Substance use disorders contribute to substantial problems among persons with severe mental illness (
1,
2,
3,
4 ). Prevalence of alcohol and drug problems is increased among persons with major mental illnesses (
5,
6,
7,
8 ). There are even more people with major mental illnesses who have problems related to substance use but do not meet the criteria for abuse or dependence (
4,
9,
10 ). Alcohol negatively affects persons with serious mental illness more profoundly at a lower quantity and frequency of use (
9,
10 ), compared with the effect reported for the general population (
11 ).
Coexisting substance use disorders are associated with medication noncompliance, more severe depressive and psychotic symptoms, poorer psychosocial functioning, and poorer treatment outcome among clients with serious mental illness (
2,
6 ). Patients who are intoxicated or abusing substances present to emergency settings with higher psychiatric acuity, require higher levels of behavioral management, and spend more time in the psychiatric emergency service than do nonintoxicated, non-substance-abusing individuals. These individuals raise unique risk management issues because of the potential danger to themselves or others while intoxicated.
The purpose of this study was to determine the prevalence of at-risk drinking among patients seen in a large psychiatric emergency service and to examine the characteristics and functioning of at-risk drinkers with schizophrenia or bipolar disorder (serious and persistent mental illnesses) and compare them with those of at-risk drinkers who had depression or anxiety disorders. This analysis is part of a larger study designed to determine the effectiveness of brief alcohol interventions and case management with patients who have at-risk drinking.
Methods
All eligible adult psychiatric emergency service patients aged 18 years and older with major mental illnesses were asked to complete the informed consent form, which was approved by the University of Michigan Institutional Review Board. Patients who were too medically ill, intoxicated, or incarcerated or who had acute psychosis, were being seen for an overdose, had suicide attempts, or had legal guardians were excluded from the study. A total of 460 psychiatric emergency service patients were approached between 2001 and 2005; 70 (20 percent) refused to participate. A total of 390 patients completed questionnaires. An additional 214 patients were not approached because they did not meet inclusion criteria.
The screening questionnaire included health behavior questions adapted from the Health Screening Survey (
12 ), including quantity or frequency items for alcohol use, dieting, tobacco, and exercise in the previous three months; perceptions of a past or current alcohol problem; and seven past-year alcohol consequence items from the Alcohol Use Disorders Identification Test (AUDIT) (
10 ). The consequence questions were analyzed individually and then summed for comparative analysis. The Brief Carroll Depression Scale measured depression levels (
13 ). Individual items were summed; possible scores range from 0 to 12, with higher scores indicating worse functioning. Individuals were considered at risk for alcohol problems on the basis of the following criteria: drank heavily, according to National Institute on Alcohol Abuse and Alcoholism (NIAAA) guidelines, which is defined as 15 or more drinks per week for men, eight or more drinks per week for women; participation in binge drinking (four or more drinks on two or more occasions in the past month); perception of a current problem with alcohol; or reports of two or more alcohol-related consequences in the past year, as measured by the AUDIT (
14 ).
Analyses compared at-risk drinkers with serious mental illnesses (schizophrenia and bipolar disorder) who received their mental health care through a publicly funded community mental health center with at-risk drinkers who had depression or anxiety and generally received care through private insurance sources. Univariate statistics were calculated for all variables. Bivariate relationships were examined by using various measures of association contingent on the description of the data distribution. Chi square tests and t tests were used to determine any differences between the group with schizophrenia or bipolar disorder and the group with depression or anxiety, depending on the categorical or continuous nature of the variables of interest. Analyses were performed by using SAS version 8.02.
Results
Of the 390 patients who were eligible and completed the screening questionnaire, 148 (38 percent) had serious mental illnesses (schizophrenia or bipolar disorder) and were currently receiving services from a community mental health center. A total of 242 patients (62 percent) presented with other mental health diagnoses (depression or anxiety).
There were no statistically significant differences between the groups on gender and race variables. However, patients with depression or anxiety had significantly more education than those with schizophrenia or bipolar disorder (χ 2 =22.46, df=2, p<.001). In the group with schizophrenia or bipolar disorder, 63 (43 percent) were male, 108 (73 percent) were Caucasian, 25 (17 percent) were African American, and 12 (8 percent) were from another racial or ethnic group. Thirty-three patients (23 percent) had less than a high school education, 34 (24 percent) had completed high school, and 76 (approximately 53 percent) had a more than a high school education. (Percentages reflect five cases in the group with schizophrenia or bipolar disorder with missing educational data.)
In the group with depression or anxiety, 99 (41 percent) were male, 192 (79 percent) were Caucasian, 26 (11 percent) were African American, and 23 (10 percent) were from another racial or ethnic group. Twenty-three (10 percent) had less than a high school education, 35 (15 percent) had completed high school, and 183 (76 percent) had more than a high school education. (Percentages reflect one case in the depression or anxiety group with missing educational data.)
