Diabetes is the seventh leading cause of death in the United States, as documented on over 8% of the country's death certificates, or about 200,000 deaths annually (
1 ). An additional 200,000 people with diabetes die each year of causes other than diabetes (
1 ). While the mortality rate in the United States has declined for the general population in the past 30 years, death rates have increased by as much as 45% for people with diabetes during this same period (
2 ).
That persons with diabetes die younger is not surprising; diabetes can lead to serious long-term complications, which in turn can lead to life-threatening conditions. Even within the population of individuals with cardiovascular disease, people with diabetes are two to four times more likely to die from cardiovascular problems (
1 ), and diabetes is a significant predictor of mortality among people with chronic heart failure (
3 ). Similarly, among people with hepatitis, poor glycemic control of diabetes significantly increases the likelihood of death (
4 ).
Compared with the general population, people with psychotic disorders, like those with diabetes, also die at significantly younger ages (
5 )—likely a result of an increased risk of serious medical conditions. For example, individuals with psychotic disorders are about twice as likely as the general population to have type 2 diabetes (10%-15% versus 6%) (
6 ), about 1.5 times more likely to have coronary heart disease (
7 ), eight times more likely to be infected with HIV (
8 ), five times more likely to be infected with hepatitis B (
8 ), and 11 times more likely to be infected with hepatitis C (
8 ).
The purpose of the study reported here was to examine the impact of diabetes on mortality—above and beyond the contribution of age, gender, and race and ethnicity—among individuals with co-occurring psychotic and substance use disorders who participated in a randomized controlled study of integrated mental health and substance abuse treatment.
Methods
The Connecticut Dual Diagnosis Study was a longitudinal, randomized controlled study comparing assertive community treatment and standard case management for individuals with co-occurring psychotic and substance use disorders who were receiving integrated mental health and substance abuse treatment (
9 ). The protocol was approved by the institutional review boards of the Connecticut Department of Mental Health and Addiction Services, the Southwest Connecticut Mental Health System, Dartmouth College, and the University of Connecticut. Study sites included two community mental health centers in urban areas of Connecticut with a large population of residents below the poverty line.
Study participants were enrolled between August 1993 and July 1998 and followed for up to 12 years; deaths were confirmed by medical record review and the Social Security Death Index (ssdi.genealogy.rootsweb.com). All study participants had a major psychotic disorder (such as schizophrenia or bipolar disorder) and active substance abuse at study entry. The sample was predominantly male (N=140 men, or 71% of the sample), young (mean±SD=36.8±7.9 years), and from minority backgrounds (114 African American, or 58%, and 30 Hispanic, or 15%). The demographic characteristics reported here differ slightly from a previous report (
9 ) because further information about some study participants allowed us separate variables for ethnicity and race.
We obtained Medicaid reimbursement data for 197 of 199 study participants from the period ranging from one year before through up to seven years after study entry. Study participants were coded as having evidence of diabetes if they had at least one reimbursement for a diabetic drug or device or at least one reimbursement for a service for which diabetes was the diagnosis. Using survival analyses, we examined whether the time from study entry until death was different for individuals with and without evidence of diabetes. Using a Cox regression model with demographic information entered first (age, gender, whether race was African American, and whether ethnicity was Hispanic) and evidence of diabetes entered second, we explored the impact of diabetes on death above and beyond demographic variables.
