The relationship between psychiatric disorders and risky behaviors associated with HIV is not well documented in representative samples of homeless individuals. Often, in assessing psychiatric and substance abuse and dependence disorders in the homeless population, researchers have used different instruments, thereby limiting the comparability of the existing studies.
In addition, there is some variation in the measurement of sexual behaviors associated with contracting HIV among homeless individuals with mental illness and a substance use disorder. For instance, some studies have focused on single behaviors, whereas others have thoroughly assessed a range of sexual behaviors that place individuals at risk for negative outcomes (
1,
2,
3 ). Thus the exact relationship between mental illness, substance use disorders, and HIV risk remains unclear. The goal of this study was to assess the relationship between psychiatric disorders and HIV risk behaviors in a probability sample of homeless adults.
HIV risk behaviors are commonly reported among homeless adult men and women. Prevalence estimates derived from a sample of 224 patrons using services at homeless shelters, soup kitchens, outpatient mental health clinics, and community centers suggest that 51% of homeless adults engaged in high-risk sexual behaviors (
4 ), including sex with multiple partners, inconsistent condom use, needle sharing, and trading sex for money or drugs (
5,
6,
7 ). These behaviors are likely to contribute to increased rates of HIV and AIDS.
Prevalence estimates of HIV-AIDS infection vary greatly among the homeless population. Among shelter and soup kitchen users, rates of HIV-AIDS infection range from 2% to 16% (
8,
9 ). In a large study of out-of-treatment drug users (N=16,366), the highest rates of HIV-AIDS (19%) were reported among homeless individuals living on the street (
10 ). Among individuals presenting at an urban emergency department (N=340), 35% of homeless individuals were HIV positive, compared with 13% among a nonhomeless control group (
11 ). Among homeless adults utilizing inpatient psychiatric services, studies have shown that approximately 6% were infected with HIV (
12,
13 ). One study with a sample of 315 reported a 12% HIV seroprevalence among homeless, mentally ill men who abused substances and were receiving psychiatric services in a residential treatment community (
14 ). Although these estimates are likely to reflect differences in HIV risk behaviors in a heterogeneous homeless population, reliance on convenience samples limits the interpretation of HIV infection rates in the homeless population.
The rates of substance abuse and dependence among homeless individuals generally have been higher than in the general population (
15,
16 ). In a review of the literature examining various modalities of measurement to assess lifetime prevalence rates of substance abuse among homeless individuals—that is, structured clinical interviews, the Diagnostic Interview Schedule (DIS), and the Short Michigan Alcohol Screening Test—lifetime rates of alcohol abuse ranged from 4% to 86% and lifetime rates of drug abuse ranged from 1% to 70% (
17 ). In another review of nine studies, all using the DIS (
18 ), the authors indicated a mean lifetime prevalence rate of 56% for alcohol abuse or dependence and 43% for drug abuse or dependence.
Elevated rates of mental illness also have been reported among homeless individuals. A review of the literature suggests that prevalence rates have ranged from 1% to 30% for schizophrenia among homeless adults and from 2% to 30% for mood disorders (
17 ). In another study, lifetime rates of psychiatric problems were assessed by using the DIS across nine studies, and the authors reported a mean lifetime rate for mood disorders of 21% (mostly depression) and 6% for schizophrenia (
18 ).
In examining the relationship between psychiatric disorders, substance use disorders, and HIV risk behaviors, researchers seldom rely on representative samples of homeless individuals. Because it is costly and time consuming to use sophisticated sampling methods, researchers often rely on convenience samples of individuals living in shelters (
2,
14,
19 ), samples of homeless adults involved in inpatient or outpatient psychiatric treatment (
3,
14,
19,
20 ), or street-based samples (
6,
10,
21,
22,
23 ). Thus the goal of this study was to assess the relationships between psychiatric disorders and HIV risk behaviors by using a probability sampling design among the adult homeless population.