Within- and between-group analyses were conducted to determine any differences between groups regarding exercise, weight control attempts, smoking, and alcohol use. There were no significant differences between the groups in weight control attempts and exercise. Patients with schizophrenia or bipolar disorder were significantly more likely to be smokers than those with depression or anxiety (93 patients, or 63 percent, compared with 109 patients, or 45 percent; χ 2 =11.65, df=1, p<.001). Additionally, a majority of patients with schizophrenia or bipolar disorder smoked, regardless of whether or not they drank at risk levels.
Thirty-four persons with schizophrenia or bipolar disorder (23 percent) and 53 with depression or anxiety (22 percent) drank heavily, according to NIAAA guidelines (15 or more drinks per week for men and eight or more drinks per week for women), engaged in binge drinking (four or more drinks on two or more occasions in the past month), reported a perception of a current problem with alcohol, or reported two or more alcohol-related consequences; no significant difference was found between groups. Among the at-risk drinkers, the group with schizophrenia or bipolar disorder drank an average of 23.7±34.1 drinks per week; the group with depression or anxiety drank 24.3±27.8 drinks per week. There was a significant difference between the two groups in use of any alcohol (62 persons with schizophrenia or bipolar disorder, or 42 percent, compared with 140 persons with depression or anxiety, or 58 percent; χ 2 =9.37, df=1, p=.002).
In the group with schizophrenia or bipolar disorder, 31 (91 percent) of the at-risk drinkers reported a past problem with alcohol, and 20 (59 percent) reported a current problem. In contrast, in the group with depression or anxiety, 34 (64 percent) of the at-risk drinkers reported a past problem, and 34 (64 percent) reported a current problem.
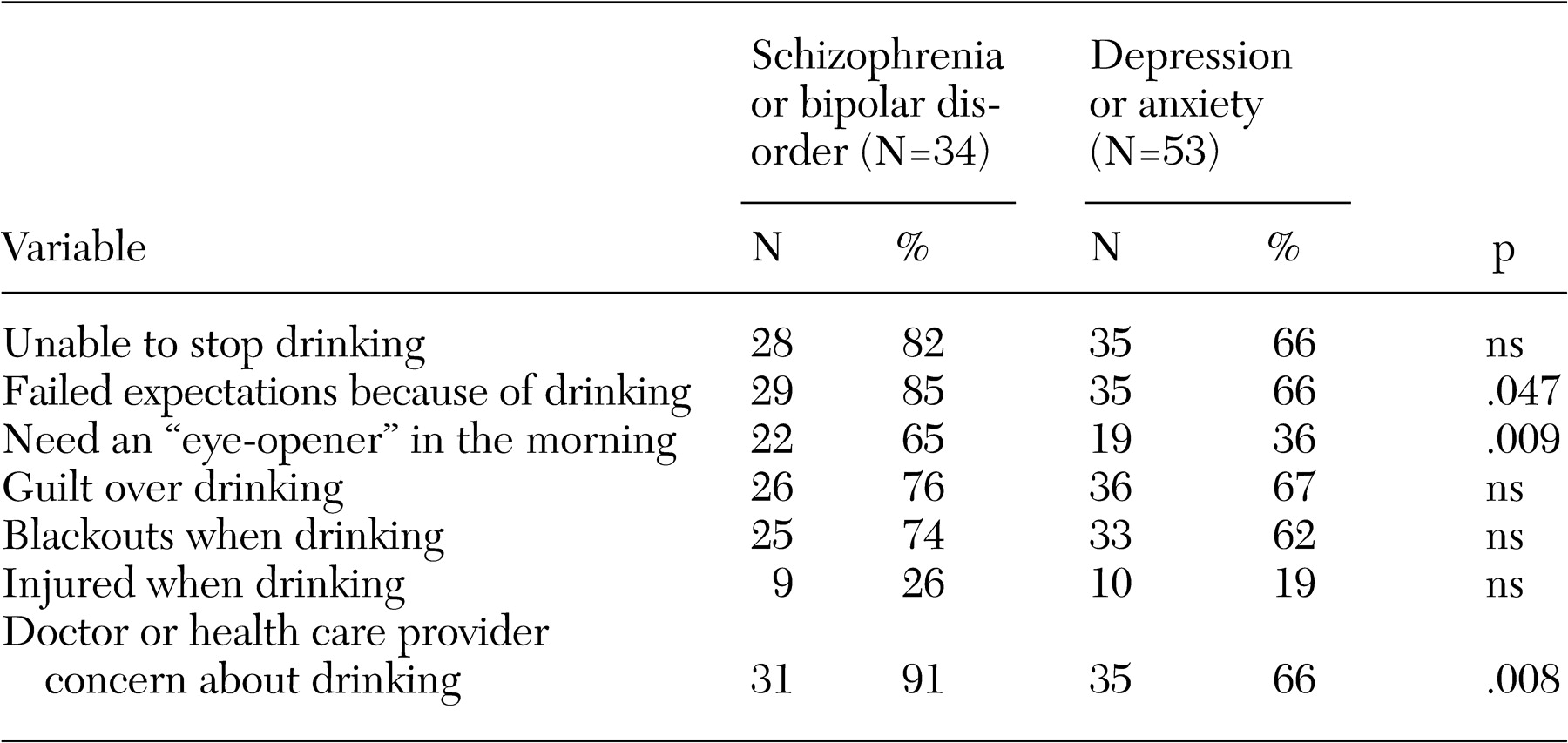
As shown in
Table 1, at-risk drinkers in both groups reported several alcohol consequences. There was a significant difference between groups in the mean number of consequences, with the group with schizophrenia or bipolar disorder experiencing more consequences (schizophrenia or bipolar disorder, mean±SD of 5.00±1.50 consequences; depression or anxiety, mean of 3.83±1.87). Patients with schizophrenia or bipolar disorder were significantly more likely to endorse three specific consequences: failing to meet expectations, needing an "eye-opener" to get going in the morning, and having a health care provider concerned about their drinking. The item endorsed most by both groups was "unable to stop drinking once I start." The item least reported was an "injury resulting from drinking."
