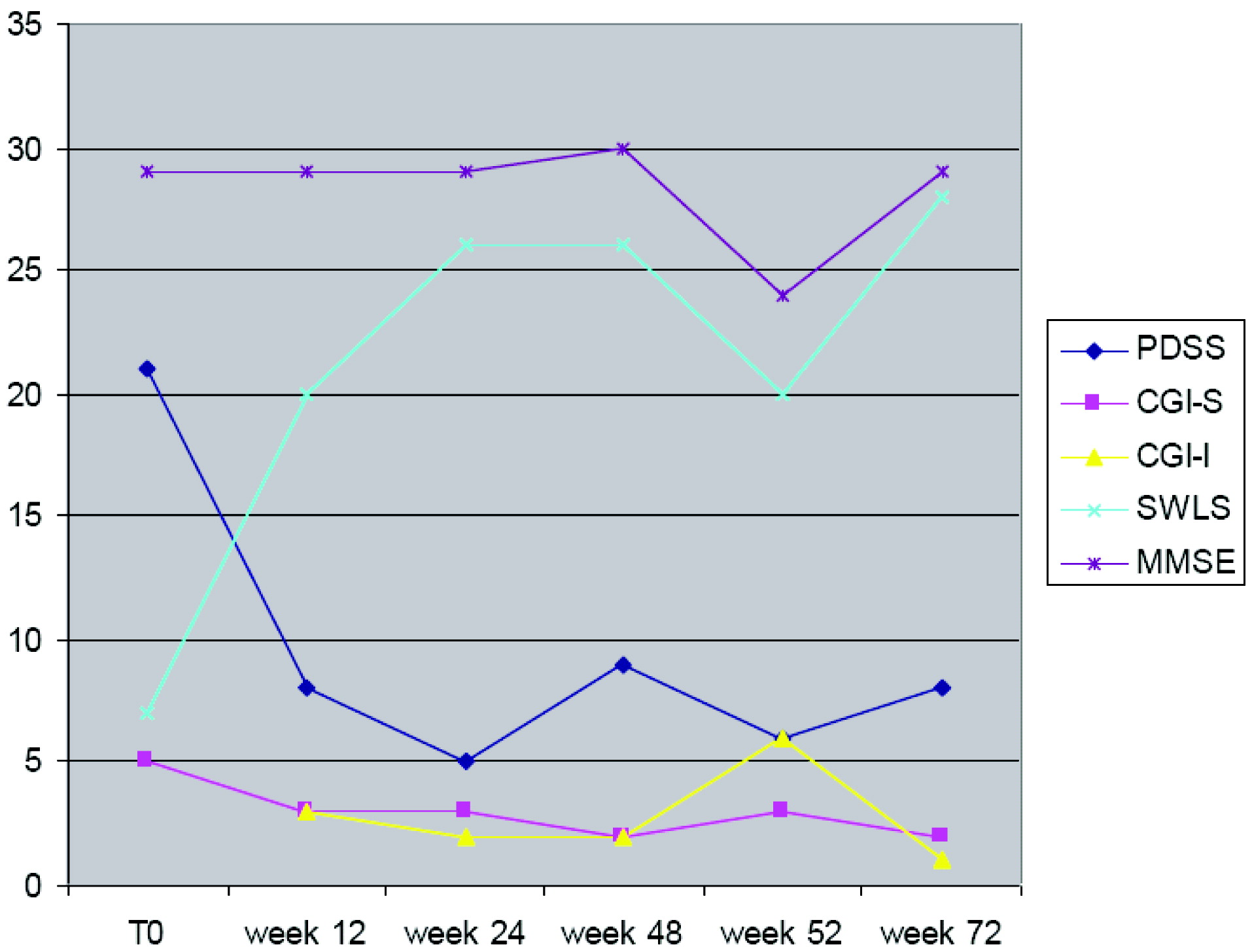
We observed a substantial improvement in panic- and anxiety-related symptoms in a patient with a DSM-IV panic disorder diagnosis, hypertriglyceridemia, and hypercholesterolemia with bupropion at 150 mg daily and the onset of symptomatology characterized by chest pain, severe agitation, increased anxiety, and cognitive impairment at increased dosage (300 mg daily). This case report showed that bupropion was effective not only in reducing or eliminating panic attacks, avoidance behavior, and anticipatory anxiety, but also in improving and normalizing psychosocial functioning and quality of life that represent the most relevant pharmacologic goal in the treatment of panic disorder.
