In the aftermath of the attacks of September 11, 2001, the New York State Office of Mental Health (NYOMH) implemented Project Liberty, a program that provided free crisis counseling services to persons and groups affected by the World Trade Center disaster. Project Liberty was funded by the Federal Emergency Management Agency (FEMA) and the Center for Mental Health Services, and it was a collaborative effort among the NYOMH, local governments, and provider agencies in order to reach individuals in the five boroughs of New York City and surrounding counties. Project Liberty offered one-to-one or group sessions wherever the service recipients wished to have them: in their homes, at a community agency, at a school, at a business, or elsewhere in the community.
Project Liberty subsidized the demand for counseling services related to the disaster by providing free care. The payment agreement with provider agencies was similar to the terms used with public insurance programs, such as Medicaid or Medicare. On a voluntary basis, some community-based public mental health agencies in New York City participated in the emergency program and devoted a large proportion of staff and a major proportion of management effort to Project Liberty.
During the first year of the project, the agencies that agreed to become Project Liberty providers were paid on a fee-for-service basis for the provision of individual and group counseling and group public education sessions (fee schedule for each type of visit). The bulk of services provided (more than 95 percent of the logs of service encounters) was directed toward counseling activities (
1 ). Only provider agencies outside of New York City and a small group of provider agencies serving special populations were paid on a cost basis, in which payments were based on the cost estimate of providing the anticipated volume of services. In September 2002 there was a change in reimbursement, from a fee-for-service system to a cost-based system for all Project Liberty provider agencies in the city.
This study examined the impact of the September 11, 2001, attacks and Project Liberty on mental health service provider agencies in New York City and surrounding counties. In particular, we analyzed whether the introduction of Project Liberty services affected the ability of agencies to supply community-based services provided by Medicaid, the main public program for people with serious mental illnesses. The World Trade Center disaster was the largest terrorism event in U.S. history, creating a huge and immediate need for mental health services in areas most affected by the attacks. Results from a survey conducted in the Manhattan area in the aftermath of September 11, 2001, showed that 7.5 percent of adults reported symptoms consistent with a diagnosis of current posttraumatic stress disorder and 9.7 percent reported symptoms consistent with current depression (
2 ).
Despite the new funds available to pay for Project Liberty services, the introduction of a new, large program to meet emergency needs may have diverted the community agencies' resources away from the supply of other mental health services. In the first nine months of Project Liberty, the volume of services provided by Project Liberty was comparable to the volume of services delivered by mental health programs in the region for the entire 1999 calendar year, which raised concerns among policy makers and researchers of a potential shortfall of other services provided in the mental health system (
3 ).
The FEMA regulations stipulated that Project Liberty funds were to be used to provide short-term, crisis counseling services that would supplement, not supplant, existing mental health services. Part of the application process for the federal funding required the state to conduct a needs assessment and demonstrate that existing mental health services were insufficient to meet the expected need. If provider agencies needed to divert staff or management time in order to provide Project Liberty services, participation in this program could have affected the provision of traditional services, particularly to Medicaid beneficiaries. Investigating how Project Liberty affected other services that agencies provide can be helpful in assessing the capacity of the mental health system to respond to disaster-related demands for mental health care.
Methods
We combined data at the level of the provider agency from two sources. The first source was the Project Liberty logs of service encounters, which contain information on each counseling or educational session provided. For this analysis the encounter-level data were aggregated by month for each provider agency. The second source was a datamart maintained by the state that contains summary information about Medicaid claims and corresponding payments related to mental health services. These data were also available on a monthly basis. We tracked Medicaid and Project Liberty services over time to check whether participation in Project Liberty diverted supply from Medicaid.
Project Liberty services were measured by number of Project Liberty visits. Volume of Medicaid services was measured in terms of amount of dollars claimed by a provider agency. This is an appropriate measure for Medicaid activities because it allows us to summarize in one number the volume of the varied mental health services provided by each community agency or hospital. Because not all mental health provider agencies in New York City and surrounding counties participated in Project Liberty, we were able to include a natural comparison group of provider agencies that were not participating in Project Liberty as a control for potentially confounding time trends.
We calculated statistical means of the volume of services provided by Project Liberty provider agencies and the comparison group. In addition, we used the data on provider agencies over this same period (January 2000 to June 2003) to estimate the impact of number of Project Liberty visits on the volume of Medicaid services. For that purpose, we estimated least-squares regressions with time random effects to account for correlations within provider agencies over time. We estimated these regressions in levels of Medicaid services measured in claimed dollars and in logarithms of this variable in order to account for the asymmetry of its distribution and have a better fit.
