Police officers are often first-line responders to emergency calls involving individuals with mental illnesses (
1,
2,
3,
4,
5 ). To improve officers' responses, the crisis intervention team (CIT) training program was developed in 1988 by the Memphis Police Department in partnership with the Memphis chapter of the National Alliance for the Mentally Ill, the University of Memphis, and the University of Tennessee (
6 ). This innovative program equips police officers with knowledge and skills to enhance their responses to individuals with mental illnesses (
6,
7,
8,
9 ).
In this model, self-selected police officers typically participate in 40 hours of educational training provided by local mental health professionals, family advocates, and mental health consumer groups (
9,
10 ). Upon completion of the training, officers receive certification as specialized first-line responders for calls involving people in crisis (
4,
11 ). Along with officer training, the CIT program supports partnerships between psychiatric emergency departments and police departments, increasing the likelihood that people in psychiatric crisis are taken to medical facilities rather than jails (
8,
10 ).
The CIT program has produced favorable results by reducing unnecessary arrests and use of force, while increasing referral rates to emergency health care (
6,
9,
11 ). Deescalation training and education about mental illnesses enhances police officers' responses to people in crisis, which reduces the need for more costly responses and incarceration (
9 ). Compared with non-CIT officers from the same police department, CIT officers are significantly more likely to feel well prepared in handling crises involving people with mental illnesses (
7 ). However, there has been virtually no empirical research on whether CIT training influences police officers' knowledge, attitudes, and stigma regarding mental illnesses.
The objective of this study was to use a pretest, posttest study design to determine changes in knowledge, attitudes, and social distance (especially regarding schizophrenia) among police officers completing CIT training. It was hypothesized that after the training, officers would report improved attitudes regarding aggressiveness and violence among individuals with schizophrenia, become more supportive of local treatment programs, have enhanced knowledge about schizophrenia, and report lower levels of social distance.
Methods
Data were gathered during nine CIT trainings conducted in the metropolitan Atlanta area between December 2004 and July 2005. Each training class included approximately 18 to 20 officers from local jurisdictions. Although only one hour of the training specifically focused on schizophrenia, many of the other lectures, presentations, and deescalation experiences dealt with schizophrenia as well. Complete pre- and posttest data were available for 159 officers.
The pretest survey included sociodemographic variables and six questions to determine level of familiarity with and exposure to mental illnesses. Aside from these initial questions, all other items were included in both the pre- and posttest. To assess recognition of mental illnesses among people with whom they interact, officers were asked, "As a police officer, have you ever arrested someone with an obvious mental illness?" and "As a police officer, how many people with an obvious mental illness do you deal with during an average month?"
Several items were adapted from the Edmonton Health Attitude Study (
12 ). Two questions assessed attitudes regarding aggressiveness and violence among individuals with schizophrenia, compared with those without the disorder. These items were rated by using a 5-point Likert scale, ranging from 0, "much less aggressive/violent," to 4, "much more aggressive/violent," with a score of 2 indicating "about the same as the average person." Four questions measured level of support for four hypothetical programs "located about two blocks from your home" that provide services to individuals with a criminal history, schizophrenia, drug or alcohol abuse, or HIV-AIDS. These items were assessed by using a 4-point Likert scale, with responses ranging from 1, "extremely unsupportive," to 4, "extremely supportive."
Knowledge about schizophrenia was measured with a ten-item multiple-choice test that was part of a larger knowledge test initially designed to assess level of knowledge about schizophrenia among lay community members, family members of patients with schizophrenia, and police officers. Possible scores on this version of the knowledge test range from 1 to 10, with higher scores indicating greater knowledge about schizophrenia. For the assessment of social distance (which is a manifestation of stigma) toward people with schizophrenia, a six-item modified version of the Social Distance Scale was used (
13 ). An example of a social distance item is, "How comfortable would you be working with a person with schizophrenia?" Police officers rated their level of comfort in six situations with a 4-point Likert scale, ranging from 1, "very uncomfortable," to 4, "very comfortable." Possible scores range from 6 to 24, with higher scores indicating a lesser degree of social distancing. The Cronbach's alpha internal consistency coefficient for this scale was .85 for both the pre- and posttest.
