Yet little is known about the types of family behaviors that enhance rather than detract from the quality of life of persons with schizophrenia. Lopez and colleagues (
2 ) have begun to identify prosocial family processes, such as the expression of warmth and positive remarks, that support clients on their road to recovery. However, research on adults with schizophrenia has been limited to studying the relationship of these prosocial behaviors to relapse (
3,
4,
5 ). The purpose of this cross-sectional analysis of data drawn from a longitudinal study of families and adults with schizophrenia was to build upon and extend this work by investigating whether these prosocial family processes also are associated with greater life satisfaction among persons with schizophrenia.
In addition, an individual's self-concept is deeply influenced by the attitudes of significant others with whom he or she most intensively interacts (
9 ). Because few persons with schizophrenia marry and have children, their self-concept may be particularly influenced by parental attitudes. Expressed emotion research indicates that persons with schizophrenia are profoundly affected in a negative way when living in environments characterized by high levels of criticism, be they the parental home or nonfamily settings (
10,
11,
12 ). Conversely, the general literature on parenting indicates that the expression of parental warmth and nurturance is associated with a variety of positive psychological adjustments among children (
13 ). Similarly, we hypothesized that expressions of parental warmth and praise and a better-quality relationship between the parent and adult child would be associated with higher levels of life satisfaction among adults with schizophrenia.
In exploring the relationship of these prosocial family processes to the life satisfaction of adults with schizophrenia, we recognize that there is growing evidence for the bidirectional nature of parent-child relationships in general and, more specifically, between expressed emotion among relatives and the functioning and symptom levels among persons with schizophrenia (
10,
14,
15 ). Thus a complementary or alternative hypothesis is that adults with schizophrenia with higher levels of life satisfaction interact in ways that elicit more positive responses from others. In this cross-sectional study, we focused our ordering of variables and discussion on the influence of prosocial family behavior on the life satisfaction of individuals with schizophrenia because researchers have, for the most part, neglected the positive role that families play in the lives of adults with schizophrenia. Also, the temporal sequencing of administering the measures was consistent with this ordering of the variables in our analysis—that is, individuals with schizophrenia completed the life satisfaction scale about three weeks after the prosocial measures were administered to the mother. Given the cross-sectional nature of the study, however, we can demonstrate only an association between prosocial family processes and the life satisfaction of adults with schizophrenia and cannot establish a causal direction.
Methods
The data are from the third wave of a longitudinal survey of 295 aging families of adults with schizophrenia. Families were recruited through community support programs, the local media, and the National Alliance on Mental Illness. Mothers were the primary family respondent and were asked to participate if they met three criteria: the mother was aged 55 years or older, the mother reported that her son or daughter had been diagnosed by a psychiatrist as having schizophrenia or schizoaffective disorder, and the mother provided at least weekly assistance with a major activity of daily living to her son or daughter with mental illness. Mothers completed a two-hour in-home interview and self-administered questionnaire. With the mother's consent, the son or daughter was asked to complete a self-administered questionnaire. Data from the adult child was collected within three weeks, on average, after the mother's interview. Informed consent was obtained for all study participants. The institutional review board of the University of Wisconsin-Madison approved all the procedures for the protection of human subjects.
Participants
This analysis was based on data from the third wave of the study (2003-2004) when the Satisfaction With Life (
16 ) scale was added to the adult child's questionnaire. Of the original 295 mothers, 26 died between the first and third wave of the study. Of the remaining 269 mothers eligible to participate at wave 3, 34 mothers dropped out of the study, typically because of illness or time constraints, and an additional 32 mothers participated at wave 3 but completed an abbreviated interview that did not contain the measures of maternal warmth or praise. The remaining 203 mothers completed the full-length in-home interview and self-administered questionnaire. When the 203 mothers who participated fully were compared with the 66 who did not participate or who participated at a reduced level, no significant differences were found in maternal age and education, the adult child's age or gender, or the mother's baseline (wave 1 of the study) report of the severity of her son or daughter's psychiatric symptoms, as measured by the Symptom Severity Scale (
17 ).
Of the 203 mothers, 143 (70 percent) gave us permission to contact their adult child with schizophrenia. Of the 143 adult children approached, 129 (90 percent) completed and returned the questionnaire. An additional seven adult children were dropped from the analysis because by the third wave of the study, the adult with schizophrenia had reduced contact (monthly or less) with his or her mother. A relationship between prosocial family processes and the life satisfaction of the adult with schizophrenia would not be expected to occur when face-to-face contact is sporadic.