13 Only a few previous studies in the literature investigated the efficacy of bupropion in panic and anxiety disorders. Simon et al.
6 have suggested in 20 outpatients meeting criteria for panic disorder with or without agoraphobia in an 8-week, two-center, open-label, flexible-dose trial, that bupropion SR may be meaningfully effective, resulting in clinically and statistically significant mean reduction of 1 to 2 points in the main outcome measure (CGI Severity score), in both the intent-to-treat and completer samples. Gebhardt et al.
14 most recently have reported that bupropion may be effective and well-tolerated in the case of a patient with Parkinson's disease who also suffered from panic disorder. However, previous evidence reported negative findings (e.g., increased panic and anxiety symptoms) with combined pharmacological strategies of the SSRI fluoxetine and bupropion,
15 and a related lack of efficacy in the treatment of panic disorder with phobias.
16,17 Also, we found that bupropion was effective and well tolerated only at 150 mg daily. When his dosage was increased to 300 mg daily, our patient experienced strong adverse effects; in particular, he was very fearful about the onset of chest pain. Effectively, the presence of cardiovascoular risk factors such as hypertriglyceridemia, hypercholesterolemia, and hyperlipidemia, combined with the possible drug-induced coronary vasospasm, increased the risk of developing acute cardiovascular disease. de Graaf and Diemont
18 have suggested that treatment with bupropion may be associated with chest pain, presumably exerting a direct action on the human myocardium by triggering catecholamine release.
19 According with this evidence, Vidovich et al.
20 recently reported that bupropion presumably exacerbated a recent angina episode through coronary vasospasm in a patient suffering with depression, panic episodes, and recurrent coronary vasospasm, so bupropion treatment required a reduction of dosage in patients with cardiovascular disease. A further consideration must be relative to cognitive impairment, which was clinically observed with bupropion treatment at increased dosages. It was reported that bupropion may suppress tumor-necrosis factor (TNF) synthesis by mediating increased signaling at beta-adrenoreceptors and D1 receptors, resulting in increased cAMP, which inhibits TNF synthesis.
21 TNF is a pleiotropic cytokine deemed crucial in a broad range of biological activities, including inflammation, cell survival, and cell proliferation, but, also, cell death.
22 TNF is also an important mediator of the β-amyloid (Aβ)-induced inflammatory response of the cognitive impairment in Alzheimer's disease,
23 so that TNF production seems to be determinant in synaptic plasticity and memory-formation in the healthy brain. However, the lack of an adequate check of cytokine levels and a direct relationship between increased cytokine levels and cognitive impairment do not allow us to hypothesize that bupropion treatment at higher dosages may be associated with synaptic loss and memory-consolidation disruption. Finally, bupropion may be effective only in some clinical aspects of anxiety disorders; in fact, although the features constituting the DSM-IV diagnostic definition of panic disorder form a coherent syndrome,
24 researchers have also documented only a partial independence of these symptom domains (e.g., panic frequency is not strongly associated with agoraphobic avoidance).
25 So, we believe, reviewing earlier evidence,
26 that bupropion at higher doses could be effective only in reducing symptoms like agoraphobic avoidance and less in reducing panic/anxiety symptomatology itself. We believe that physicians may benefit from this case presentation, which, although limited by the clinical nature of the study, adds relevant evidence of the efficacy of bupropion in panic disorder, also because results were sustained over a long period of follow-up.