The mental health needs of youths in juvenile justice systems have recently become a focus of considerable concern (
1,
2,
3,
4 ). It has been estimated that of the roughly two million youths under age 18 who come into contact with juvenile justice systems each year, nearly two-thirds have either symptoms of or risk factors for serious mental health problems (
2,
3,
5 ). This is consistent with results of studies following youths with serious mental health conditions through adolescence that have found high rates of arrest and trouble with the law (
6,
7,
8,
9,
10 ). Recognition of the potential consequences of not addressing mental health issues has led to a growing consensus that youths entering juvenile justice facilities should be screened for symptoms of mental illness and substance abuse (
11,
12 ). However, prevention of arrest has not been a major focus of adolescent mental health systems.
Arrest rates in the general population are high during adolescence and young adulthood (
13,
14,
15,
16 ). However, rates among youths with mental disorders are markedly higher than among youths in the general population or youths with disabilities not related to mental health conditions (
6,
7,
17 ), even after analyses have controlled for socioeconomic status (
6 ). Taken together these studies suggest that during adolescence and early adulthood, youths with psychiatric disorders are at even greater risk than their contemporaries of involvement in the juvenile or criminal justice system (referred to in this article as "the justice system").
Interventions for limiting involvement in the justice system among youths with serious mental health conditions are critical. Crafting such interventions, however, requires more detailed knowledge than is currently available regarding who is at risk and at what ages risk is highest. Previous studies that have focused on youths receiving child mental health services in the public sector or on special education students with emotional disturbance have laid a foundation for these efforts by examining prevalence of justice system involvement, types of charges, and correlates of involvement (
6,
18,
19,
20,
21 ; Brown E, Greenbaum P, unpublished manuscript, 1994). These studies have not provided sufficiently detailed findings for targeted prevention or reduction efforts. Among the important next steps in this line of research, therefore, is refinement of the empirical knowledge base regarding justice system involvement of youths who use mental health services.
A logical starting point for this effort is determining the risk of offending among youths in mental health systems across the developmental course and by gender. Indeed, criminological research has consistently found substantial gender differences in rates and patterns of offending (
22,
23,
24,
25 ). A number of criminologic risk factors differentiate males and females. For example, victimization histories are more prevalent among female offenders than among male offenders (
16,
26,
27 ). Females may require more aversive experience than males before engaging in antisocial behavior (
24,
28 ). Social control and social learning mechanisms in antisocial behavior are different for males and females (
29,
30,
31 ). Incarcerated juvenile girls are almost 1.5 times more likely than boys to have a non-conduct-related psychiatric disorder with impairment—the reported prevalence among incarcerated juvenile girls is 68% (
32 ). These findings suggest that gender is likely to affect most dimensions of justice system involvement and thus argue for different prevention and treatment strategies.
Previous studies of youthful offenders have sought to determine the ages in boys' and girls' developmental trajectories that interventions should occur, but such studies have not been conducted among youths receiving mental health services. Gender appears to play a role here as well. There is evidence among general offenders that girls' offending begins later than boys' but may persist longer (
33,
34,
35 ). Gender differences in patterns of offending over time also appear to exist; there is a greater variety of patterns among males, and each pattern has its own characteristic ages of onset and desistance (
36 ).
Using statewide administrative databases, we examined involvement in the justice system of individuals between ages seven and 24 who were users of public mental health services for adolescents. The study's principal objective was to gain knowledge about the effects of age and gender on risk of arrest in this population during adolescence and young adulthood in order to support practice and policy reform. The findings may provide insight into the question of when it is best to intervene in a population of intensive users of adolescent mental health services so as to minimize offending.
Methods
Sample
Participants consisted of a statewide cohort of 1,519 youths born between 1976 and 1979 who received adolescent case management services from the Massachusetts Department of Mental Health (DMH) sometime during 1994–1996. The cohort consisted of 781 males (51%) and 738 females (49%). According to the database, 1,111 participants (74%) were white, 126 (8%) were African American, 115 (8%) were Hispanic, 71 (5%) were identified as "other," and 86 (6%) were identified as "unknown." No gender differences in race-ethnicity were found. Race-ethnicity was not further analyzed.
