Providing mental health care to patients with combined neuromedical and psychiatric illness presents a special challenge. This study focused on people with multiple sclerosis, a group that has high needs for mental health care as well as treatments and services to manage their neurologic disease. Depression is the most common psychiatric condition among people with multiple sclerosis (
1 ), with an estimated 50 percent lifetime rate of depression by the age of 59 years (
2 ). Rates of major depressive disorder are significantly higher among people with multiple sclerosis than in the general U.S. population (
3 ). The Goldman Consensus Group (
4 ) recommended psychotherapeutic and psychopharmacologic treatments as effective for depressive syndromes among patients with multiple sclerosis.
We are interested in urban and rural differences in behavioral health services provided to patients with multiple sclerosis and affective disorders. In general, rural residents face barriers to mental health care, including fewer local mental health providers, longer distance to specialty services, lack of insurance, social stigma, and a tendency to rely on family and other informal support (
5,
6 ). Primary care physicians provide a large proportion of mental health care in rural areas. They have few mental health specialists to refer patients to, and they treat more cases of depression on their own than their urban counterparts (
7 ). Kessler and colleagues (
8 ) found that people treated for emotional disturbances in rural areas were less likely than those in urban areas to receive mental health care from sectors of health services included in their study. The objectives of our study were to identify any urban and rural differences in mental health needs and treatments among people with multiple sclerosis, as well as their satisfaction with mental health care.
Methods
The data presented in this study were collected in a nationwide survey of 1,518 people with multiple sclerosis. The survey focused on urban and rural differences in a range of health services, including mental health care. We developed three subgroups: metropolitan statistical areas (urban areas), rural areas located within 50 miles of a metropolitan statistical area (adjacent rural areas), and rural areas located more than 50 miles from a metropolitan statistical area (more remote rural areas). Members of the National Multiple Sclerosis Society were stratified by their residential zip codes into one of these subgroups. A random sample of 3,500 members was then chosen by computer to recruit 500 participants for each urban or rural subgroup. The Institutional Review Board for Human Subjects in Research at Texas A&M University approved the survey questionnaire.
Potential survey respondents were selected from each urban and rural random sample of 3,500 people to receive prenotification mailings. Materials explained the purpose of the study and included a toll-free number to call to participate in a computer-assisted telephone interview. Prenotification mailings continued until at least 500 participants completed interviews for each of the three geographic subgroups. The survey process began in October 2004 and was completed in January 2005. A total of 5,181 prenotification letters were mailed, with 263 returned as undeliverable, and 1,518 society members completed the telephone survey (31 percent participation rate). Interviews were completed by 505 people with multiple sclerosis in urban areas, 500 respondents in adjacent rural areas, and 513 respondents in more remote rural areas.
Although we had a relatively low participation rate (31 percent), our urban sample closely matched a sample of people with multiple sclerosis who participated in the Slifka study (83 percent from urban areas) on demographic and disease characteristics (
9,
10 ). For example, our urban sample and the Slifka sample had nearly identical proportions of women, Caucasians, and married people. The Slifka study was designed to create a representative sample of people with multiple sclerosis (
10 ). Our urban subgroup was similar to the Slifka sample for disease characteristics, such as average number of years since diagnosis of multiple sclerosis (13.3 years compared with 13.0 years), the course of multiple sclerosis (relapsing or remitting, 59 percent compared with 58 percent), difficulty walking (65 percent compared with 67 percent), and overall health status.
Self-reported data (for example, the practice specialties of physicians) and measurement of satisfaction with care have limitations. We minimized self-reporting problems by asking in the prenotification letter that respondents be prepared to discuss during the interview the types of physicians seen in the past 12 months. In addition, face validity testing of the questionnaire was performed by members of the study team with expertise in multiple sclerosis care and by staff at the National Multiple Sclerosis Society. To improve reliability, the questionnaire was also pretested on 11 people with multiple sclerosis before the survey process began (
11 ). Similar to other studies assessing patient satisfaction, including patients with multiple sclerosis (
12,
13,
14,
15 ), our study used a Likert scale to assess patient satisfaction with mental health care.
