Two widespread approaches to the management of acutely aggressive children include the use of mechanical restraints or seclusion. With restraint, leather or Velcro straps are attached from a person's limbs to bed railings, and with seclusion, there is typically locked-door confinement in a padded "safe room." Although such measures can be lifesaving in the context of serious aggressive, violent, or self-injurious behaviors, there is a concerted movement to minimize their use in clinical practice. Toward this goal, legislative measures at the federal level (
1,
2 ) have sought to reduce if not eliminate (
3 ) the use of such restrictive interventions.
There are several lines of reasoning behind such efforts. First, there have been growing concerns about safety, particularly with restraint use, which first received national attention in 1997 after the untimely death of a young patient in Connecticut. A subsequent national investigation by the
Hartford Courant revealed that the deaths of an additional 142 people were related to restrictive intervention (
4 ). Another 45 deaths were documented across the country between 1993 and 2003 (
5 ), and analyses of fatalities identified positional asphyxia as the leading root cause of death (
6,
7 ). Apart from physical injury and medical complications, recurring concerns include the psychological impact of these measures, both on the children (
8 ) and on the nursing staff and other direct care staff involved in the children's care (
9 ). Moreover, there is no clear evidence supporting the efficacy of these interventions (
10 ); for example, a review of 36 published studies concluded that there is insufficient evidence to support an association between patient safety and use of restraint and seclusion in the short-term management of violent behavior in adult psychiatric inpatient care (
11 ). Other critics have called attention to the poor cost-effectiveness of practices that are as inherently intensive in their staffing needs and that detract from the more proactive allocation of precious human resources (
12 ).
Taken together, these data provide a compelling argument to reconceptualize restraint and seclusion as last-resort interventions, if not as outright treatment failures (
3 ). The Joint Commission (
13 ), the American Academy of Child and Adolescent Psychiatry (
14 ), and the Child Welfare League of America (
15 ) have all provided specific guidelines to reduce the use of restraint and seclusion. Common among all three is the recommendation to provide competency-based training for all professionals involved in the application of restrictive interventions. Several staff training programs have been described in the literature (
16,
17,
18,
19,
20,
21 ), all of which focus on the prevention of behavioral escalation to the point that restrictive interventions would become necessary to ensure patient safety. These approaches are more humane and based on patients' strengths in their approach to clinical care, but data are limited on the ability of these approaches to effect change while ensuring patient safety, particularly in the case of children and adolescents.
In this article we describe changes in use of restraint and seclusion in a child psychiatric inpatient setting after the implementation of the collaborative problem-solving (CPS) model of care (
22 ). Although CPS was not designed with the explicit goal of decreasing restrictive interventions, we hypothesized, on the basis of preliminary experience of others (
20 ), that after complete implementation of the model there would be fewer and shorter restraint and seclusion events and no compromise in patient safety.
Methods
Study site and participants
This prospective study was based on data collected at a psychiatric inpatient unit for school-age children that is part of the Yale-New Haven Children's Hospital. The inpatient service has a bed capacity of 15; during the five-year interval of the study, the unit had an average of 198 admissions per year, a bed occupancy of 92%, and a length of stay of 29 days. Approval to review and abstract data was obtained from the institutional review board of Yale University School of Medicine. Clinical information was stripped of all personal identifiers, stored anonymously, and exclusively referenced through study-specific unique identifiers, according to published guidelines (
23 ).
Information was collected for all children hospitalized during fiscal years (FYs) 2003 to 2007 (October 1, 2002, through September 30, 2007). Demographic and clinical variables were abstracted from electronic medical records and included age, sex, race-ethnicity, admission status (via emergency service versus other access points), insurance status (Medicaid versus other forms), length of stay, readmissions within the year (yes versus no), and primary discharge diagnosis. We defined psychiatric diagnoses as
ICD-10 codes between 290.00 and 319.99 and divided these into seven mutually exclusive categories by minor modification of a previously used classification scheme (
24 ): adjustment disorders, anxiety disorders, bipolar disorder, depressive (nonbipolar) disorders, hyperactivity, psychosis, and other mental disorders.