In 1994–1995 eligibility criteria for child DMH services included being under age 19 and having a diagnosable psychiatric condition with functional impairment in two or more domains lasting (or expected to last) at least a year. However, in 1996 DMH standardized its criteria further to define functional impairment as having a score of 80 or higher on the Child and Adolescent Functional Assessment Scale (
37 ).
Data sources
The DMH administrative database contains information on individuals' mental health service use, psychiatric diagnosis, health insurance coverage, and sociodemographic characteristics. The DMH cohort was constructed by extracting data for persons in the DMH database who were born between 1976 and 1979. From that group, data were extracted for those who had received a DMH adolescent case management service between 1994 and 1996. A total of 1,519 participants met these inclusion criteria. Age at which DMH services were initiated was not recorded in the DMH database. Therefore, individuals who received case management services at the time sampled may have also received services at other times.
Arrest data were obtained in July 2005 from the state's Criminal History Systems Board and Department of Probation, which manage the Criminal Offender Record Information (CORI) for criminal and juvenile courts, respectively. CORI data include arrestees' birth year and gender and information about their juvenile and adult arraignment histories in all nonfederal courts in Massachusetts. Each arraignment record contains the charge, court, date of arraignment, and final disposition. Cross-matching between the CORI and DMH data was accomplished by using a specially created unique identifier. We included in our analyses all arrests that occurred before participants' 25th birthday.
Approval for human subjects research