The Emory University Institutional Review Board approved the protocol. The first page of the pretest survey was a participant information document, which notified participants that completing the survey implied consent to use the information. Signatures were not required in order to maintain anonymity. Pre- and posttest surveys were linked by using a unique identifier. Officers were given the pretest survey on the Monday morning of the training week, and the posttest survey was administered on Friday at the end of the training. Completion of each survey required approximately 15 minutes.
All descriptive statistics and hypothesis tests were conducted with the SPSS 11.0 statistical software package (
14 ). Differences between pre- and posttest scores were tested with the McNemar chi square test, the Wilcoxon signed-rank test, and the paired-samples Student's t test, for dichotomous, ordinal, and continuous variables, respectively.
Results
Of the 159 officers the mean±SD age was 37.8±8.1 years, with 72 officers (45 percent) aged between 31 and 40 years. Forty-four officers (28 percent) were female. Approximately half of the sample (83 officers, or 52 percent) self-identified as black or African American, 74 (47 percent) self-identified as white, and two (1 percent) self-identified as being from another racial or ethnic group. A total of 136 officers (86 percent) had attended some college or had completed college, and 92 officers (58 percent) reported a yearly household income of greater than $50,000. Participants had worked as police officers for a mean of 10.1±6.9 years.
Although only 17 officers (11 percent) reported ever having received psychiatric treatment, 48 (30 percent) reported a family history of psychiatric treatment, and 83 (52 percent) reported having known someone in psychiatric treatment. Eleven (7 percent) reported a family history of schizophrenia, and 67 (42 percent) reported ever having known someone with schizophrenia. Ninety-six (60 percent) responded on both the pre- and posttest that they had arrested someone with an obvious mental illness, whereas 39 (25 percent) reported on both surveys that they had not. However, 17 (11 percent) officers responded at baseline that they had not made such a prior arrest and then reported in the posttest that they had done so (p=.04).
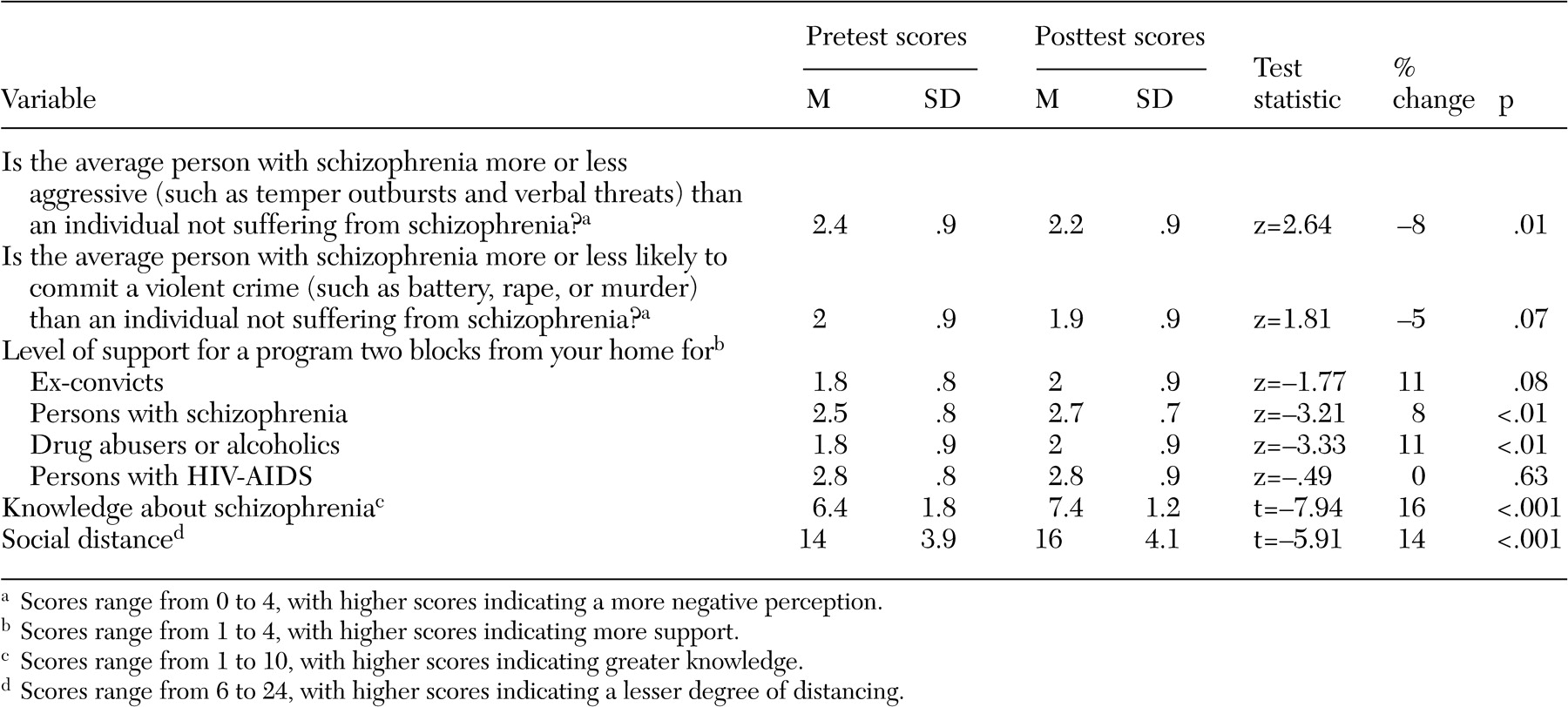
As shown in