Results
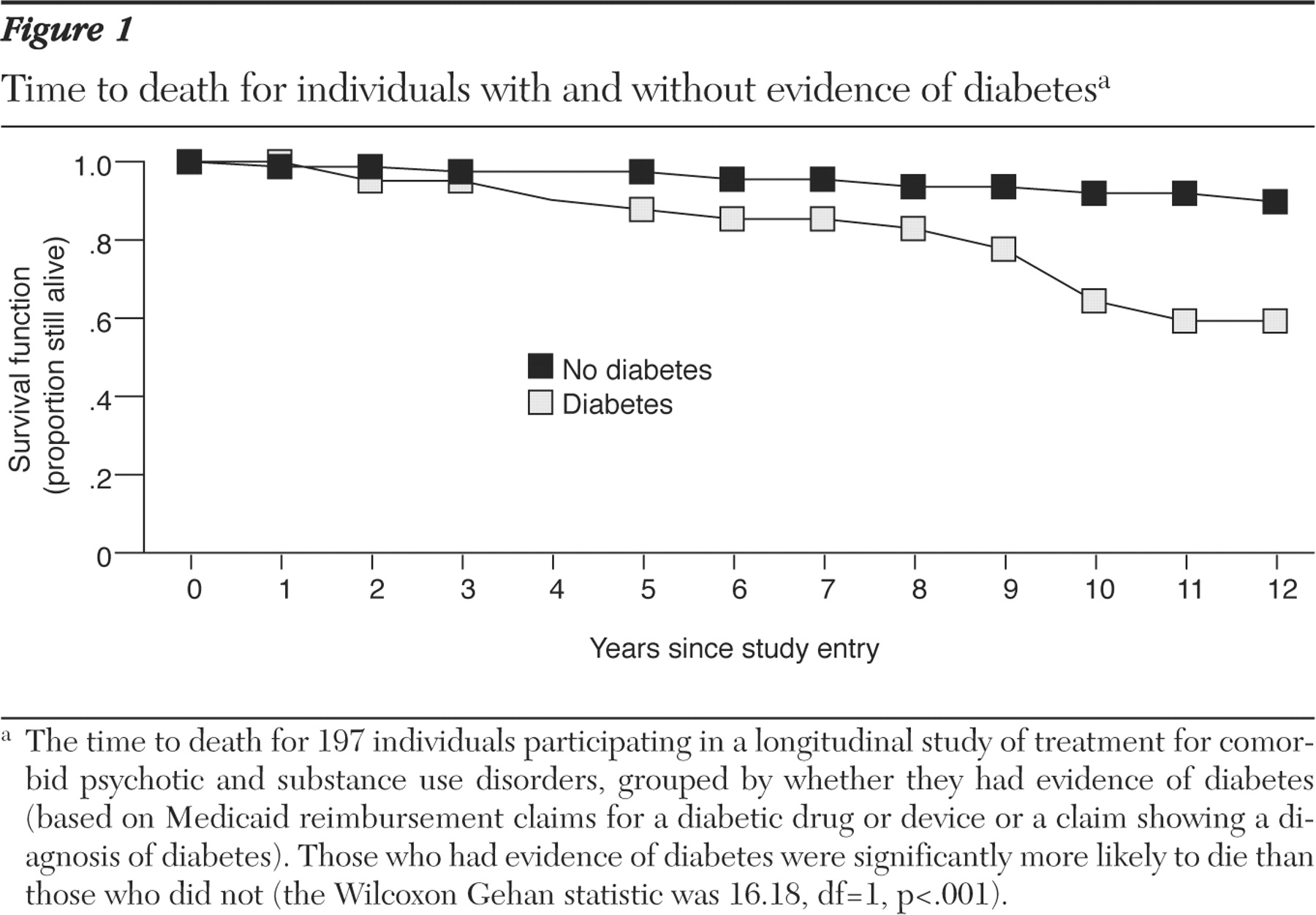
Of the 197 individuals with Medicaid information available, 41 (21%) had evidence of diabetes. People with evidence of diabetes were significantly more likely to die during the study period than those without evidence of diabetes (Wilcoxon Gehan statistic of 16.18, df=1, p<.001) (
Figure 1 ). By the tenth year in the study, 13 (36%) of those with evidence of diabetes had died compared with only 12 (8%) of those without evidence of diabetes. After ten years, data were available for only 16 individuals with and 96 individuals without evidence of diabetes, during which time one person from each group died.