This study was approved by a medical school institutional review board and by the DMH Central Office Research Review Committee. The project was also reviewed and approved by the Massachusetts Criminal History Systems Board, a division of the Massachusetts Trial Court that oversees access to criminal CORI data, and the Massachusetts Office of Probation, which oversees access to juvenile CORI data.
Analysis
Our analyses entailed between-gender comparisons of arrest patterns within age groups, which were performed with SPSS version 14.0.1 and SAS version 9. Arrest rates were calculated by age and gender, and cumulative arrest rates and age at first arrest were calculated for all youths. In addition, arrest risk was calculated by dividing the number of youths arrested by the number of youths at risk for two groups within gender—those never before arrested and those arrested in the previous year of age ("previous year"). Relative risk, which compared the risk of arrest among those never before arrested and the risk among those arrested in the previous year, was calculated. Pearson chi square tests were used to compare arrest rates in independent groups, and t tests were used to test independent means. The McNemar test was used to examine age effects on arrest rates within gender (paired comparisons). The Breslow-Day test, which tests the null hypothesis of homogeneous odds ratio, was used to test gender differences in odds ratios.
Results
Arrest onset
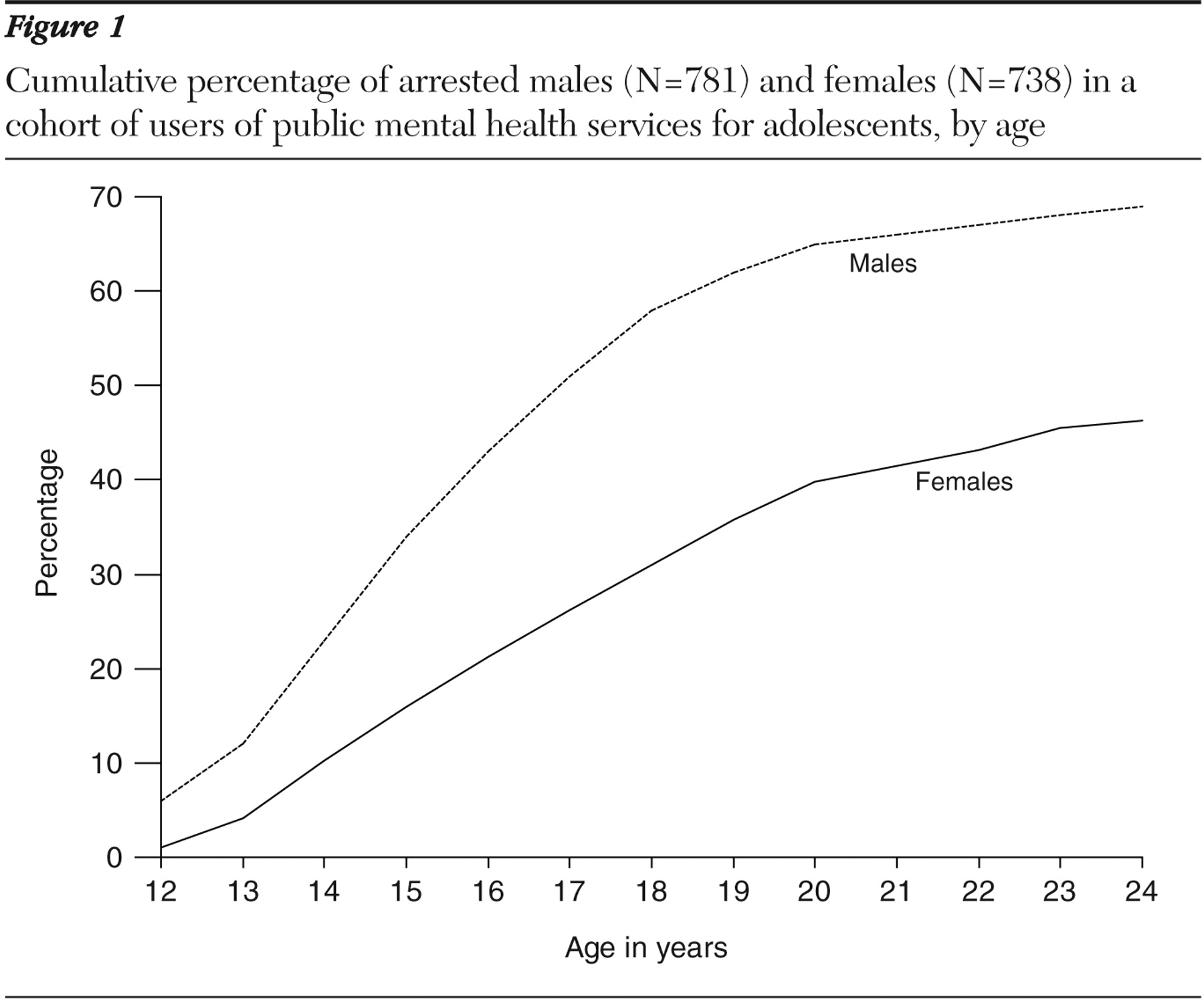
Overall, 870 (58%) of the 1,519 participants had at least one arrest by age 25. The rate was significantly higher among males than among females (533, or 69%, compared with 337, or 46%; χ 2 =79.13, df=1, p<.001). Among those arrested, males were younger than females at first arrest; the mean±SD difference in age at first arrest was 1.31±.20 years (95% confidence interval [CI]=.93–1.71; t=6.65, df=878, p<.001).