CPS intervention
CPS is a manualized therapeutic program rooted in cognitive-behavioral principles that was initially developed to work on an outpatient basis with children and adolescents with oppositional behaviors and aggressive outbursts (
25 ). CPS has been adapted to the specific needs of an inpatient setting (
20,
22,
26 ). The CPS model conceptualizes aggressive behavior as the by-product of lagging cognitive skills in the domains of flexibility, frustration tolerance, and problem solving. It provides a framework to understand children's aggressive behavior as stemming from impairments in one of five non-mutually exclusive pathways: executive functioning (including inattention, disorganized thinking, and poor handling of transitions), language processing (such as expressive or receptive impairments and difficulty expressing feelings), emotion regulation (including irritability, anxiety, and distorted self-perception), cognitive flexibility (such as concrete thinking and insistence on sameness and rigid routines), and social skills (such as misreading interpersonal nuance and difficulty appreciating the views of others). CPS seeks to identify pertinent social and cognitive pathway impairments and precipitating antecedent events; it models alternative means of de-escalation through social problem-solving, conflict resolution, and anger management strategies. Through these means, CPS seeks to ultimately prevent further aggressive outbursts.
CPS was implemented during a six-month period beginning in September 2005. Staffwide training included an initial three-hour overview lecture of the conceptual model and dissemination of written materials, followed twice weekly by 90-minute videoconference-based supervision sessions with the developers of the CPS model. During these sessions, specific children and their challenging behaviors were discussed in detail in the context of the CPS model. The initial lectures (repeated for different shifts) and the ongoing supervision sessions were scheduled in a way that maximized exposure to the model for all staff members, namely 25 nursing staff, 35 milieu counselors, two child and adolescent psychiatrists, one psychologist, three school personnel, and six trainees in various disciplines. Staff members attended a mode of three supervision sessions per month during the training period (range one to four). Each session was attended by a mode of 12 staff members (range three to 17).
During the implementation phase, a simultaneous process was initiated to revise and update routine clinical chart documentation so that it incorporated the principles of the CPS model (specifically, identification of pathways, triggers, and ensuing interventions) and still covered all administrative, legal, and clinical requirements. This revised chart documentation, together with ongoing weekly group supervision meetings (without the initial videonferencing element), served to maintain the CPS model incorporated into the unit's clinical practices after the active implementation phase was over.
Restraint, seclusion, and injury measures
Data on use of restraint and seclusion were collected in accordance with requirements of the Joint Commission, which were in full operation at the inpatient service as of January 1, 2002. Date, time, and duration were available for all of the restraint and seclusion events during the study period. Data on staff injuries were available for FY 2005 through FY 2007. Incidents on file were those in which a formal report had been made to the hospital's occupational health service.
Data analysis
Categorical and normally distributed continuous variables were respectively compared across years by using the chi square statistic and independent-sample t tests or one-way analysis of variance. The likelihood of a child's restraint or seclusion during his or her hospital stay was explored with multivariate logistic regression analysis. Separate models were run for each outcome. Odds ratios (ORs) and 95% confidence intervals (CIs) are presented to quantify significant associations.
Next, the total number of events and their cumulative duration were summarized for each patient and expressed as total events per year and as monthly averages. To allow for interinstitutional comparisons, summary results were also expressed per 1,000 patient-days, a metric common in national benchmarking surveys. Next, monthly and yearly tallies for restraint, seclusion, and their combined totals were calculated. These totals served as dependent variables for linear regression models, with the 60 months of study as the independent ordinal variable. Slope (beta) and p for trend values were obtained through linear regression, and these values are presented alongside a summary measure (size of change) of the difference in the variable in question between the first and last quarters of the study period. All analyses were conducted with SAS, version 9.1.