The 122 mother-adult child dyads included in this analysis were compared with the 81 dyads who were lost to attrition for various reasons—that is, the mother refused permission, the adult child refused to participate, or the mother and adult child had infrequent contact. There were no differences between the groups with respect to maternal age, marital status, or education and the adult child's age, gender, work status, number of hospitalizations, psychiatric symptoms (as reported by the mother), and the number of positive remarks made by the mother during the Five-Minute Speech Sample (FMSS). However, mothers who participated in the study had significantly higher levels of maternal warmth compared with mothers who did not participate (mean±SD score of 3.1±1.1 compared with 2.7±1.1; t=2.77, df=200, p<.01). There also was a trend for mothers who participated to report having a higher quality of relationship with the adult child than mothers who did not participate (mean score of 47.3±6.4 compared with 45.2±8.3, respectively; t=1.90, df=141, p=.06). (For scoring information, see below.)
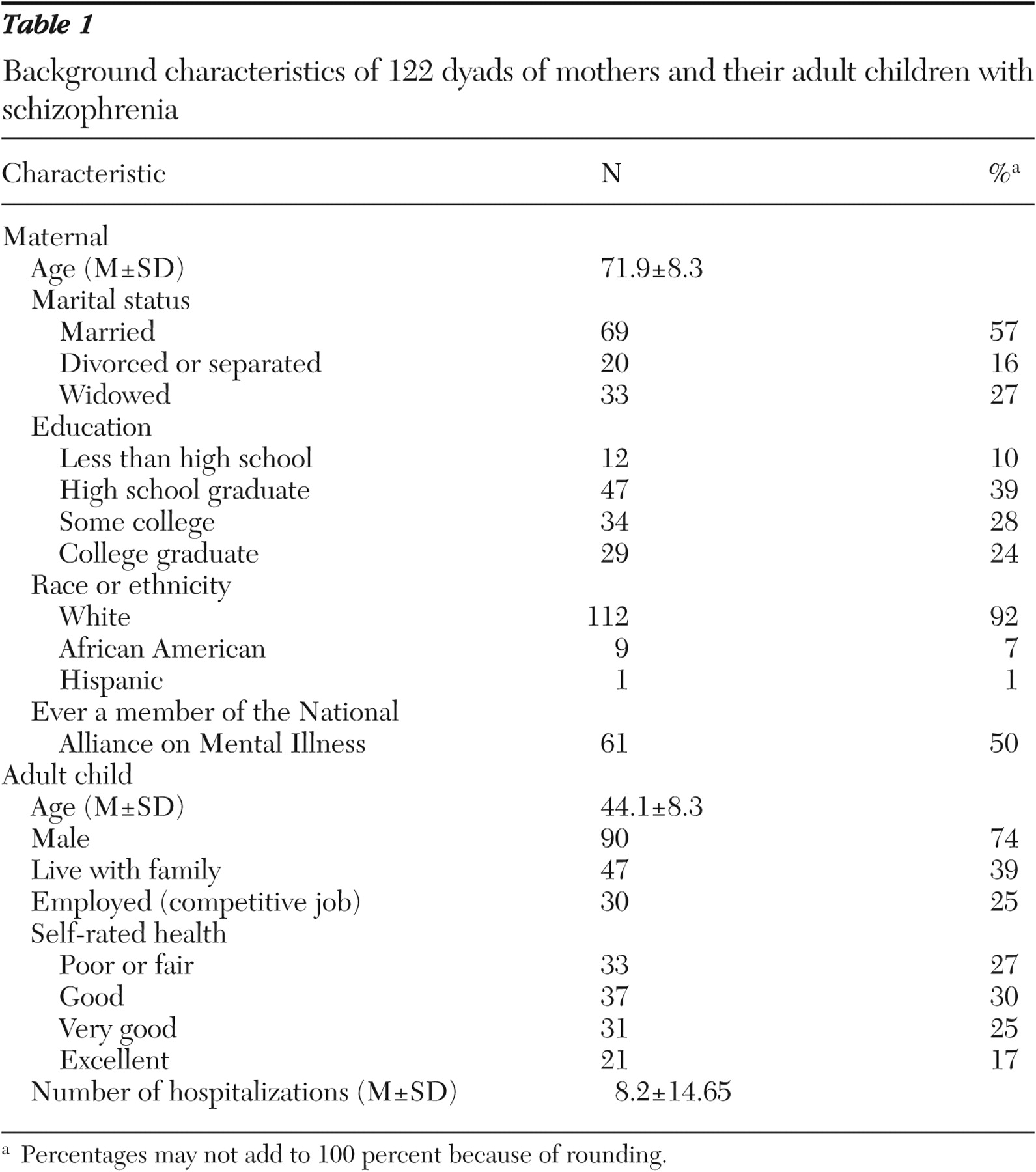
As shown in
Table 1, the 122 mothers had a mean age of 71.9 years, and 57 percent were married. The adults with schizophrenia had a mean age of 44.1 years, and 74 percent were men. Thirty-nine percent lived with their parents, 25 percent were employed in competitive jobs, and only 17 percent rated their health as excellent.