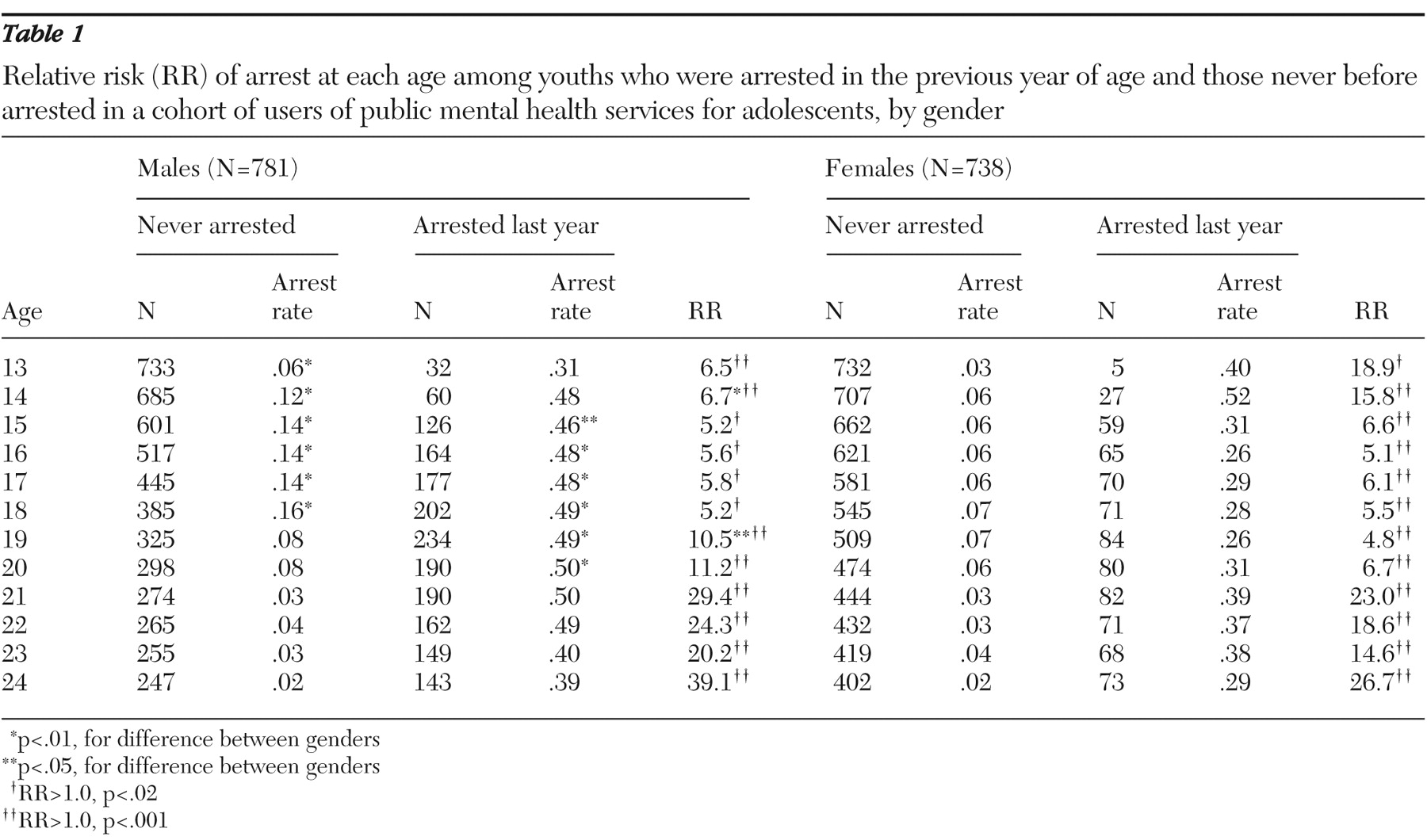
Data in
Table 1 indicate the risk of first arrest at each age. The numbers of males and females at each age who were never arrested and who were arrested in the previous year are shown. Arrest rates among those never arrested were higher for males than for females from ages 13 to 18 (p<.009) but were not significantly different from ages 19 to 24. Within gender, data on age at first arrest during the ages that adolescent mental health services typically cover (13 to 17 years) (
38 ) revealed that few arrestees experienced a first arrest before age 13 (48 males, or 9%, and six females, or 2%). A total of 342 male arrestees (65%) and 187 female arrestees (55%) had first arrests at ages 13 to 17, and 142 male arrestees (26%) and 149 female arrestees (44%) had first arrests at ages 18 to 24.
Figure 1 shows the cumulative proportion of arrested males and females. A total of 390 males (51%) and 193 females (26%) were arrested before age 18; 142 males (18%) and 149 females (20%) experienced a first arrest after age 17.