Survey results were analyzed with the SAS statistical package. To test for statistically significant urban and rural differences, we used two sample z tests for comparisons of proportion, such as diagnosis of depression, and for continuous variables, such as age.
We used the two-way contingency table chi square test for categorical data, including type of treatment. The urban subgroup was used as the reference group in the calculation of statistically significant differences. If the chi square test was significant when we compared each rural subgroup with the urban subgroup for race or type of treatment, we concluded that the two subgroups had significantly different percentages across categories for this characteristic. Because our focus was to identify urban and rural differences, we did not use a one-way analysis of variance (ANOVA) for the three subgroups simultaneously. We wanted to test for possible differences in survey characteristics between each rural subgroup and the urban subgroup, whether or not a one-way ANOVA would show a significant overall difference for this characteristic.
Results
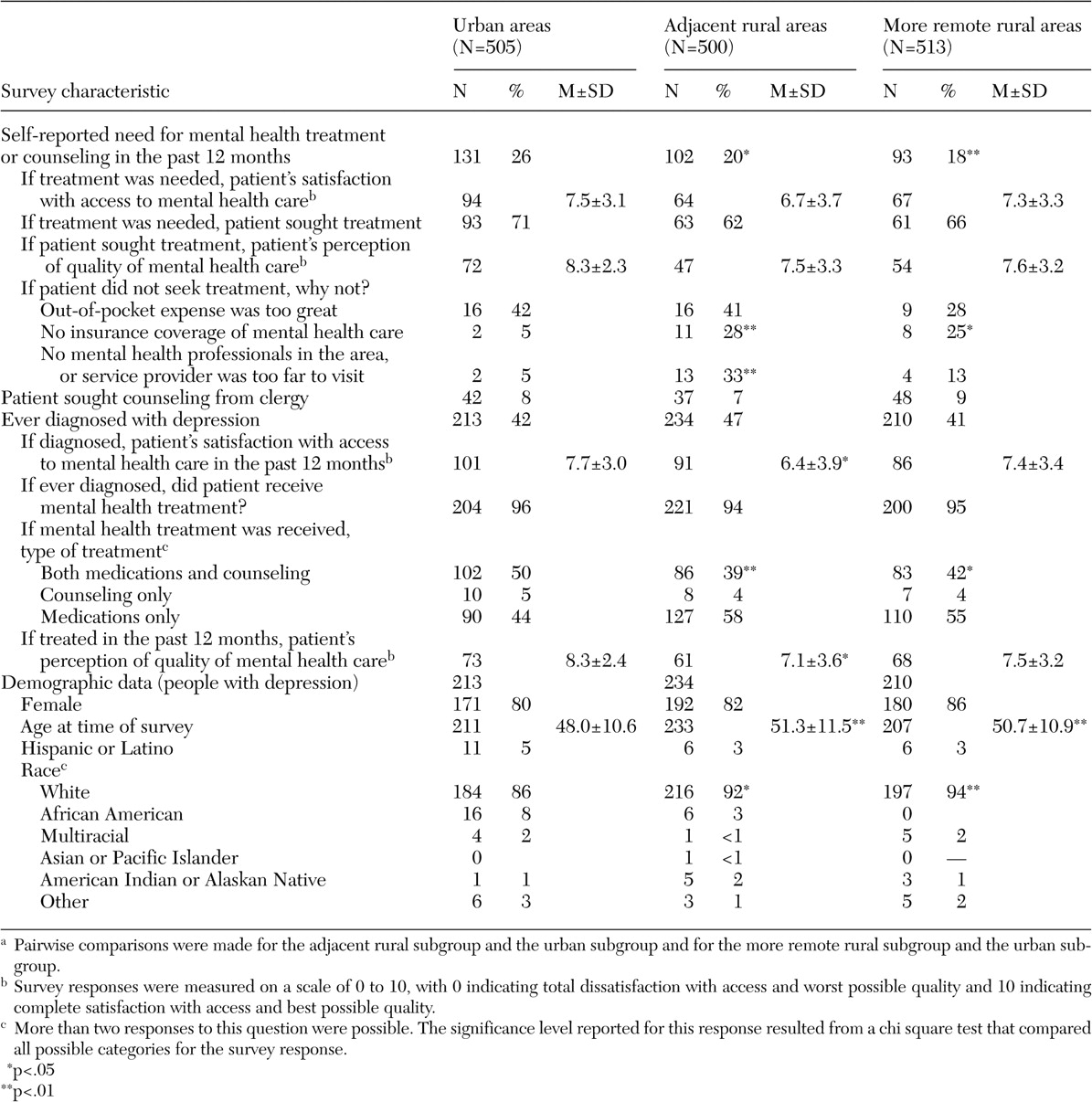
Survey results, as well as demographic characteristics of our study samples, are presented in
Table 1 . The interviewer asked if respondents felt that they had needed treatment or counseling from a mental health professional for a personal or family problem in the past 12 months. Significantly smaller proportions of respondents in the rural subgroups than in the urban subgroup reported a need to seek this counseling. However, there were no significant differences between urban and rural groups in the proportions of people with multiple sclerosis who sought counseling or in levels of satisfaction with access to mental health care. There also were no significant differences between subgroups in perceptions of the quality of mental health care received by those who sought treatment. However, significantly larger proportions of people with multiple sclerosis