Results
Participant characteristics
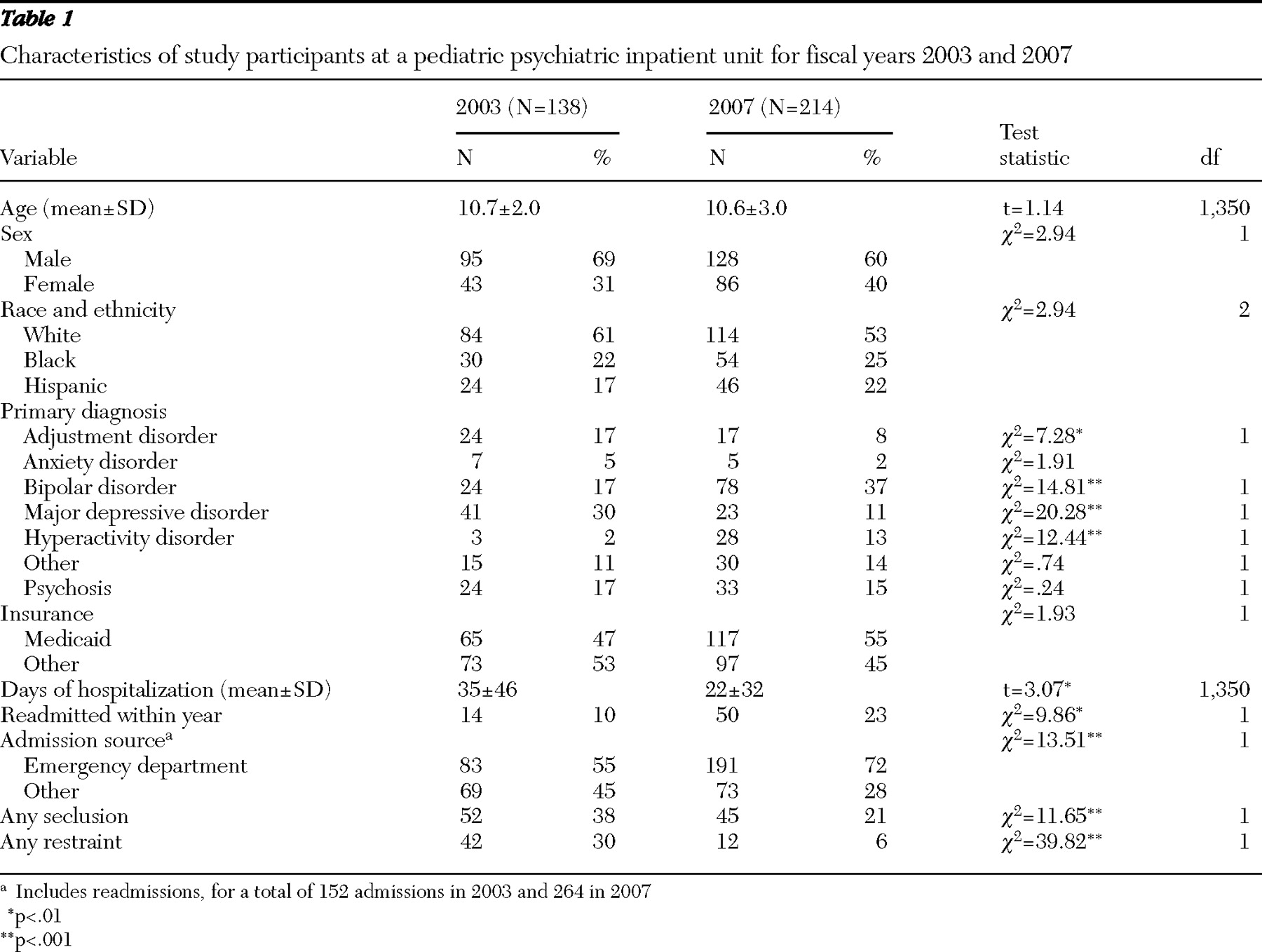
A total of 755 children were admitted to the service during the five-year study period and accounted for 998 separate admissions. Demographic and clinical characteristics of the children admitted in FY 2003 and FY 2007 are summarized in
Table 1 .