Measures
We investigated three indicators of prosocial family processes: warmth, praise, and quality of the relationship. Maternal warmth and praise were coded from the FMSS, developed as an alternative, brief method for assessing expressed emotion in which the mother is asked to speak uninterrupted for five minutes about her relationship with her son or daughter (
18 ). Ratings of maternal warmth were based on guidelines developed for coding warmth from the Camberwell Family Interview (CFI) (
19 ). The CFI is a one- to two-hour semistructured interview administered to a family member to obtain information about the circumstances in the home in the three months preceding the person's admission for psychiatric care (
20 ). Level of warmth, rated on a 5-point scale from 1, no warmth, to 5, high warmth, is based on the tone of voice, spontaneity of expression of sympathy, concern and empathy, and the expression of interest in the adult child with schizophrenia. The mean rating of warmth in this study (3.1±1.1) was slightly higher than ratings of warmth reported by Lopez and colleagues (
2 ) (2.8±1.4) and King and Dixon (
14 ) (2.9±1.0) in studying families of persons with schizophrenia.
Maternal praise was measured by the number of positive remarks the mother made about her son or daughter during the FMSS. A positive remark is one in which a person's behavior or personality is praised or complimented (
18 ). These remarks are coded on both tone and content; examples include "He is a wonderful person," and "I really admire her." Because few mothers made more than five positive remarks, five or more positive remarks were coded as 5 to correct for skewness in the distribution of the variable. Thus possible scores ranged from 0 to 5. The mothers made an average of 1.6±1.6 positive remarks. The coding of the FMSS was performed by a highly trained rater who had more than two decades of experience coding both the FMSS and the full CFI. In a reliability study, a second experienced rater independently coded 15 FMSS tapes. The intraclass correlation coefficients between the two raters for maternal warmth and positive remarks were .79 and .88, respectively.
Quality of the relationship between the mother and adult child was measured by the Positive Affect Index (PAI), a ten-item self-report measure completed by the mother (
21 ). Five questions address the mother's feelings of positive affect toward her son or daughter (for example, "How much affection do you have toward your son/daughter?"), and five questions represent the mother's perception of positive affect from her son or daughter (for example, "How much affection do you feel that your son/daughter has for you?"). Each question is rated on a 6-point scale ranging from 1, not at all, to 6, extremely. Possible scores range from 10 to 60, with higher scores indicating better quality relationships between the parent and adult child. Construct and discriminant validity of the PAI have been established (
21,
22 ). The scale had a Cronbach's alpha reliability of .88 in this sample.
Mothers also completed the Symptom Severity Scale from the Schizophrenia Outcomes Module: Informant Version (
17 ). The scale consists of 11 symptoms of depression and psychosis rated on a 4-point scale ranging from 1, not at all, to 4, a great deal. Possible scores range from 11 to 44, with higher scores indicating higher levels of symptomatology. The mean level of symptoms was 20.3±7.20, and the scale had an alpha reliability of .89.
The remaining variables were measured from the self-administered questionnaire completed by the adult with schizophrenia. Life satisfaction was measured by the self and present life subscale of the Satisfaction With Life Scale (
16 ). This subscale was selected because it measures general satisfaction with oneself, whereas the other subscales focus on specific domains (that is, living situation, work, and social life). It consists of six items asking individuals to rate their satisfaction with different aspects of their psychological well-being along a 5-point scale ranging from 0, not at all, to 5, a great deal. The self and present life subscale has a possible score range of 0 to 30, with higher scores indicating higher levels of life satisfaction. The score on the self and present life subscale among clients in this study (mean=2.2±.85) is similar to the mean score reported by Test and colleagues (
16 ) of Program for Assertive Community Treatment clients living independently in the community (mean=2.1±.71 and 2.2±.90 at 12 and 24 months, respectively). The reliability and validity of the scale has been established (
16 ) and has been widely used in studying the life satisfaction of persons with schizophrenia (
23,
24,
25 ). The scale had a Cronbach's alpha reliability of .88 in this sample.
