Ascertainment procedures
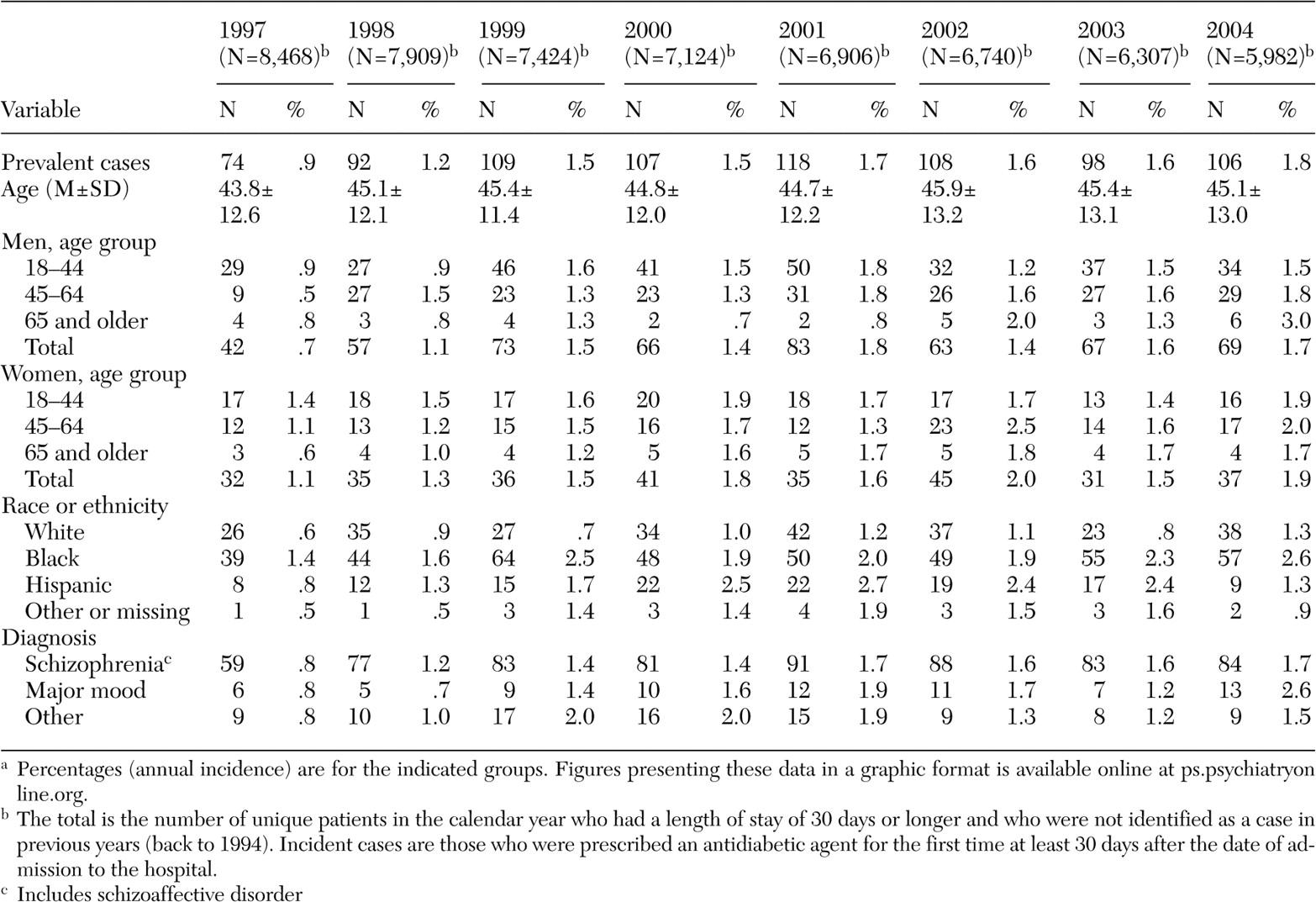
Patients were included in the study if they were inpatients at any time during the period January 1, 1997, through December 31, 2004. Cases were defined as those who had received prescriptions of antidiabetic medication as documented in the IRDB (insulin, glyburide, glipizide, glimepiride, tolbutamide, chlorpropamide, tolazamide, repaglinide, metformin, troglitazone, acetohexamide, acarbose, miglitol, rosiglitazone maleate, pioglitazone hydrochloride, and nateglinide) or those who had a recorded diagnosis of diabetes mellitus ( ICD-9 code 250.xx) in the IRDB. Incident cases were defined as those with a new prescription for an antidiabetic medication; that is, we excluded patients from being considered as an incident case if an antidiabetic medication had been prescribed at any time since January 1, 1994 (the earliest date for which such data were available), as documented in the IRDB. Patients were also excluded from the calculation of incident cases if they ever had a recorded diagnosis of diabetes mellitus.
