To the Editor: A 27-year-old male driver was admitted to our hospital because of aggression. Two months before admission, after an encounter with the police, his symptoms of aggression, physical abuse of his spouse, and suspiciousness had been exacerbated. He also had disturbed social behavior. The night before coming to the hospital, he was watching an action film, and a scene in the film made him so aggressive that his behavior became out of control, and his family brought him to Psychiatric Emergency. He had sleep problems, and he was awake all night. In the week before admission, on one occasion, he took off all his clothes and burned them all, and then spent a large amount of money buying new clothes.
He had a previous history of secondary generalized tonic–clonic epilepsy, which began at 14 years of age and was controlled with sodium valproate, but because of his taking the drug irregularly, he had seizures occasionally. Also, he had been summoned to court for several legal problems. His developmental milestones were normal, and he did not have a history of neonatal jaundice or convulsion. Since adolescence, he had been intrusive in his increased involvement with others, leading to friction with family members and friends. His other abnormal behaviors since adolescence include unaccustomed profanity and tactless jocularity, and impulsive and aggressive behavior. History of substance abuse was negative.
On examination, he had good grooming and eye contact. His psychomotor and speech tone and volume were increased, and he was agitated and distractible. His mood was irritable, but with appropriate affect. He had persecutory delusions, ideas of reference, and intrusive thoughts about involvement with others, as well as flight of idea. No hallucinations were present. The Mini-Mental State Exam score was 26 (of 30). All other neurological examinations, as well as general physical examination, was unremarkable.
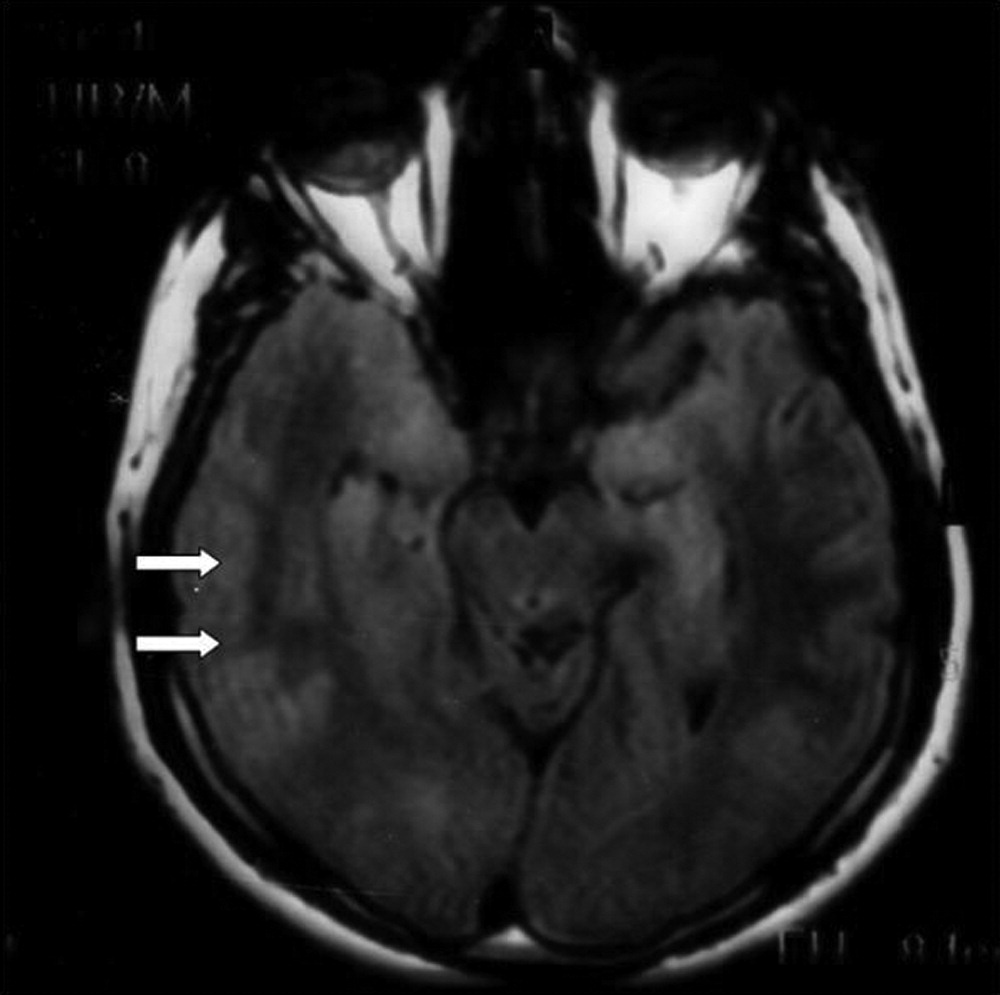
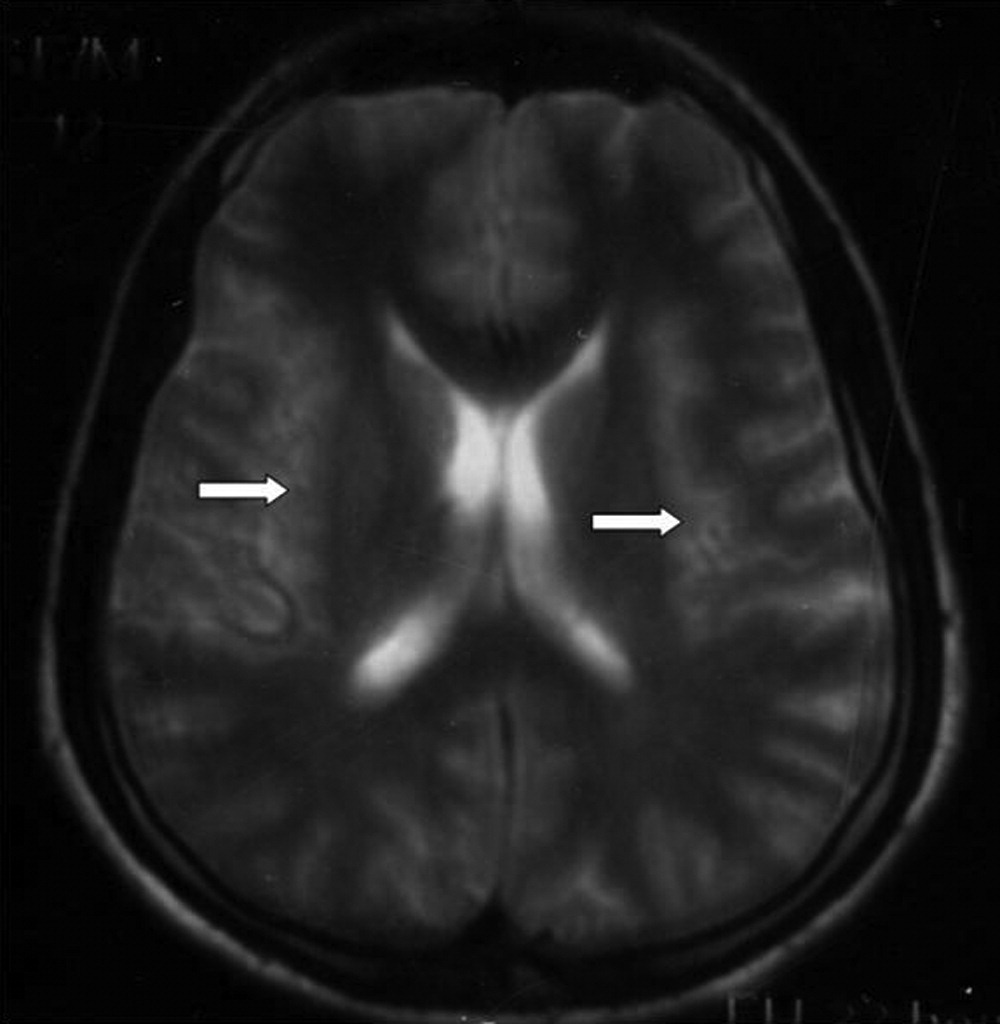