Table 1, attitudes regarding aggressiveness among individuals with schizophrenia improved by the end of the training week (p= .01). Levels of support for local treatment programs for schizophrenia and substance use disorders also improved from baseline to course completion (p<.01 for both). Officers demonstrated enhanced knowledge about schizophrenia at the posttest compared with baseline (p<.001). Officers also reported lower levels of social distance toward individuals with schizophrenia upon completion of the training (p<.001).
Correlation analyses did not reveal significant associations between level of knowledge about schizophrenia and social distance at either the pre- or posttest survey. However, compared with officers who reported never having known someone with schizophrenia, those who had known someone with the illness reported less social distance at both the pretest (score of 15.5±4.0 compared with 13.1±3.6; t=3.67, df=139, p<.001) and the posttest (17.2±4.0 compared with 15.2±4.0; t=2.94, df=138, p< .01). When the sample was divided into those who had known someone with schizophrenia and those who had not, both subgroups had statistically significant (p<.001) improvements in social distance.
Discussion
CIT programs are being implemented in numerous localities throughout the United States, and this study is the first to document changes in knowledge, attitudes, and social distance regarding schizophrenia among participating officers. By using a relatively simple survey design, it was shown that after the training, officers reported improved attitudes regarding aggressiveness among individuals with schizophrenia, more support for local treatment programs for schizophrenia, greater knowledge about schizophrenia, and lower levels of social distance. Thus this study supports the hypothesis that an educational program for police officers may reduce stigmatizing attitudes toward persons with schizophrenia.
Prior research suggests that CIT programs may be effective at reducing unnecessary arrests, minimizing the use of force, and increasing referrals to psychiatric facilities (
6,
9,
11 ). The findings here indicate that CIT programs may effectively correct myths, enhance understanding and support, and reduce reports consistent with holding stigmatizing attitudes in the context of officers' responding to calls involving individuals with schizophrenia. This may lead to improved rapport-building skills, deescalation abilities, and communication between officers and family members; improved patient and officer safety; better outcomes for patients in terms of referrals to mental health services; and fewer incarcerations for minor infractions related to externalizing behaviors of serious mental illnesses.