Arrest rate
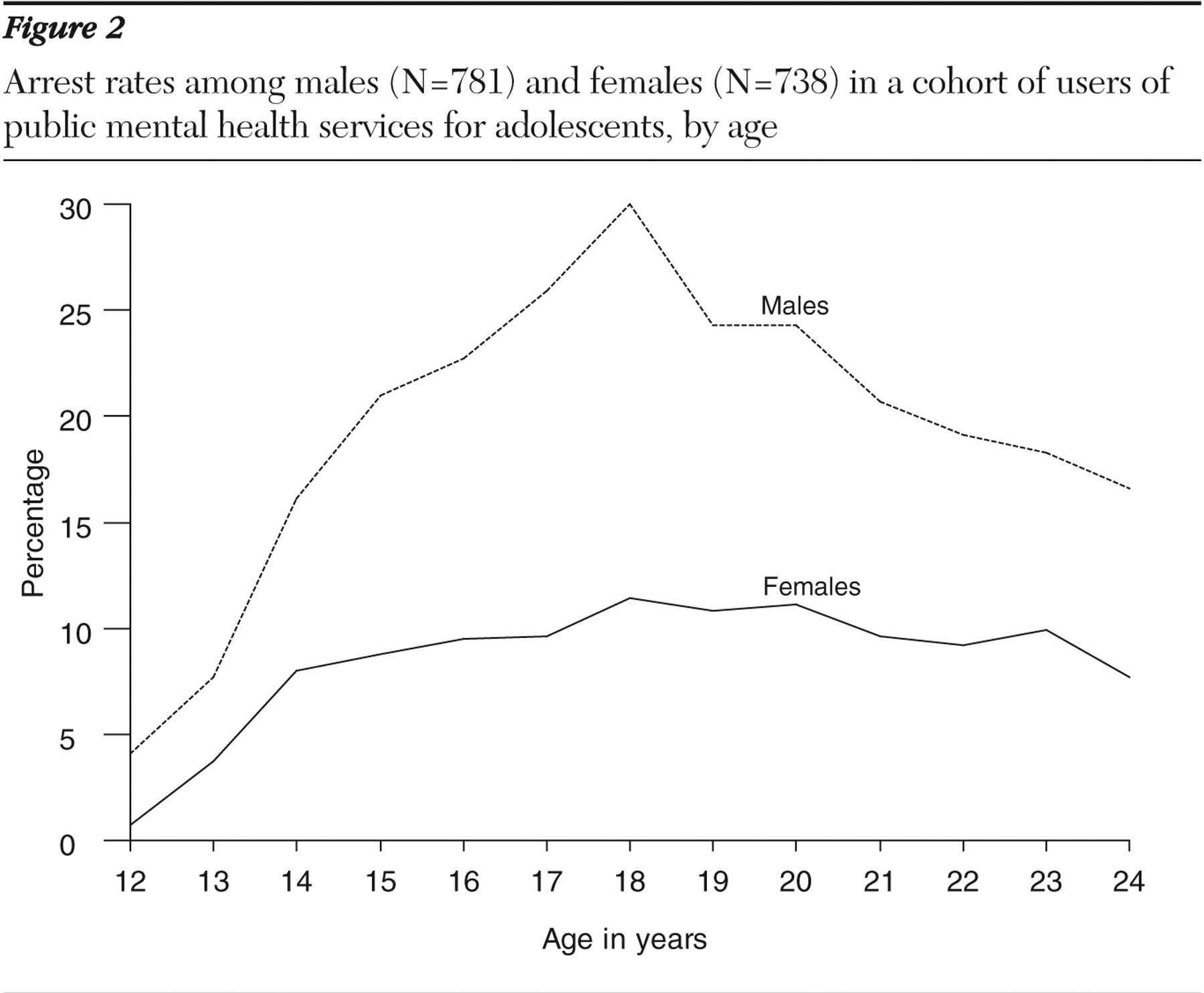
As shown in
Figure 2, the proportion of males arrested at each age was significantly higher than the proportion of females (p<.001). No significant age effects on female arrest rates were found between the ages of 16 and 23. Male arrest rates peaked at age 18, with a higher arrest rate than for males at every other age (p<.05; p<.005 for all ages except 17, p=.044 for 17). Many youths were arrested multiple times—449 males (58%) and 222 females (30%). Many were arrested as adults, that is, at age 18 and older (445 males, or 57%, and 269 females, or 36%). Among those with adult arrests, 303 males (68%) and 120 females (45%) had their first arrest under age 18. Generally, crimes committed at age 17 and older are tried in criminal court; juvenile courts try offenses of individuals under age 17, with the exception of specific charges that are tried in criminal court largely regardless of age.