Age, sex, race-ethnicity, and insurance coverage distributions remained stable over the study period, with an overall median age of 11 years (range three to 15). For the overall study period, the sample consisted predominantly of boys (63%). Most of the children were white (52%), 25% were black (25%), and 23% were Hispanic. Slightly over half (52%) of the children were covered by Medicaid. In contrast, the diagnostic composition of the sample changed considerably ( χ 2 =49.01, df=6, p<.001), with fewer children discharged in FY 2007 with a primary diagnosis of depressive or adjustment disorders (depression, OR=.41, CI=.21–.80; adjustment disorders, OR=.29, CI=.16–.50) and more with a diagnosis of bipolar disorder or hyperactivity (bipolar, OR=2.72, CI=1.61–4.59; hyperactivity, OR=6.77, CI=2.02–22.74). The average length of stay decreased by a mean of two days per year, dropping from 35 days in FY 2003 to 22 days in FY 2007, for an overall change of 37%. During the same interval, children were more likely to be readmitted to the service within the same year (OR=2.7, CI=1.43–5.11) and to come in as nonelective admissions via pediatric emergency services (OR=2.18, CI=1.43–3.30).
Restraint and seclusion use
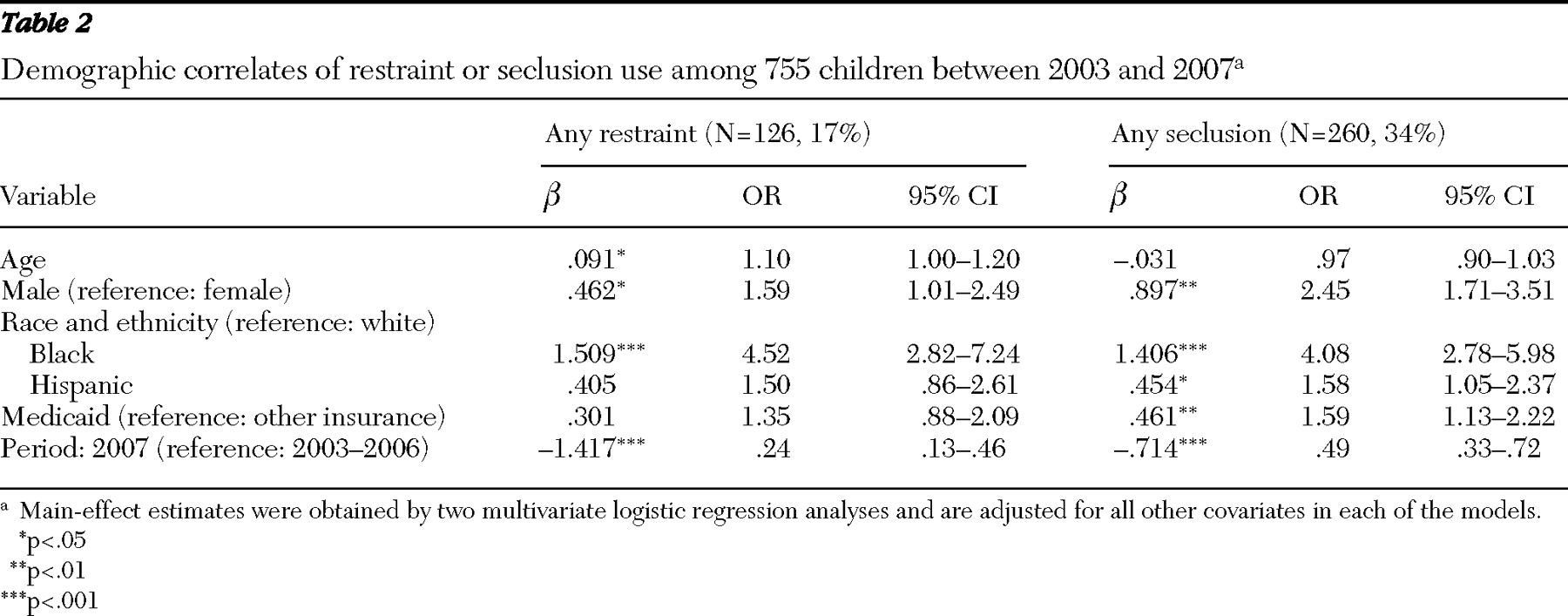
A total of 2,230 restrictive interventions occurred during the study period, comprising 559 restraint events (25%) and 1,671 seclusion events (75%). Although the five-year period prevalence of restraint and seclusion is hardly informative given the time trends described below, during each year of the study a small number of patients (approximately 5%) accounted for a disproportionately large number of the restraint and seclusion events (approximately 50% for both). Demographic patterns emerged in the use of restraint and seclusion, even after multivariate adjustment (
Table 2 ). Boys were more likely than girls to be restrained or secluded, and each additional year in age conferred a slightly increased likelihood of restraint (but not seclusion). Children covered by Medicaid were more likely to be secluded (but not restrained). Even after adjustment for age, sex, insurance status, and fiscal year of the study, strong racial differences emerged. Black children were more than four times as likely to be restrained or secluded as their white peers; Hispanic children were 50% more likely than whites to be restrained or secluded, although the difference was statistically significant only for seclusion. Diagnostic variables were not included in the final regression models, because they did not significantly improve the models' fit, and because their administrative source made their accuracy and clinical usefulness questionable other than for the purpose of description of the study sample.