Depressive symptoms during the few days before the visit were examined. Both groups scored similarly on the depression scale. With a potential score of 12, at-risk drinkers in the group with schizophrenia or bipolar disorder had a mean score of 9.09±2.35. The group with depression or anxiety had a mean score of 8.46±2.86. There were no statistically significant differences in depression rates between groups. Both groups had a relatively high level of depression (standard scoring, four or more positive items indicates major depression).
Discussion
This study underlines the need for routine alcohol screening in psychiatric emergency services, even when the presenting problems do not appear to be alcohol related. The findings confirm the relatively high rates of current at-risk drinking that have been found in other studies (
6,
9 ) and highlight the presence of alcohol problems among psychiatric emergency service patients, regardless of psychiatric diagnosis. Previous research indicated that substance use rates were higher for patients with schizophrenia and personality disorders but that rates were relatively much lower for patients with affective disorders, adjustment disorders, and other diagnoses (
11 ). Additionally, because of the range of consumption levels for the at-risk groups, a number of those who screen positive for at-risk drinking may fit into abuse or dependence categories.
The types of consequences resulting from at-risk drinking were similarly endorsed by patients with schizophrenia or bipolar disorder and those with depression or anxiety. However, patients with schizophrenia or bipolar disorder had more consequences. In both groups, injury was the least reported negative consequence from drinking. Every other negative consequence was reported by a majority of patients in both groups. Feeling unable to stop drinking was narrowly the most reported consequence, followed by doctor or health care provider concern about drinking. The latter item indicates that many patients with at-risk drinking or abuse or dependence have had a discussion with a professional about their alcohol use. A visit to an emergency department has often been considered a "teachable moment" when a crisis can provide the impetus for the individual to make changes in health behaviors, particularly alcohol use. The psychiatric emergency service may be an ideal setting to target alcohol problems with motivational brief interventions and follow-up case management that will ensure access to substance use care.
Patients from both groups had high rates of depression, endorsing approximately nine of the 12 criteria for depression. Depression is an issue for clinicians to address in this setting when dealing with any patient, whether or not that patient is specifically given a diagnosis of major depression.
Patients with schizophrenia or bipolar disorder were significantly more likely to be smokers than those with depression or anxiety. A majority of patients with schizophrenia or bipolar disorder smoked.
In sum, this study demonstrates the importance of assessing alcohol use and depression symptoms among all patients who present to psychiatric emergency services. Most of the patients who took part in this study were not being seen for their alcohol use, but rather for symptoms of psychosis, depression, anxiety, panic attacks, family problems, or other concerns. Furthermore, these findings highlight the opportunity to address substance use and depression in health care settings and the importance of clinicians' receiving the training and gaining the expertise to provide brief interventions and linkage to treatment when appropriate.
The limitations of the study include the sample size of at-risk drinkers with serious and persistent mental illnesses. The exclusion criteria in the study (for example, acute psychosis, suicidality, or incarceration) made it less likely that patients with schizophrenia or bipolar disorder would be included in the screening sample. It is possible that a high percentage of individuals in the excluded group may have been more likely to have problems related to alcohol, but they could not give informed consent and, therefore, could not be included in the study. Further studies will be needed to address the issues inherent in using these exclusion criteria. Additionally, psychiatric diagnoses were made by clinicians as part of regular practice and were not based on structured research diagnostic instruments and were, therefore, subject to clinical impression rather than standardized instrumentation.
Conclusions
The results of this study confirm previous findings regarding the prevalence and characteristics of the psychiatric population with comorbid alcohol problems (
4,
6,
12 ). Identifying and addressing at-risk substance use in psychiatric emergency settings for patients with major mental illnesses and comorbid alcohol problems is an important step in addressing a serious issue affecting the physical and mental health of these patients at a time when they may be most open to making changes in their health behaviors.
Acknowledgment
The authors thank the Flinn Family Foundation for its support of this research.