Risk of arrest
Table 1 also shows the number of males and females at each age who were arrested in the previous year and the arrest rate among them. At every age and for both genders, the relative risk of arrest was significantly higher among those arrested the previous year than among those with no previous arrests. The highest rates were for males aged 14 to 22 whose arrest rates among those arrested in the previous year hovered around 50%. For youths between the ages of 15 and 20 arrest rates were significantly higher among males arrested in the previous year than among females (p<.05), but rates did not differ significantly otherwise (
Table 1 ). Gender differences in relative risk for those arrested in the previous year compared with those never arrested were significant for youths aged 14 years (Breslow-Day
χ 2 =111.60, df=1, p<.001) and 19 years (Breslow-Day
χ 2 =4.23, df=1, p=.04) but not for those of other ages. Fifty percent (N=3,481) of all male charges made between ages 13 and 24 occurred among those arrested the previous year, whereas only 22% (N=1,503) were among first time arrestees. Among females these figures were 37% (N=764) and 34% (N=713), respectively.
Discussion and conclusions
As noted in our introduction, current research on mental heath issues in juvenile justice populations has tended to begin with youths involved in the justice system, focusing on the prevalence of psychiatric symptoms and risk factors among youths encountered in juvenile justice settings (
1,
2,
12 ). The study reported here took the opposite perspective, looking at involvement in the juvenile and criminal justice systems of youths served in the public mental health system. Both perspectives offer essential and complementary data on mental health issues in populations involved with the justice system and on risk factors for such involvement among recipients of public mental health services.
Limitations
Before we consider this study's specific implications for mental health service delivery, we must acknowledge the limitations that this perspective imposes on the generalizability of our findings. The eligibility criteria for receiving Massachusetts DMH services—and the inclusion criteria for our sample—constitute a high threshold for clinical and functional severity. Many youths with significant psychiatric disorders would fail to meet this threshold. Many who do meet it may be treated in the private sector or in public services other than the child mental health system. Our study did not capture data on these youths and on the majority of youths with serious mental health conditions who receive no services (
39 ).
Although we cannot generalize our findings to these populations, we nonetheless feel that our data on DMH clientele are valuable. First, eligibility criteria for Massachusetts' DMH services are similar to those in other states, so these findings are likely generalizable to adolescents served in state mental health systems across the country. Administrators of these agencies need to work with the juvenile and criminal justice systems in their locales to develop interventions that are beneficial for those with significant needs for mental health treatment. Indeed, the public mental health system may be one of the destinations for many youths with disorders identified in juvenile justice settings, and these individuals will become part of the population for which administrators need to plan. Findings for this population thus can help refine related questions for other populations.
Any study reporting on crime in a population with mental health conditions should be interpreted with caution so that it will be reasonably informative without needlessly adding to stigma. The arrest rates by age 25 reported here appear to be high. However, we did not compare these rates with those for persons of the same age in the general population, nor have we yet described the types of charges involved in these arrests. Arrest rates and charging patterns vary across time and geographic location, and thus any comparison needs to be carefully informed by a well-chosen, local, contemporary comparison group. For this reason, and for reasons of generalizability described above, these findings should not be interpreted to mean that adolescents with serious mental health conditions are more violent than their peers.
This study was also unable to identify in which system youths were first involved or pathways traveled between DMH and justice systems. Although the justice records captured data on lifelong juvenile or criminal court appearances in Massachusetts, the DMH database recorded receipt of services only for the years the database existed, which for these youths was limited to adolescence and older. It did not include dates of first DMH involvement. It is important to note that for some youths justice system involvement may have been the door through which DMH services were accessed. Another limitation of this study is that arrest rates were not corrected for exposure time; specifically, our arrest rates underestimated arrest risk because individuals who were incarcerated or hospitalized, with little risk of arrest during those times, are included in the risk pool. With these caveats in mind, we turn to the discussion of our findings.