Furthermore, in assessing psychiatric disorders and substance abuse or dependence among homeless samples, many researchers rely on scores generated by self-report symptom checklists (such as the Symptom Checklist-90 or the Brief Symptom Inventory) to determine the presence of psychiatric disorders (
1,
22,
24,
25 ). These measures reflect the individual's distress level only at the time of self-report, without providing a reliable diagnosis. In other studies, participants are asked to report a history of psychiatric hospitalization and diagnoses in order for investigators to determine the presence of psychiatric disorders (
11,
12 ). Thus individuals who have never been hospitalized for psychiatric disorders and untreated individuals may be overlooked because they do not have access to mental health services.
The use of structured interviews is a more rigorous method of assessing psychiatric disorders and substance abuse and dependence. Other studies have used structured clinical interviews for assessing
DSM-IV criteria such as the DIS or the Structured Clinical Interview to assess psychiatric disorders among homeless individuals (
19,
26,
27 ). Although structured interviews are time consuming and require adequate interviewer training to ensure interrater reliability, they remain an effective method to examine the prevalence of psychiatric disorders, including mood and substance-related disorders as well as schizophrenia. Structured interviews also allow a more accurate differentiation between substance-related disorders and other psychiatric disorders (
28 ).
The goal of this study was to examine the individual contributions of psychiatric disorders and substance use disorders to HIV risk behaviors in a probability sample of homeless adults by using a structured clinical interview—the DIS—to yield DSM diagnoses of psychiatric disorders as well as substance abuse or dependence and by using a measure of HIV risk behaviors that assesses a wide range of sexual behaviors.
Methods
Sample
Using a probability sampling design patterned after a study by Toro and colleagues (
29 ), we interviewed 218 homeless adults from a large Midwestern city. As part of the probability sampling strategy, we conducted key informant surveys before conducting interviews. Our goal was to determine the total number of homeless individuals served at various locations in the area. Key informants were individuals from mental health and substance abuse agencies, neighborhood-based community organizations, shelters, food pantries, and other agencies knowledgeable about the homeless population. Informants completed 15- to 20-minute phone surveys regarding familiarity with their geographical sector, which provided estimates of the percentage of homeless individuals who could be found over the course of a year at each of the shelters and food programs in the county.
Next we conducted 443 short sampling surveys across these sites. This survey was used as a screening tool to determine if individuals met our criteria for homelessness. In addition participants were asked to list the services that they had used in the previous year, as well as the frequency of their utilization of these services. This feedback allowed us to refine key informant estimates of where homeless individuals could be found by adjusting our sampling for overlap. In turn, these estimates determined the overall number of interviews to be completed at each site. However, because most homeless adults can be found at food programs and shelters (
30 ), we did not sample from other agencies assisting the homeless population. As a result, our sampling strategy may have resulted in oversampling frequent users and undersampling infrequent users. In the urban setting in which this study was completed, most homeless individuals sleep in shelters and use food programs and are less likely to be a street-based population (
29 ).
Participants were adults (mean age of 42 years); 161 (74%) were men and 170 (78%) were African American, 37 (17%) were white, and seven (3%) were Native American. Patrons receiving services at these sites were approached and asked to complete a short sampling survey to determine eligibility to participate in a full-length interview. Participants were eligible to be interviewed if they had been homeless for at least one night within the month before initial contact. Homelessness was defined as not owning or renting a house or an apartment, living on the streets or in a shelter, or staying with friends or family and not paying rent.
Procedure
Staff and graduate and advanced undergraduate students in psychology conducted two-hour face-to-face interviews. Interviewers received extensive training (including role playing, periodic supervised interviews, and weekly staff meetings), and initial interviews were observed to ensure that all measures were administered appropriately. Participants were paid $40 upon completion of the interview. Interviews were conducted at a place that was most convenient for the research participant, such as shelters, soup kitchens, restaurants, libraries, and research offices. Interviews were completed across the seasons, from November 2000 to May 2002. This study was approved by the Wayne State University Institutional Review Board, and all participants gave informed consent. The names of all participants were recorded to ensure that no one was interviewed more than once.