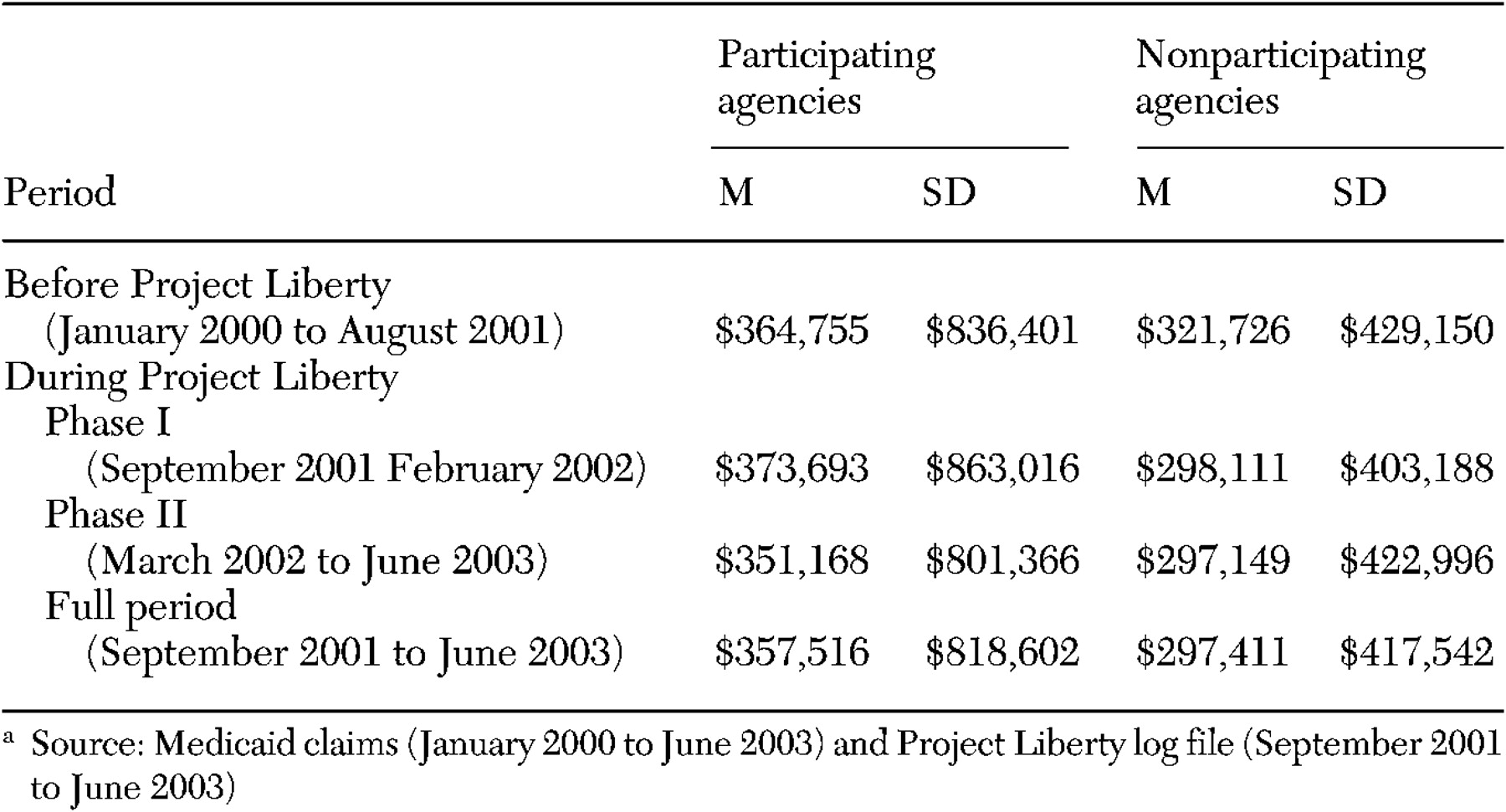
Provision of Medicaid services was examined for four periods: before Project Liberty was introduced (January 2000 to August 2001), during phase I of Project Liberty (September 2001 to February 2002), during phase II of Project Liberty (March 2002 to June 2003), and during phase I and II of Project Liberty (September 2001 to June 2003).