Participants with diabetes were significantly more likely to be Hispanic ( χ 2 =5.40, df=1, p<.05). Eleven (37%) of 30 Hispanic participants compared with 30 (18%) of 167 non-Hispanic participants had evidence of diabetes. Participants with diabetes were also marginally older than participants without diabetes (p=.06). The mean age was 38.8±8.1 years at study entry for those with evidence of diabetes and 36.2±7.7 years for those without evidence of diabetes. Ethnicity and age were not related, and there were no racial or gender differences between those with and without diabetes. In the Cox regression model, evidence of diabetes significantly predicted time to death above and beyond the demographic characteristics (Wald χ 2 = 15.03, df=1, p<.001); age was also significantly related to death in the final model (Wald χ 2 =5.11, df=1, p<.05).
Discussion
Similar to the general population, people with co-occurring psychotic and substance use disorders have a significantly greater likelihood of premature death if they also have diabetes. In a 12-year period, death rates for individuals with evidence of diabetes exceeded 40%, compared with 10% for those without evidence of diabetes. In addition, whereas rates of diabetes among those with serious mental illnesses range from 10% to 15% (
6 ), 21% of individuals with co-occurring psychotic and substance use disorders in this study had evidence of diabetes.
Others have indicated the need for diabetes prevention and care among persons with serious mental illness (
10 ), and this need may be even greater for those with comorbid substance use disorders. People with co-occurring serious mental illness and substance use typically have low treatment adherence rates (
11 ), which may increase the likelihood that health symptoms will remain undiagnosed and untreated. Substance abuse also likely complicates the management and course of diabetes, increasing the risk of death from diabetes complications. Also, individuals with co-occurring serious mental illness and substance abuse appear to be at increased risk of several serious medical illnesses in addition to diabetes. For example, among individuals with serious mental illness, substance use tripled the likelihood of HIV infection and roughly doubled the rates of hepatitis B and C (
8 ). Given these findings, mental health providers should consider providing diabetes education and interventions within the mental health setting to manage weight gain. Some promising interventions among persons with schizophrenia and diabetes include behavioral modification for weight loss (
12 ) and participation in diabetes education groups to reinforce concrete behavior change (
13 ).
Given the relatively small number of deaths from any cause reported in this study of persons with co-occurring psychotic and substance use disorders, these results should be interpreted cautiously. In addition, the use of administrative data likely underestimated the number of individuals with diabetes, for two reasons. First, because we followed individuals for up to 12 years and claims were available for only seven years, individuals who developed diabetes after seven years would have been incorrectly categorized as not having evidence of diabetes.
Second, many individuals have undiagnosed diabetes (
1 ) and thus would not have claims representing diabetes treatment. However, one of the strengths of this study was that we were able to confirm the death status of each study participant for at least eight years and up to 12 years beyond study entry by accessing public records. We did not have access to information on medications prescribed throughout the follow-up period. Given that some antipsychotic medications can exacerbate metabolic conditions (
10 ), it is possible that some diagnoses of diabetes and some deaths were related to the antipsychotic medications prescribed. Because diabetes may be preceded by metabolic syndrome and is associated with cardiovascular disease and obesity, each of which may also increase the likelihood of mortality, future studies including larger sample sizes of persons with co-occurring substance use and serious mental illness should include measures of weight, metabolic syndrome, cardiovascular disease, and diabetes to identify the unique and interactive contributions of these factors to mortality in this population.
Conclusions
Diabetes may significantly increase the likelihood of premature death among people with co-occurring psychotic and substance use disorders (41% for those with evidence of diabetes compared with 10% for those without evidence of diabetes by the end of 12 years). Interventions targeted for diabetes prevention and management are critical for persons with serious mental illness, particularly among the subset who also abuse substances.
Acknowledgments and disclosures
This work was supported by U.S. Public Health Service grants R01-MH-52872 and R01-MH-63463 from the National Institute of Mental Health; R01-AA-10265 from the National Institutes on Alcohol Abuse and Alcoholism; and UD3-SM51560, UD3-SM51802, and UD9-MH51958 from the Substance Abuse and Mental Health Services Administration.
Dr. Drake reports receiving funding from Johnson & Johnson. The other authors report no competing interests.