Predictor variables
Background characteristics. In addition to demographic characteristics, respondents were asked to provide other information, such as their age, gender, race and ethnicity, and educational background.
Length of homeless episode at baseline. Respondents' answers regarding the length of homeless episode at baseline were categorized as follows: 0, one to seven days; 1, eight to 14 days; 2, 15 to 19 days; 3, one to two months; 4, three to five months; 5, six to 11 months; 6, 12 to 17 months; 7, 18 to 23 months; 8, 24 to 36 months; and 9, more than 36 months.
Client needs assessment. The client needs assessment scale provides a list of service needs specific to homeless populations, such as finding affordable housing, individual counseling, treatment for problems with drugs or alcohol, and case management. Participants were asked to rate the importance of each service on a 5-point Likert scale that ranges from 1, not important, to 5, extremely important.
DIS. The DIS (version 3A) is a structured diagnostic interview designed to elicit
DSM-III-R criteria for lifetime psychiatric disorders, such as mood disorder (including mania), schizophrenia, and substance use disorders (
31 ). A dichotomous diagnosis for these disorders was assigned to each respondent on the basis of a computer algorithm that operationalizes
DSM-III-R criteria and applies them to data collected by lay interviewers. This instrument has demonstrated adequate reliability and validity and has been used in recent studies of homeless adults (
29,
32,
33,
34 ).
Outcome variable: HIV risk behaviors. Sexual behaviors that may increase the risk of contracting sexually transmitted diseases were assessed among respondents who reported having sexual intercourse within the six months before the study. Several behaviors were assessed with the HIV risk behaviors scale. The result is a sum of the values assigned to several risky behaviors in which each participant engaged. The scale evaluates 13 behaviors: sexual activity in the previous six months (0, no; 1, yes); total number of opposite-sex partners (ranging from 0, no partner, to 3, more than three partners); lifetime prevalence of sexually transmitted diseases (rated from 0, never, to 3, five times or more); ratio of protected sex (rated from 0, for 100% protection, to 3, for 0% protection); trading sex for drugs or money (rated from 0, never, to 4, just about every day); sex without a condom while drunk or high (rated from 0, never, to 4, just about every day); sex without a condom with someone who injected drugs (rated from 0, never, to 4, just about every day); drug injection (rated from 0, never, to 4, just about every day); sex without a condom with someone who had a blood transfusion, who had AIDS, who tested positive for HIV, or whom the individual paid (rated from 0, never, to 4, just about every day); and sex without a condom with a man who had sex with another man (rated from 0, never, to 4, just about every day).
Using the Winsorizing technique, which brings outliers to the next highest value within an acceptable range, we truncated the range of the 0-to-18 scale to a range of 0 to 15 and thus allowed the data to approach normality. These risk indicators were summed in order to derive a total score and construct a scale of HIV risk behaviors (ranging from 0 to 15). These self-reported behaviors were selected because they have been identified as important predictors of sexually transmitted disease (
35 ) and appear to demonstrate face validity (
36 ). In addition, the scale has demonstrated good internal consistency among samples of homeless adolescents (
α =.86).