To reduce the possibility that a prescription of an antidiabetic medication was a renewal of a medication received before hospitalization, for incident cases patients were required to have at least a 30-day period of hospitalization before the start of the prescription of the antidiabetic medication. Patients who received a new diagnosis of diabetes mellitus in the absence of a new prescription of an antidiabetic medication were not counted as a new incident case, because the coding of a diagnosis of diabetes may have occurred immediately after admission in response to the medical history obtained at that time and thus may not have represented a true incident case.
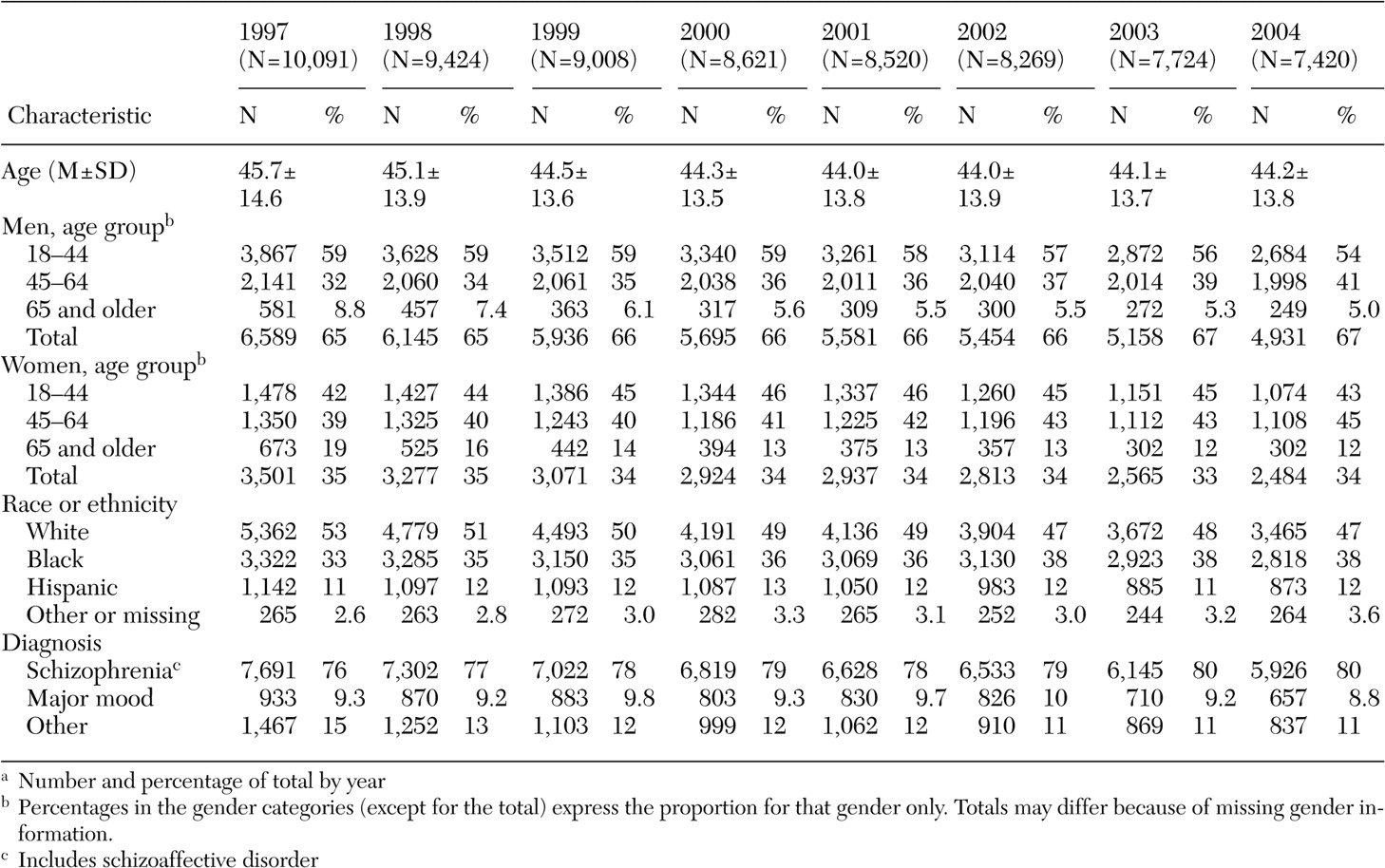
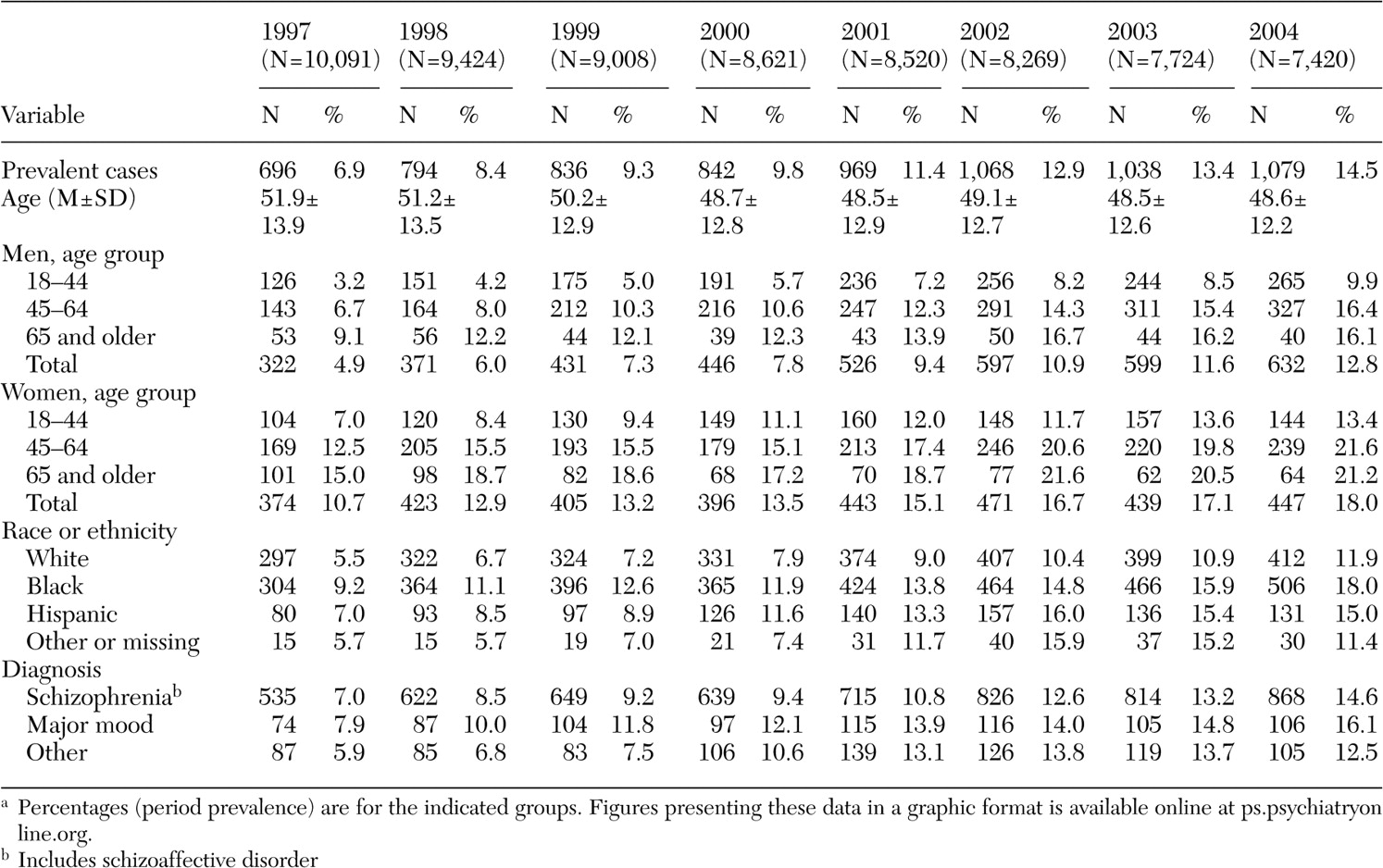
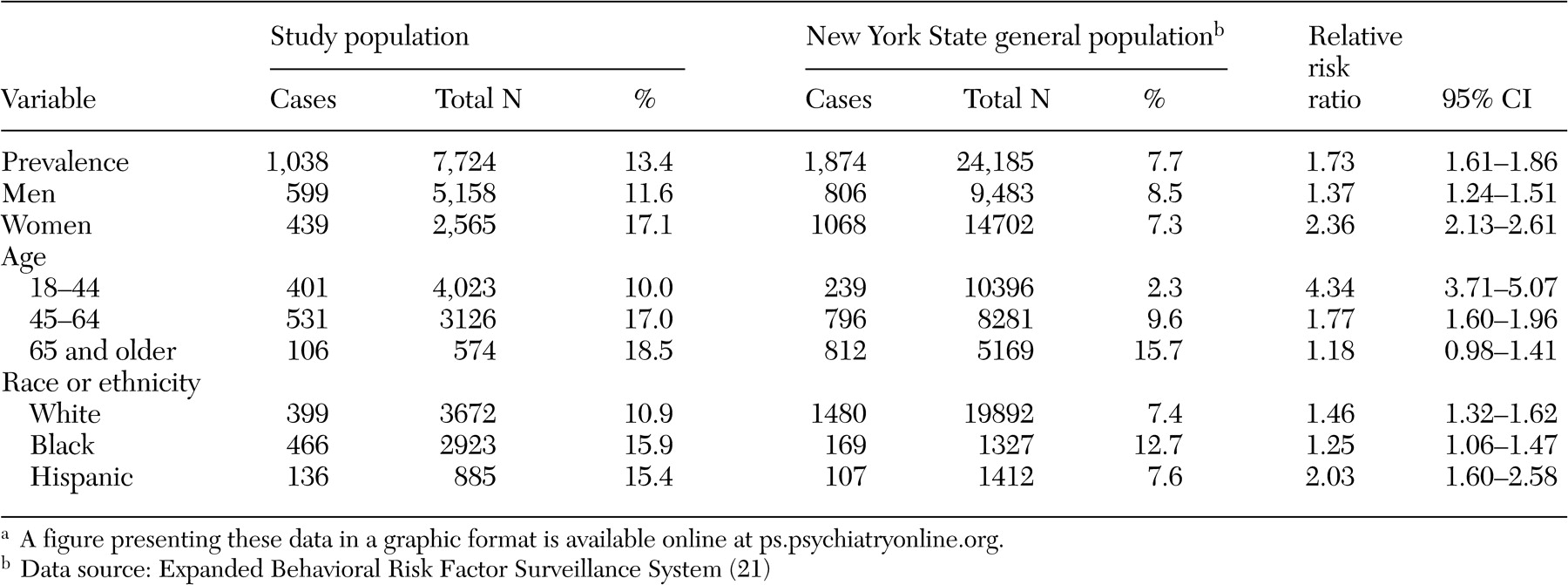
Because the risk of developing diabetes may be related to demographic and diagnostic variables, prevalence and incidence were categorized by gender, race or ethnicity (white, black, Hispanic, and other), and age group (18 to 44, 45 to 64, and 65 years and older). Three diagnostic categories were used: schizophrenia or schizoaffective disorder and other nonmood nonorganic psychotic disorders ( DSM-IV-TR code 295.x, 297.1, 297.3, 298.8, or 298.9), major mood disorders ( DSM-IV-TR code 296.x), and other diagnoses.