Several other interesting findings that were not part of the original hypotheses deserve further attention. First, there was a relatively high level of familiarity with mental illnesses and schizophrenia in particular among officers entering CIT training. This suggests that officers who volunteer for CIT training may be interested in learning more about mental illnesses in part because of past personal, family, or work-related exposure to mental illnesses or psychiatric care. Second, the findings suggest the possibility that recognition or recall of past encounters with individuals with mental illnesses may improve after CIT training. Officers may interact with individuals with recognizable behaviors that are not attributed to mental illnesses until the officers receive specialized training. Third, it appears that officers who report having known someone with schizophrenia have lower levels of social distance and that receiving training about mental illnesses further reduces this form of stigma. Thus, in addition to classroom teaching, exposure to individuals with mental illnesses may be an effective means of reducing stigma.
Overall, the main findings may have implications in terms of service provision, patient outcomes, policy, and funding. First, in addition to the goals of creating a more educated law enforcement community, enhancing collaborations between criminal justice and the mental health professions, and increasing officer and citizen safety, CIT programs likely foster diversion from jail to treatment for those with mental illnesses. Second, because of greater efficiency in obtaining treatment, patients interacting with CIT-trained officers may have better outcomes compared with patients interacting with officers who have not received such training. Third, policy and funding decisions regarding implementation of CIT programs are likely to be influenced at least in part by demonstration of outcomes such as those described here.
Since deinstitutionalization began, service providers other than mental health clinicians have assumed larger roles in responding to individuals with mental illnesses living in communities. Similarly, jails have become de facto psychiatric institutions for individuals who have not been identified as having a mental illness or who have not been engaged in community mental health programs. CIT is one important effort to better train nonclinician responders to more appropriately serve people with mental illnesses in the community.
Notwithstanding the importance of CIT in decriminalizing behaviors that may stem from mental illnesses, this training should not be viewed as the sole strategy for communities to ensure that people with serious mental illnesses in crisis have access to appropriate care. Mobile psychiatric assessment teams, crisis deescalation teams based in hospitals, and assertive community treatment teams may be preferred strategies to ensure that people with mental illnesses are not criminalized. However, until more appropriate, progressive community mental health initiatives are developed to reclaim responsibility for treatment of individuals with serious mental illness in the community, CIT programs remain an important strategy to redirect people with mental illness away from the penal system and toward mental health services.
Several methodological limitations of this study should be considered. First, these findings are based on a relatively limited array of items measuring knowledge, attitudes, and social distance. The items assessing attitudes regarding aggressiveness and violence among individuals with schizophrenia serve only as a proxy for stigmatizing beliefs, and the measures of support for treatment programs and social distance are imperfect. Future studies should continue to address attitudes among officers that might predict problems when interacting with psychiatric patients. Additionally, some of the results, although achieving statistical significance, were fairly small in terms of absolute changes. Studies of actual interactions between CIT-trained police officers and disturbed patients whom they encounter are needed. Second, the lack of a control group may limit the interpretation of findings. Third, social desirability bias may have influenced responses on the posttest, because officers likely knew that an improvement in attitudes was expected. The differences among the trainees (those with and without prior exposure), as well as improvements in more objective knowledge scores, however, suggest that other factors are at work besides the influence of social desirability. Fourth, this survey focused on knowledge, attitudes, and social distance in relation to schizophrenia. Although research suggests that CIT officers may be more likely to interact with individuals who have schizophrenia than with those who have mood disorders (
15 ), knowledge and attitudinal changes related to other psychiatric illnesses should be similarly assessed.
Conclusions
These results may provide a starting point for additional research into this important and expanding collaborative effort between mental health and law enforcement. This study points to an urgent public health need to prospectively study the impact of CIT and similar training programs on police officers' interactions with and responses to persons with mental illnesses.
Acknowledgments
The authors acknowledge the following individuals for their support of Georgia's CIT training program: David W. Covington, Vernon M. Keenan, Nora Lott-Haynes, David J. Lushbaugh, Dale Mann, J. Terry Norris, Frank V. Rotondo, Gwendolyn B. Skinner, and all members of the Georgia CIT Advisory Board.