Implications
The findings presented more than justify current concerns of public mental health systems regarding involvement of their adolescent clienteles in the juvenile and criminal justice systems. The study also identified demographic markers for intensified intervention efforts. As in the general population, involvement of males in the justice system was greater than that of females; proportionately more males were arrested at each age and by age 25. However, almost half the sample of female adolescents receiving public mental health services had an arrest by age 25, and most of these had one by age 18. Thus justice system involvement of males and females in the adolescent public mental health population is concerning. Indeed, our findings mirror those of research on gender difference in arrest among adults with severe mental illness. Data from a number of studies indicate that differences between males and females who are at risk of arrest are not as pronounced as in the general population, suggesting that the "protective effect "of female gender is not as robust in terms of arrest as it is in the general adult population (
8,
19,
40 ).
Because many youths in the study began offending after midadolescence and into adulthood, and many reoffended at those ages, our findings suggest that both child and adult mental health services have an opportunity to prevent first arrests among those not yet arrested and to reduce further offending among those with a history of arrest, regardless of the system, justice or mental health, with which youths are first involved. However, no more than 16% of the never-arrested population for each gender experienced a first arrest in any given year. Therefore, primary prevention efforts either need to be sufficiently inexpensive and nonaversive to be applicable to the whole group or need to be guided by future research in order to target the preventive intervention to those at greatest risk. Such research will need to determine risk markers for each gender and age.
Our findings further suggest that interventions to reduce recidivism could be more precisely targeted in this population by identifying youths arrested in the previous year. Such information should be relatively easy to obtain. Those arrested in the previous year are about five to 40 times as likely to be arrested as those who have never been arrested. In fact, if recidivism reduction were completely effective for one year, targeting those arrested the previous year would eliminate half of all arrests among males and more than a third of arrests among females and could have the added benefit of helping youths desist from offending at an early age.
These findings also suggest that ages 16 to 22—the ages when youths transition from adolescence to adulthood and from child to adult systems—are particularly fraught with risk of arrest for males and include some of the highest arrest rates for females. Other studies have identified this transition period as a time when youths in mental health systems "age out" of eligibility for adolescent mental health services and other support and do not necessarily gain access to compensatory services (
39,
41,
42 ). Little is known about the ability of mental health services to reduce or prevent offending or about the impact of loss of needed services. This, too, is an area for future research.
Finally, our data confirm gender as an important consideration in questions of justice system involvement among intensive users of public mental health services but illustrate that it is not always a critical factor. Specifically, gender did not play a role in the risk of first arrest after age 18, in the risk of arrest in those arrested the previous year among those under 15 or over 20, or, at most ages, in the increased risk of arrest among those arrested the previous year compared with those never arrested. These findings suggest that males and females in this population share many risk factors for arrest and recidivism, which will be important questions for future research.
In considering gender differences we need to be cognizant that, as with race and to some extent age, gender is in many ways a marker for a host of lifestyle, behavioral, and societal reaction factors. Better understanding of what these factors are and whether they are mutable through system intervention is one of the next steps in designing strategies for reducing the risk of justice involvement among youths with serious emotional disorders.
Acknowledgments and Disclosures
This research was supported by grant R01-MH-067862-01A1 from the National Institute of Mental Health to Dr. Davis. The authors thank David Huizinga, Ph.D., Nancy Koroloff, Ph.D., Krista Kutash, Ph.D., Edward Mulvey, Ph.D., and Ann Vander Stoep, Ph.D., for helpful comments. They also thank Fred Altaffer, Ph.D., and Thomas Athearn at the Massachusetts Department of Mental Health and the research staff at the Criminal Offender Record Information and the Office of Probation for their assistance in accessing these databases.
The authors report no competing interests.