Control variables included the following characteristics of the adult with schizophrenia: level of depressive symptoms, level of functioning, number of close friends, age, and gender. Depressive symptoms, which are correlated but independently associated with quality of life (
26 ), were measured by the depression subscale of the Brief Symptom Inventory (BSI) (
27 ). The depression subscale of the BSI is a six-item self-report scale in which respondents are asked how much a problem has distressed them in the past seven days (0, not at all, to 4, extremely). Possible scores range from 0 to 24, with higher scores indicating higher levels of depression. The adults with schizophrenia reported a mean depression score of 1.13±.99, which translates to a T score (that is, a standardized score with a mean of 50 and a standard deviation of 10) of 47 based on the norms for psychiatric outpatients (
27 ). The Cronbach's alpha reliability was .89.
Level of functioning was measured by the Instrumental Activities of Daily Living (IADL) scale (
17 ). The IADL scale consists of 11 items asking the adult with schizophrenia to indicate the degree to which he or she performed 11 tasks of daily living (for example, personal hygiene, food, transportation, and money management) during the past month on a 5-point scale ranging from 0, almost never, to 4, nearly always. The IADL scale has a possible range of 0 to 44, with higher scores representing higher levels of independent functioning. The scale had a Cronbach's alpha reliability of .84. The mean score on the IADL scale was 3.0±.70. The number of friends was coded by a single item asking the adult to indicate how many close friends he or she had (0, none, to 5, five or more). Approximately 40 percent of the adults reported having three or more friends. Additional control variables included the individual's gender (1, female, or 0, male), and age (in years).
Data analysis
Hierarchical ordinary least-squares multiple regression analysis was used to examine the relationship of prosocial family processes to the life satisfaction of the adult with schizophrenia. The control variables were entered on the first step, and the prosocial family processes were entered on the second step. Separate regression analyses were conducted for each of the three prosocial family indicators (that is, warmth, praise, and relationship quality) and referred to as model 1, model 2, and model 3, respectively. A power analysis was conducted on the basis of the following assumptions: a sample size of 122, an alpha of .05, and the five control variables, which explained 35 percent of the variance. The study had a power of .69 to detect a 3 percent increment in variance explained in life satisfaction by any indicator of prosocial processes (
28 ).
Problems of missing data were minimal, as callbacks to respondents were made to obtain missing information. For individual items missing on scale scores, a mean score was imputed if 75 percent of the items for the scale had been completed. In no case were more than 25 percent of the items for a scale missing.
Discussion
Lopez and colleagues (
2 ) were among the first to search for family prosocial behaviors that promoted the well-being of persons with mental illness. In the tradition of research on expressed emotion, they focused on the role of these prosocial processes in reducing relapse among persons with schizophrenia. Our findings point to the promise of extending this work on the effects of these prosocial processes to recovery-oriented outcomes, such as the life satisfaction of individuals with serious mental illness.
Adults with schizophrenia reported a higher quality of life when their mothers displayed higher levels of warmth and their mothers described them in a more affirming and validating way. When parents provide a nurturing environment and offer praise, the child is encouraged to view himself or herself more positively (
9 ). The importance of parental warmth and positive parental appraisals may be even more significant for adults with severe mental illness, who often confront acts of stigma or discrimination on a daily basis. Our findings as well as past research on the contributions of persons with mental illness to their family (
29 ) suggest that when family members are able to look beyond their relative's deficits and recognize and affirm the relative's strengths, not only is their own burden reduced (
30 ) but they also may contribute to the overall quality of life of their loved one. However, many families struggle with their relative's mental illness and may have difficulty stepping back to reflect on their relative's positive attributes without the encouragement of mental health clinicians. Falloon and colleagues (
31 ) have developed a behavioral family therapy intervention that incorporates therapeutic strategies for strengthening prosocial family processes. The intervention involves individual and family sessions, in which information about mental illness is shared, and communication and problem solving skills are taught in an effort to help family members support and affirm the positive qualities in one another.
The parenting literature suggests that a supportive relationship between the parent and adult child has a modest but significant effect on the psychological well-being of adult children (
32 ), which is similar to the pattern found here. Mental health researchers have devoted considerable effort toward identifying factors that promote friendships because of the importance of these relationships to the quality of life of persons with schizophrenia (
33 ). However, little is known about the factors that promote close relationships between adults with schizophrenia and their parents. Identifying these factors is a necessary first step toward the goal of developing interventions to strengthen these family bonds. The current practice of including clients in multiple-family groups might be encouraged in all family psychoeducation programs, as it provides an opportunity for adults with mental illness and their family members to work together to form a more supportive and understanding relationship (
34 ).
