Complementary alternative medicine enjoys wide use in this country (
1,
2 ), particularly among U.S. ethnic minority populations. Complementary alternative medicine has been used to treat cancer (
3 ), HIV (
4 ), and other health conditions (
5 ). Remarkably few data are available on complementary alternative medicine use among patients with mental health disorders, especially among Asian Americans, who not only heavily rely on traditional treatments (
5 ) but also increasingly present with mental health symptoms (
6 ).
This study used a cross-sectional survey to determine the prevalence and sociocultural correlates of complementary alternative medicine use in an urban sample of Chinese-American patients seen at mental health service units of community health centers.
Methods
The study sample consisted of 153 Chinese-American patients seen in the mental health service units of three community health centers in New York City that were located in predominantly Chinese neighborhoods in Manhattan and Queens. Eligible patients were Chinese (through self-report); were aged 18 years or older; could speak and understand Cantonese, Mandarin, or English; and presented with at least one DSM-IV diagnosis.
Data were obtained through self-administered questionnaires and chart review. Patients' self-reported information included sociodemographic characteristics, such as age, gender, income, employment, education, insurance, physical functioning status, mental functioning status, acculturation, mental health stigma, traditional beliefs in mental health, and use of complementary alternative medicine. Psychiatric diagnosis was extracted from patients' medical charts.
On the Alternative Health/Complementary and Alternative Medicine questionnaire (
5 ), patients indicated their use of 28 complementary alternative therapies during the past 12 months and over their lifetimes. The categories included megavitamins, Chinese herbal medicine, acupuncture, Chinese massage (tui na), massage therapy, spiritual healing, chiropractic therapy, yoga, meditation, hypnosis, energy healing or reiki, folk remedies, chelation therapy, qi gong, macrobiotics, polarity, aromatherapy, naturopathy, tai chi, homeopathy, biofeedback, guided imagery, Ayurveda, and popular dietary approaches (vegetarian, Pritikin, Atkins, Ornish, and the Zone diets).
Physical health functioning and mental health functioning were measured, respectively, by the physical component summary subscale and the mental component summary subscale on the 12-item Medical Outcomes Study Short-Form (
7 ). On both measures, possible scores range from 0 to 100, with higher scores indicating better health status. Acculturation was measured by a 12-item, 5-point Likert scale covering language and media use and social relations (
8 ). Patients also used a 12-item Likert scale to report whether they believed that people in mental health treatment are discriminated against by others (
9 ). Finally, patients were asked to assess the extent to which they believed that traditional forces (for example, supernatural, spiritual, and mystical forces) contribute to mental illness (
10 ).
All instruments were back translated and showed alpha reliability coefficients ranging from .88 to .94. This study was approved by the institutional review board of Columbia University and the medical and dental board of Charles B. Wang Community Health Center in New York City. Patients signed a board-approved informed consent form (in Chinese or English), and they completed the questionnaire in a private treatment room. Measures were administered at each health center from December 2004 to March 2005.
Bivariate analyses examined differences between patients who currently used complementary alternative medicine and those who did not. Chi square tests assessed dichotomous variables, and t tests compared continuous variables. Logistic regression was performed to examine predictors associated with use of complementary alternative medicine. SPSS 12.0 was used for statistical analyses, and p values of .05 or less were considered significant.
Results
The mean±SD age of the 153 study participants was 44.8±16.2 years; 101 (66%) were female. A total of 142 (93%) were born outside the United States, 79 (52%) were married, 87 (57%) were unemployed, and 69 (45%) lacked a high school diploma. Ninety-five (62%) reported an annual household income of less than $20,000. According to DSM-IV diagnoses, 76 (50%) had depressive disorders, 43 (28%) had anxiety disorders, 16 (10%) had psychotic disorders, ten (7%) had bipolar disorders, and eight (5%) had adjustment disorders.
Most patients (144 patients, or 94%) had used complementary alternative medicine, and 126 patients (82%) were currently using alternative therapy to treat medical and mental health problems. The most popular currently used forms were megavitamin therapy (70 patients, or 46%), Chinese herbal medicine (66 patients, or 43%), massage therapy (40 patients, or 26%), acupuncture (38 patients, or 25%), and spiritual healing (36 patients, or 24%).
Compared with patients who did not use complementary alternative medicine during the past year, those who used the treatment were older (t=-5.81, df=151, p<.001) and more likely to be female ( χ 2 =6.80, df=1, p<.01) and employed ( χ 2 =4.09, df=1, p<.05). Compared with current nonusers, current users had poorer physical functioning (t=2.10, df=150, p<.05) and were less acculturated (t=2.07, df=151, p<.05). Alternative treatment use did not differ by education or insurance coverage and was unrelated to patients' reports regarding mental functioning, mental illness stigma, and traditional beliefs.