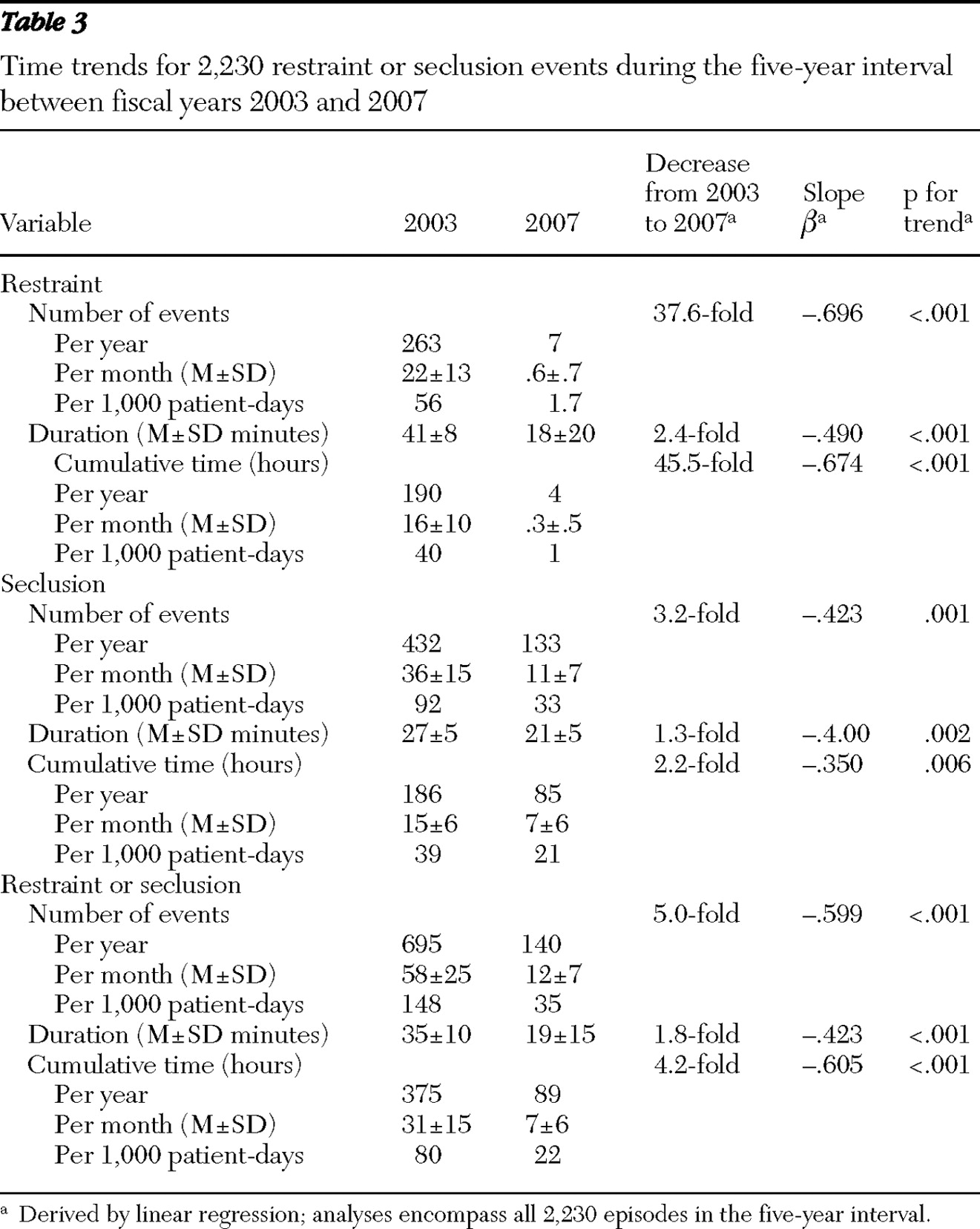
Time trends
Table 3 depicts the overall change in the frequency and duration of restraint and seclusion use between FY 2003 and FY 2007. During this time, and after the complete implementation of the CPS model by early 2006, there was a marked reduction in the use of restraints (from 263 to seven events per year, representing a 37.6-fold reduction, slope
β =-.696) and seclusion (from 432 to 133 events per year, representing a 3.2-fold reduction,
β =-.423). The mean duration of restraints decreased from 41±8 to 18±20 minutes per episode, yielding cumulative unitwide restraint use that dropped from 16±10 to .3±.5 hours per month (a 45.5-fold reduction,
β =-.674). The mean duration of seclusion decreased from 27±5 to 21±5 minutes per episode, yielding cumulative unitwide seclusion use that dropped from 15±6 to 7±6 hours per month, a 2.2-fold reduction (p for trend <.01 or better for all slopes).
Staff injuries were formally documented in 180 instances: 55 in FY 2005, 101 in FY 2006, and 24 in FY 2007. Of note, 83% of the staff injuries in the peak year of FY 2006 occurred during the six months beginning midway through the CPS implementation phase.
Discussion
Our findings show marked reductions in the use of restraint and seclusion in a psychiatric inpatient setting for children after the implementation of the CPS model of care. In the 18 months after the model was fully adopted, reductions were much more pronounced for use of restraint than for use of seclusion, suggesting that restraint may be a more achievable first target of reduction efforts. Changes were primarily driven by decreases in utilization and to a lesser extent by shorter duration of events. By the end of the study period, the overall rates of restraint use had fallen to within the national range for comparable settings (.5–2.0 events per 1,000 patient-days) (
27 ), although the rates fell short of the experience of facilities that have virtually eliminated use of restraint and seclusion (
28 ).
These changes, and the fact that over time a substantially smaller proportion of children underwent seclusion or restraint during their hospital stays, were possible even in the context of fairly steady clinical conditions. Indeed, by several parameters the unit became more acute during the study period, in keeping with national trends (