Results
Preliminary and descriptive analyses
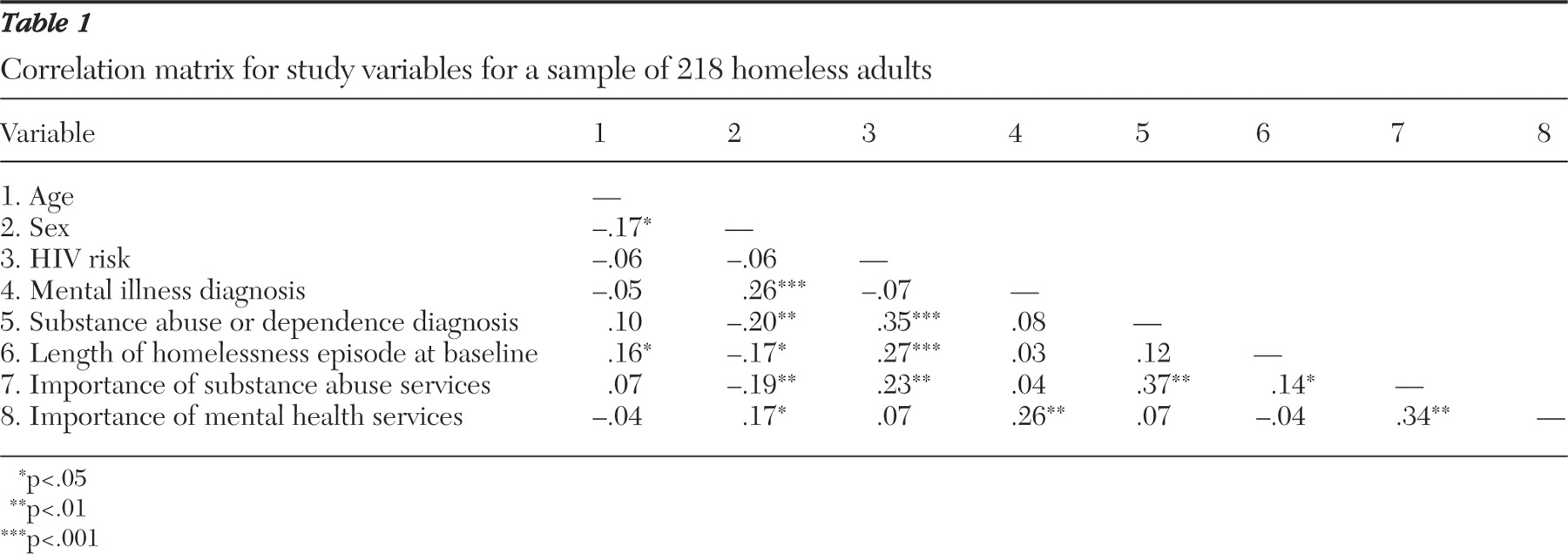
We first made appropriate transformations to allow skewed and kurtotic variables to approach normality. Before conducting the main analysis, we computed bivariate correlations. As shown in
Table 1, HIV risk behaviors were positively related to substance abuse and dependence, length of homelessness episode, and the self-reported need for substance abuse services.
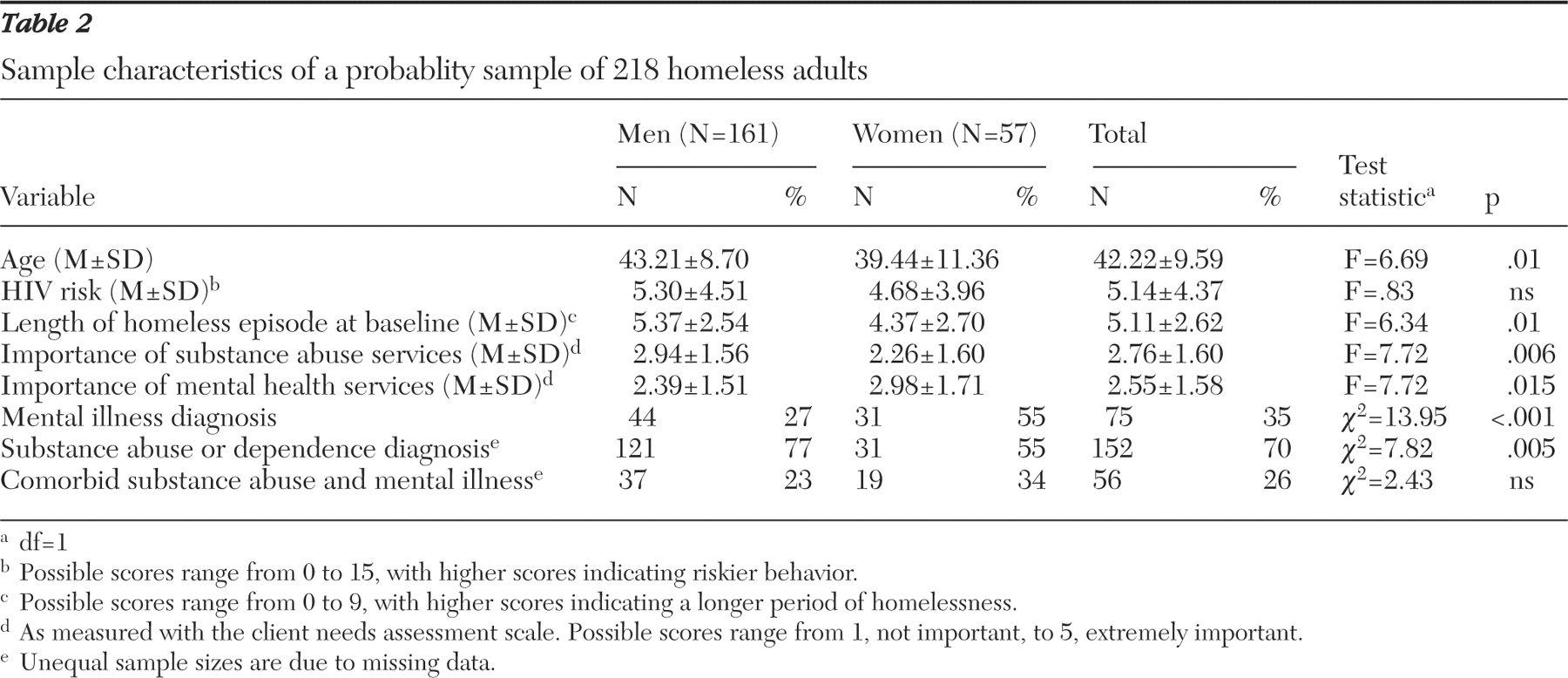
Means and standard deviations for transformed key study variables are reported by gender in
Table 2 . Compared with women, men were more likely to be older, to have experienced a longer period of homelessness at the time of the study, and to present with a diagnosis of substance abuse or dependence rather than a diagnosis of mental illness. In contrast, women displayed equal frequency of mental illness