We conducted an exploratory qualitative post hoc analysis of the FMSS transcripts in an effort to identify specific prosocial maternal behaviors associated with high levels of life satisfaction among individuals with schizophrenia. We compared 20 mother-adult child dyads: ten dyads in which the mother had high scores on the indicators of prosocial family processes and the adult with schizophrenia reported high levels of life satisfaction and ten dyads who had low scores on these measures. This analysis revealed three types of prosocial behaviors associated with high levels of client life satisfaction. First, mothers in the high prosocial group initiated activities that supported their son or daughter's sense of being a competent adult. These activities were ones that their son or daughter enjoyed and could do well, such as gardening, playing board games, or engaging in a sports activity. Second, mothers in the high prosocial group were more likely to acknowledge and affirm small steps that their son or daughter made toward recovery, even when the adult fell short of the goal. For example, one mother spoke of the courage and determination her son showed in making attempts to return to school after experiencing several setbacks. Third, mothers in the high prosocial group were less reactive to displays of negative symptoms (for example, lack of conversation and detached behavior). Whereas mothers in the low prosocial group expressed their frustration and desire to change negative symptoms, mothers in the high prosocial group were more accepting of these symptoms. For example, a mother in the high prosocial group responded sympathetically when her son was feeling stressed by the stimulation at a large family dinner and wanted to return to his room. In contrast, a mother in the low prosocial group reacted to a similar situation by becoming quite upset with her son for wanting to retreat to his room.
On a related note, mothers who displayed high levels of prosocial behavior seemed able to separate the person from the illness. In the words of one mother, "He's a very gentle person, but the illness, when it manifests itself, it makes him into somebody completely different … angry, hostile, somebody who is ruled by voices." Mothers in the low prosocial group had great difficulty separating the symptoms from the person. They were more likely to perceive symptoms as willful and to respond with criticism and anger. This post hoc analysis speaks to the continued need for mental health professionals to educate families about the symptoms of schizophrenia and to teach families more adaptive strategies of coping with behavioral manifestations of the illness. It also reminds us that many families have a great deal of "practice wisdom" and have much to teach mental health providers about how to most effectively intervene with their adult child with schizophrenia.
There are several limitations to this study that should be noted. First, our sample was drawn from clients with schizophrenia or schizoaffective disorder who were living in one Midwestern state and had regular contact with their mothers. Our sample is also limited by its ethnic and racial homogeneity; less than 10 percent of the sample was from an ethnic minority cultural group, which potentially reduced the generalizability of the findings. Second, our attrition analysis suggests that the sample of 122 mother-adult child dyads has a small bias toward the mother's expressing higher levels of warmth and having a better quality of relationship with her adult child. Mothers with these characteristics may possess other traits, such as a high level of motivation or commitment toward helping their adult child, which may influence the strength of the relationship between these prosocial processes and the quality of life of the adult with schizophrenia.
Third, the measurement of prosocial family factors was based on data collected from mothers because of their role as the primary caregiver when this study began. Although sampling the primary caregiver is a common practice in studying families of persons with serious mental illness, future research needs to determine if these prosocial processes have similar effects when enacted by other family members.
Fourth, and most important, given the cross-sectional and correlational nature of the data, causality cannot be established. In this study we focused on the relationship of maternal prosocial processes to the life satisfaction of adults with schizophrenia, in part, because the life satisfaction data were collected from the adult with schizophrenia after the mother's interview, during which the prosocial measures were administered. However, an alternative hypothesis is that clients with higher levels of life satisfaction may interact in ways that evoke more positive responses from their parents. Clearly, the nature and persistence of the client's symptoms and behaviors affect the parent's response to the child, as demonstrated by King and Dixon (
14 ), who found that maternal criticism was in response to disturbed behavior of the individual with schizophrenia. Goldstein and colleagues (
10,
15 ) conducted a series of studies showing the complex mutually influencing interplay between the clinical functioning of the adult with schizophrenia and the family's level of expressed emotion. Longitudinal studies are needed to examine the bidirectional relationships between these prosocial family processes and the quality of life of individuals with schizophrenia.
In addition, as suggested by our qualitative analysis, the display of low levels of warmth is often a very understandable family response given the nature of the behavior of the individual with schizophrenia and the family's limited knowledge about the negative symptoms of schizophrenia. We hope that rather than blaming families who are less warm or positive in their interactions, professionals can use their experiences to understand and empathize with these family reactions and help educate the family with the aim of promoting more positive relationships.
Counterbalancing these limitations are several unique strengths and features of this study. The sample captures a diverse group of individuals with respect to age, gender, symptoms, functional status, and physical health. The mother's data were collected three weeks, on average, before the data collection from the son or daughter with schizophrenia, giving us more confidence in the temporal ordering of the relationship between prosocial family processes and client satisfaction. Third, we included three indicators of prosocial processes. The convergence of the findings across the three indicators increases our confidence that the results are robust.