in rural areas who did not seek treatment reported that they had no health insurance coverage for mental health care compared with people in urban areas. Among those who had not pursued treatment, a significantly larger proportion of people with multiple sclerosis in adjacent rural areas than in urban areas replied that there were no mental health professionals in their area.
More than 40 percent of people with multiple sclerosis in each geographic subgroup responded that they had been diagnosed as having depression during their lifetime. More than 90 percent of people with a diagnosis of depression in each urban and rural subgroup received treatment. However, people with multiple sclerosis in adjacent rural areas with a diagnosis of depression were significantly less satisfied with their access to mental health care in the previous 12 months and perceived that their care was of lower quality than that of their urban counterparts.
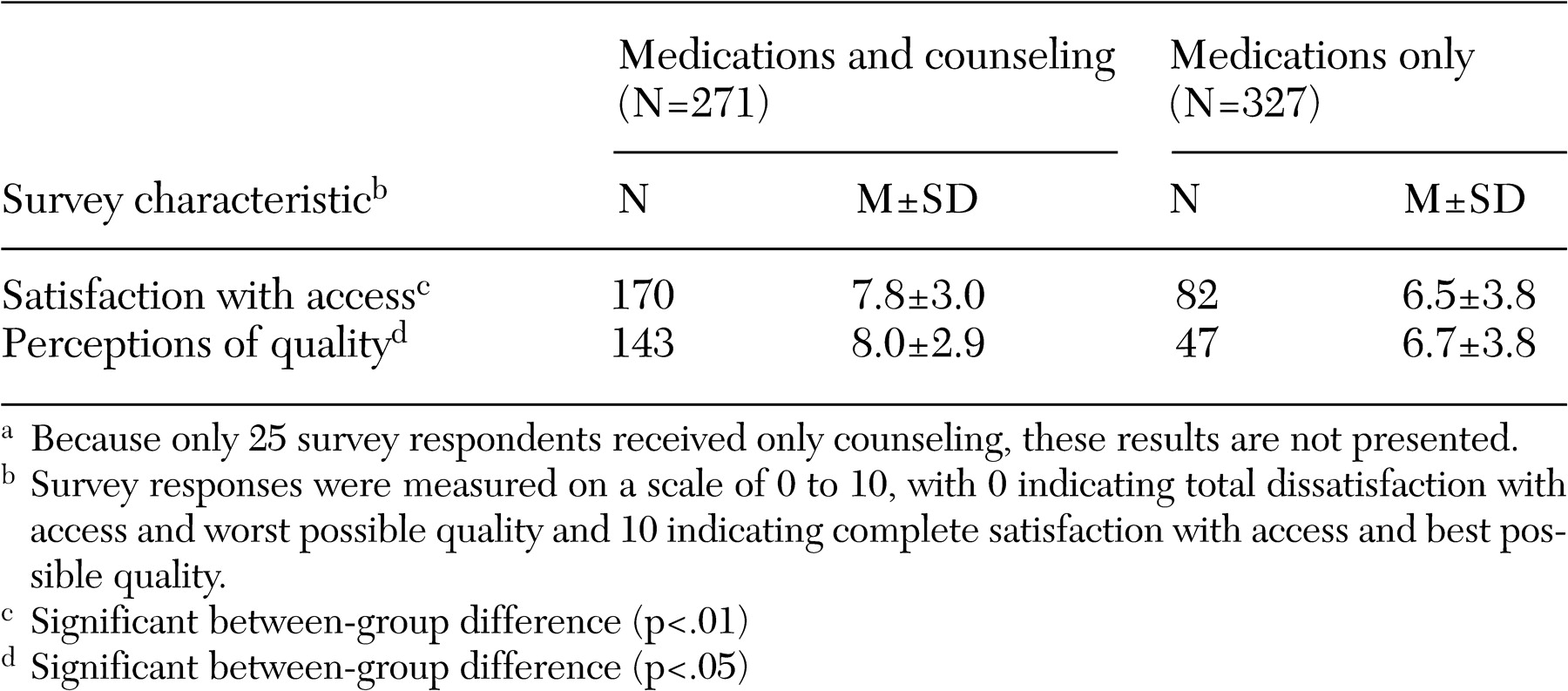
Among people with multiple sclerosis treated for depression, a significantly larger proportion of people in urban areas than in rural areas received both counseling and antidepressants. (Treatment options provided in the interview were "both medications and counseling," "counseling only," or "medications only.") Survey responses were regrouped by type of treatment received for depression to identify any differences in levels of satisfaction with access to and quality of mental health care received. As
Table 2 indicates, patients with multiple sclerosis who were treated for depression with both medications and counseling averaged significantly higher levels of satisfaction with access to mental health care and the quality of that care than those who received only medications to treat depression.
Discussion and conclusions