and substance abuse or dependence diagnoses. Although there were no significant differences between men and women regarding the frequency of comorbid substance abuse or dependence and mental illness, 75% of all respondents with mental illness also presented with a diagnosis of substance abuse or dependence. Finally, men rated obtaining substance abuse treatment as more important, whereas women rated obtaining mental health services as more important.
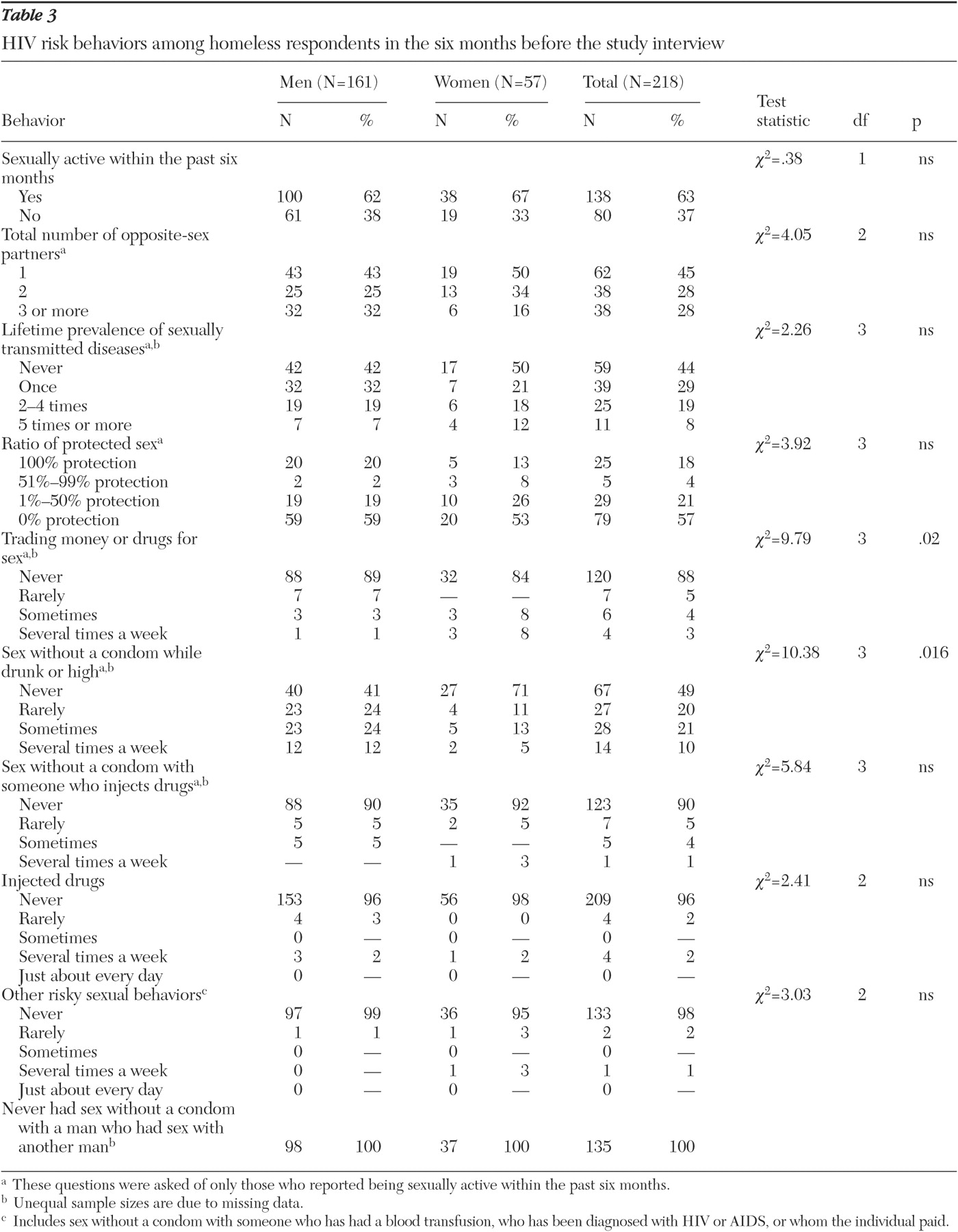
All respondents were asked whether they were HIV positive. Of the sample, seven men (4%) and three women (5%) reported testing positive for HIV-AIDS. As shown in
Table 3, 62% of homeless men and 67% of homeless women were sexually active. Specifically, they reported having engaged in anal, oral, or vaginal sexual intercourse in the six months preceding the interview. Of those who reported being sexually active in the past six months, 75 (56%) had contracted at least one sexually transmitted disease in their lifetime. In addition, among sexually active respondents, 113 (82%) did not use condoms for 100% of encounters involving sexual intercourse and 79 (57%) never used protection. After engaging in sex without consistently using condoms, the most common risky sexual behavior was "having sex without a condom while drunk or high," a behavior that 51% of sexually active respondents endorsed. All respondents were asked about injection drug use within the past six months, and 4% of men and one woman reported using needles to inject drugs.
Although the frequency of HIV risk behaviors was similar across men and women, men were more likely to have sex with a prostitute and while under the influence of alcohol or drugs, whereas women were more likely to trade sex for money or drugs.