Results
In our sample, 164 provider agencies participated in Project Liberty, and 94 provider agencies were in the comparison group of agencies that did not participate in this program. According to our analysis, the volume of Medicaid services was not affected. As shown in
Table 1, before September 11, 2001, the group of mental health provider agencies that participated in Project Liberty was providing, on average, a slightly higher volume of Medicaid services than the comparison group. After September 11, 2001, and the introduction of Project Liberty, participating provider agencies continued to be larger providers of Medicaid services than the comparison group. The increase in the average number of Project Liberty visits observed in the second phase of the program does not appear to have affected the volume of Medicaid services. Compared with the period before Project Liberty was introduced, the decrease in the aggregate volume of Medicaid services was smaller for provider agencies that participated in Project Liberty than for the comparison group.
Provider agency-level regression analyses confirmed these results. The estimate of the mean±SE impact of a Project Liberty visit on the monthly dollars claimed for Medicaid services was not statistically significant; compared with the group of nonparticipating agencies, agencies participating in Project Liberty claimed a mean decrease of $2.20±2.34 in Medicaid services per month per Project Liberty visit. When we restricted the period of analysis to the first year of Project Liberty, when fee-for-service payments were in place, the point estimates of the impact of Project Liberty were small and not statistically significant (data not shown).
When separate regressions were estimated for agencies with only one site (27 agencies, 19 of which provided services to Project Liberty) and agencies with multiple sites (104 agencies, 71 of which provided services to Project Liberty), the point estimates of the impact of Project Liberty were different, although they were not statistically significant. Compared with the period before September 11, 2001, after the attacks agencies with one site that participated in Project Liberty claimed, on average, $4.66±3.57 less for Medicaid services per month per Project Liberty visit (p=.192). Similar regressions in logarithms produced estimates in the same direction; however, in this second specification, a negative impact on Medicaid services (least-squares coefficient of −.089±.025) provided by smaller agencies was statistically significant (p<.001). For the larger agencies, compared with the period before September 11, 2001, after the attacks we found a positive impact on Medicaid services of $4.66±.36; however, results were not significant in the regression either in levels or in logs.
Discussion
The impact of disaster relief programs on providers' regular activities has not been explored. For example, an evaluation of Project Heartland, Oklahoma's mental health program implemented in response to the 1995 bombing (
4 ), did not include any study on this matter. Although the disasters may be a short-term event, elevated mental health needs of affected persons extend over months and years, raising the question of whether providing services to meet these ongoing service needs may crowd out other community-based mental health services.
The unprecedented dimensions of the terrorist attacks of September 11, 2001, and of the relief efforts implemented in its aftermath called for an evaluation of the effects on provider agencies and on continued access to services by the users of regular services. Previous research has pointed out a limited leeway among mental health providers in the New York City metropolitan area and a risk of shortfall in services (
3 ).
In terms of implications for policy in the event of subsequent disasters, our results should be interpreted with caution. The New York City metropolitan area is different from other areas in the country for many reasons, beginning with the city's sheer size. Also, there was more availability of mental health professionals for relief efforts than there might be in other areas. In addition, the terrorist attacks disproportionately affected those with private insurance (
5 ). Many of those working around Ground Zero were employed and insured, which may have also led to noteworthy utilization patterns in private insurance plans and their networks of providers. Should future disasters affect areas with lower rates of private insurance, comparably funded relief efforts may put a greater strain on public mental health services.
Conclusions
Our results suggest that overall the supply of Project Liberty services was not associated with a lower supply of Medicaid services. Only in smaller agencies with only one site did we find a small, but statistically significant, negative impact.
Project Liberty was implemented immediately after September 11, 2001, and some agencies provided a high volume of services. Yet Project Liberty was a flexible, demand-side financing program that was voluntary on the part of community agencies. Agencies choosing to participate were able to offer Project Liberty services without displacing other services. By design, most Project Liberty services provided one-to-one or group sessions in community settings (
1 ). These services were provided wherever the service recipients wished to have them—at a community agency, at a school or business, in their homes, or elsewhere in the community. This flexibility may have minimized diversion of agency-fixed resources, such as clinic office space, from traditional services.
The program model also included the use of paraprofessionals, persons who were not licensed mental health clinicians but who were part of and knowledgeable about the diverse communities and therefore able to do effective outreach. These staff received training in crisis counseling techniques to prepare for that role and represented an extension of the supply of persons able to provide Project Liberty services.
Acknowledgments
This evaluation was funded by grant FEMA-1391-DR-NY (titled "Project Liberty: Crisis Counseling Assistance and Training Program") to New York State from the Federal Emergency Management Agency. The Center for Mental Health Services of the Substance Abuse and Mental Health Services Administration administered the grant.