Our results demonstrate the relatively disadvantaged status of the two rural subgroups regarding access to mental health care for people with multiple sclerosis. Significantly larger proportions of the two rural subgroups reported inadequate health insurance coverage for mental health care compared with the urban subgroup. In addition, rural dwellers were more likely to report inadequate numbers of mental health providers in their areas, and they were more likely to be dissatisfied with the quality of mental health care received. Rural residents with multiple sclerosis were also significantly less likely than their urban counterparts to receive the recommended combination of medications and psychotherapy for treatment of depression.
More than 90 percent of respondents who reported depression responded that they had received mental health services, regardless of urban or rural residence. On the basis of these analyses, we conclude that current mental health systems, even in rural areas, are capable of reaching out to patients with neuromedical illnesses, such as multiple sclerosis. However, we observed significant patient-perceived limitations in quality and accessibility among people with multiple sclerosis in rural areas, as well as differences in rural and urban settings in offering the recommended treatment of combined medication and psychotherapy. We also found that patients with multiple sclerosis who were treated for depression with medications and counseling had significantly higher levels of satisfaction with access to mental health care and the quality of that care than patients with multiple sclerosis who received only medications for depression.
Acknowledgments
This research was supported by contract HC-0038 from the Health Care Delivery and Policy Research Program of the National Multiple Sclerosis Society. In addition, Dr. Wang's research was supported in part by grant P30-ES09106 from the National Institute of Environmental Health Sciences to the Texas A&M University Center for Environmental and Rural Health for statistical methodology research and its applications to the health sciences. The authors thank Nicholas LaRocca, Ph.D., for his assistance with this research.