Regression analysis
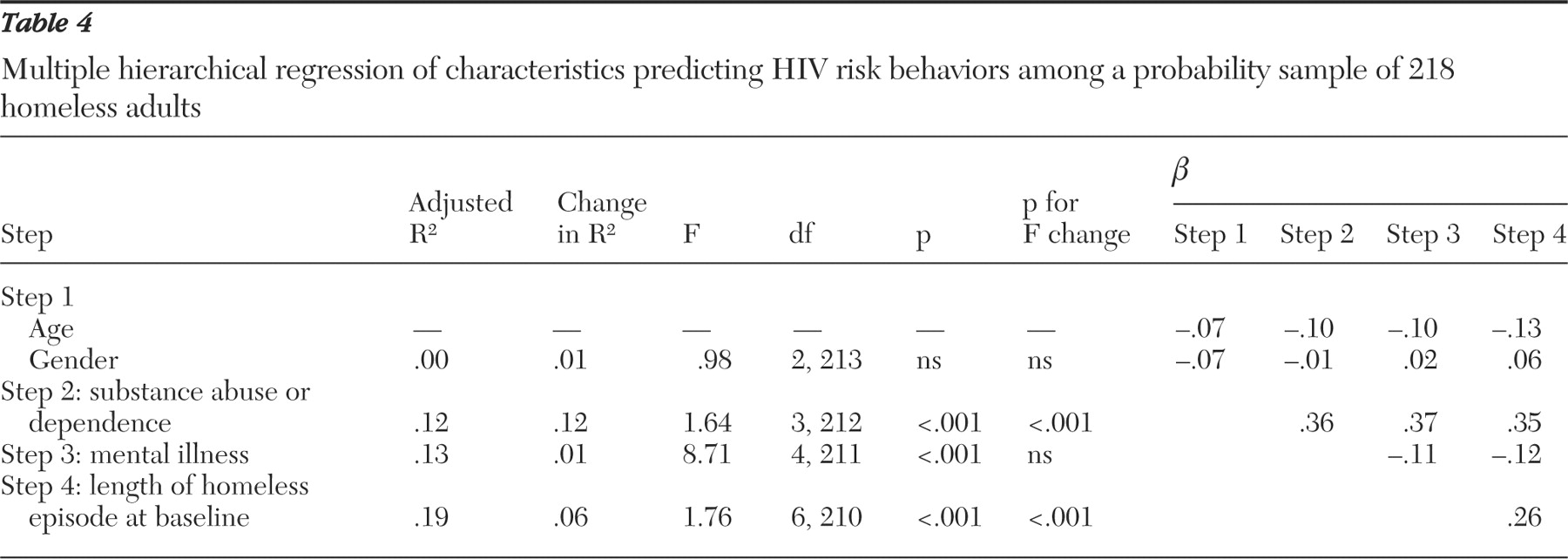
As shown in
Table 4, a hierarchical multiple regression analysis was performed with HIV risk scores as the dependent variable and substance abuse and dependence diagnosis, mental illness diagnosis, and length of homelessness episode at baseline as predictor variables. The total sample was included in the regression analyses, with gender included as a predictor. In step 1, demographic characteristics of age and gender were entered simultaneously. This step did not produce a significant change in R
2 . In step 2, substance abuse was entered and was found to be a significant predictor of HIV risk behavior. Mental illness, entered in step 3, was not significant. Finally, step 4 revealed that the length of homelessness episode at baseline was significant after all variables were entered. With all independent variables in the equation, the model accounted for 21% of the variance with substance abuse or dependence and length of homelessness significantly predicting HIV risk. Changing the order of entry of the variables (after entry of demographic variables) did not change the fact that substance abuse or dependence accounted for a unique portion of the variance. Neither psychiatric disorders nor the interaction of mental illness and substance abuse or dependence disorders were significant in the regression analyses.
Discussion
In this study we used a structured clinical interview to assess the associations between substance abuse and dependence, mental illness, and HIV risk behaviors among a probability sample of homeless adults. A lifetime diagnosis of substance abuse or dependence and a longer episode of homelessness at baseline were associated with HIV risk behaviors.