Routine laboratory examinations as well as urinary sample for opium, cannabis, and amphetamines were negative. His EEG did not show any abnormal discharges. In his MR imaging, bilateral increase in cortical diameter of temporal lobes (pachygyria) and fine gray matter foci in white matter of centrum semiovals in both frontal lobes were observed, which was suggestive of migrational anomaly (
Figure 1 and
Figure 2, respectively).
The diagnosis of mania was established because of irritable mood, mood-congruent delusions, distractibility, pressure of speech, psychomotor agitation, and decreased need for sleep, as well as exclusion of other causes such as paranoid schizophrenia and substance abuse/withdrawal.
Sodium valproate (250 mg daily) was initiated and was titrated gradually to 1,250 mg in the 2nd week. The patient responded well to the medication, and this further supported the diagnosis of bipolar mood disorder (BMD). Also, we referred the patient to a psychotherapist for management of his impulsive behavior. The patient was discharged 7 days later.
Neuronal migration disorders including pachygyria and lissencephaly are a group of heterogeneous disorders characterized by mental retardation and epilepsy, and it is often accompanied by other malformations. In the recent years, several genes that regulate neuronal migration have been reported to be malfunctioning or show polymorphism in BMD. For example, DISC1 and Ndel1 are key regulators of neuronal migration and have been shown to be disrupted in BMD.
1 In another study on a single nucleotide polymorphism, rs31745, related to protocadherin alpha gene-enhancer, a remarkable increase in homozygotes for the minor allele at this locus was shown in BMD.
2 Protocadherins are important regulators of neuronal migration. Recent findings provided evidence between some lissencephaly-related genes and both schizophrenia and bipolar disorder and influence on frontal executive function.
3 Also, both epilepsy and BMD can be explained by abnormal kindling, which was shown to be disturbed in neuronal migration disorders.
4,5