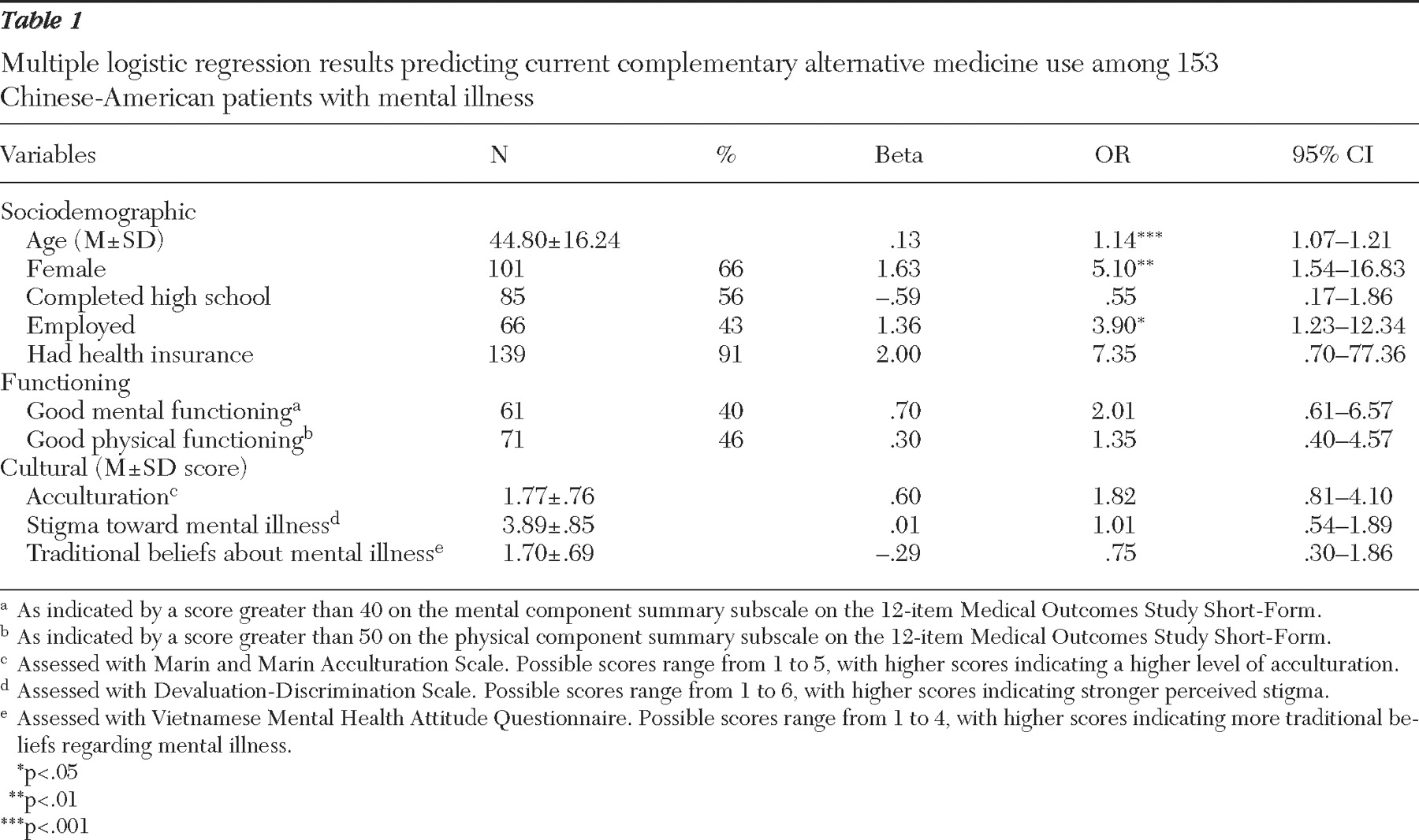
As shown in
Table 1, logistic regression analysis (Wald
χ 2 =53.57, df=10, p<.001) revealed greater current alternative therapy use by older people than by younger people (p<.001), by women than by men (OR=5.10, p<.01), and by employed persons than by unemployed persons (OR=3.90, p<.05). Use of alternative therapy did not differ by physical functioning scores or by acculturation level after the analyses adjusted for demographic, education, employment, and insurance factors.
Discussion
These are the first data on use of complementary alternative medicine in a mental health service sample of Chinese Americans. In this sample, users of complementary alternative medicine were older, female, and employed, similar to national samples of users in America (
1,
5 ). Moreover, users were also functioning less well physically and less acculturated. Types of complementary alternative medicine used by our respondents were expectedly dominated by traditional Chinese regimens, whereas national data reveal a wider repertoire of approaches (
2,
5 ). Unexpectedly, use of complementary alternative medicine in our sample was related neither to mental health symptomatology nor to stigma of mental illness.
Study findings have a number of limitations. Coming from large urban communities of relatively poor immigrants, patients were not representative of all Chinese Americans. Patients were also seen at a mental health service, likely introducing other, albeit unmeasured, biases. Further, the self-report nature of data collection precluded knowing whether patients actually employed the reported complementary alternative therapies, to what extent and fidelity the therapies were applied, and the health or mental health outcomes of complementary alternative medicine applications.
Conclusions
The above limits notwithstanding, this study points toward trends in use of complementary alternative medicine among Chinese Americans with mental health problems and, as such, has implications for responsive diagnostic and treatment efforts. Because most Chinese patients with mental health problems use treatments in addition to conventional mental health services, mental health practitioners who see those patients may wish to proactively probe use of complementary alternative medicine, evaluate its potential impact, and perhaps seek to integrate conventional and unconventional treatments.
Growing ethnic and racial diversity in America calls for new and better studies of patterns and cultural components of and reasons for complementary alternative medicine use. This use is a reality of physical and mental health treatment in the United States, especially among minority groups and new immigrants. By understanding the prevalence of complementary alternative medicine use, exploring its epidemiology and consequences, and determining how it can enhance physical and mental health treatment, public health professionals can better serve their patients and communities.
Acknowledgments and disclosures
The authors thank the patients, staff, and administration of the Charles B. Wang Community Health Center in New York City for making this research possible and the New York Coalition for Asian American Mental Health for supporting the research.
The authors report no competing interests.