The relationship between substance abuse or dependence and HIV risk behaviors is consistent with findings from other homeless samples. Substance use disorders are associated with an increased risk of contracting HIV because of unsafe drug practices related to drug injection, the failure to implement risk-reduction strategies because of impaired judgment, and barriers to obtaining condoms (
37 ). Although the association between prolonged episodes of homelessness and HIV risk behaviors has some support in the literature (
14 ), more research is needed to clarify the role of mediating factors, such as depression, stress, and victimization.
Our results did not support previous findings suggesting that homeless adults with a mental illness are more likely to engage in HIV risk behaviors (
38 ). The use of a structured clinical interview instead of self-reports may have contributed to the differences in findings. In addition, the high prevalence of comorbid mental illness and substance abuse or dependence among participants with mental illness (75% of the people with mental illness in our sample) suggests that mental illness may be a potential confound.
Findings of this study reinforce the development of policies focusing on effective HIV risk-reduction strategies among substance-using homeless adults. First, there is a need to combine effective HIV-AIDS prevention programs among homeless adults who present with substance use disorders. Our findings indicate that those who engage in high-risk sexual behaviors are more likely to report a perceived need for substance abuse treatment. Yet a majority of substance abuse treatment programs do not provide HIV risk-reduction services (
39 ). Second, the fact that 63% of participants were sexually active and engaged in sexual behaviors that could place them at risk for contracting HIV-AIDS suggests that soup kitchens and shelters could be prime locations for primary preventive interventions (
9 ). Third, because HIV infection occurs through high-risk behaviors, it is important to design interventions for modifying behaviors and attitudes associated with the spread of HIV-AIDS (
40,
41,
42 ). Among homeless adults, several interventions aimed at increasing knowledge about HIV-AIDS have demonstrated effectiveness and long-term gains (
43 ). However, the most effective interventions are likely to target not only knowledge but also attitudes and behavior skills (
41 ).
There are several limitations to this study. First, our conclusions are limited by the correlational nature of the data. Second, data reported in this study came from a sample of predominantly male homeless adults using shelters and soup kitchens in a specific urban community. Thus results may not speak to infrequent service users and women, although we do not believe this to be a serious limitation because most homeless adults in this particular urban area are men who utilize services discussed in this study. However, these results may not generalize to other locales. Third, we relied solely on self-reports, thus introducing a potential memory bias and a problem associated with the fact that some respondents may be uncomfortable reporting HIV-related behaviors. Fourth, this study did not focus on factors that might mediate the complex relationship between mental illness, substance abuse, and HIV-related behaviors (such as a history of domestic violence or child abuse). Fifth, the findings in this study may have been more robust if rates of psychiatric disorders at the time of study as opposed to lifetime rates were obtained. Sixth, the fact that we summed HIV risk behaviors to derive a score and did not weigh each item in terms of a risk of HIV seropositivity is a limitation that may have decreased the robustness of our findings.
Conclusions
Homeless men and women have been hit hard by the HIV-AIDS epidemic. This study demonstrates that those who are homeless for extended periods, as well as those who have substance use disorders, are at an elevated risk of contracting HIV-AIDS. Furthermore, our findings reveal that homeless adults who engage in high-risk sexual behaviors are likely to report a need for substance abuse treatment. These findings suggest a need to assist homeless people with substance use problems in obtaining treatment, to integrate effective HIV risk-reduction interventions into these treatment programs, and to help these individuals find stable, long-term housing.
Acknowledgments and disclosures
Funding for this research came from the city of Detroit, Wayne County, and the Homeless Action Network of Detroit. The authors thank Michael Bekheet, Amey Dallas, Marilyn Goldstein, Yakiem Israel, Delma Kemp, Nicole Ouelette, Lauren Rowland, Karen Hobden, Heather Janisse, and others associated with our research group who assisted with data collection and analysis. In addition, the authors thank Sheryl Pimlott-Kubiak, Kathleen Wyszacki, and Robert Sprecher for reviewing this manuscript and providing invaluable feedback. They also thank the many homeless individuals and the agencies that serve them in Detroit and Wayne County for participating in this research.
The authors report no competing interests.