Relative risk ratios (RR) for incidence and prevalence were calculated from 2×2 tables. When comparing rates from the year 2004 to those of 1997, we also stratified by gender, age, race or ethnicity, and diagnosis (
19 ). When comparing rates between the subgroups (men versus women, nonwhite race or ethnicity versus white, age 45 years or older versus younger than 45 years, diagnosis of schizophrenia or schizoaffective disorder versus mood disorders or others), we stratified by calendar year.
We compared our prevalence rates with those observed in the population at large in New York State, as estimated by the Behavioral Risk Factor Surveillance System study, which measured, by telephone survey, self-reported diabetes among noninstitutionalized adults aged 18 years or older (
3,
20,
21 ).
Because the likelihood of a person's being diagnosed or treated for diabetes is influenced by the rate at which plasma glucose tests are ordered, surveillance for diabetes mellitus was measured by calculating the frequency of plasma glucose testing performed during the relevant calendar year. These data were obtained from the administrative records maintained by the central laboratory that processes the bulk of these tests for the hospitals operated by the New York State Office of Mental Health. The records indicate if a test was done and its value, but they do not indicate if the sample was taken when the patient was fasting or not. A minority of patients were hospitalized at more remote facilities not served by the central laboratory. Laboratory data were available for nine facilities in 1997 and 1998 and for ten facilities in 1999 through 2002. To avoid counting laboratory tests done for patients with identified diabetes, patients who were identified as a case were excluded. We examined counts of plasma glucose tests per 100 patient-days. To estimate the number of potential cases of diabetes not captured by a recording of a diagnosis of diabetes or the prescription of an antidiabetic medication, we counted the number of unique patients in this group of patients not identified as having diabetes but who nevertheless had plasma glucose levels of 200 mg/dL or greater.