29 ) and a movement away from inpatient psychiatric care except for the most impaired children. Length of stay decreased, more children were readmitted or admitted via emergency services, and more children were admitted for aggression and externalizing disorders, each of which could have confounded some of our findings. Bipolar disorder became a particularly common discharge diagnosis during this interval, consistent with secular trends reported by others (
30,
31 ). Regrettably, we did not have consistent information regarding trauma histories, an omission that is worth noting given that trauma-informed approaches have been found to be effective (
32,
33 ) and likely to complement restraint and seclusion reduction efforts.
Even though racial and ethnic differences attenuated over time (data not shown), children from racial-ethnic minority groups in our study were much more likely to be restrained or secluded, particularly during the preimplementation years and even after the analysis controlled for socioeconomic status. Of note, we did not have consistent IQ information for the children in this study, an important omission considering that in a previous study conducted in the same inpatient unit we had found that racial differences in aggression were no longer significant after we controlled for full-scale IQ (
34 ). Whatever the underlying explanation, disparities such as those reported here are troubling and should remain a focus of clinical attention, especially because they are consistent with the experience of other investigators (
35,
36 ).
Six core elements have been deemed essential for the systematic reduction of restrictive interventions in inpatient settings: leadership support of organizational change, use of data to inform practice, workforce development, use of seclusion and restraint prevention tools, inclusion of patients and families, and rigorous debriefing after restrictive events (
37,
38 ). The process of change described here spans the first four of these tenets by training clinical staff in the proactive assessment of lagging cognitive skills that may ultimately contribute to aggressive behavior among children and by teaching them new strategies instead of resorting to alternative reward-and-consequence-driven behavioral approaches. Indeed, once-favored behavioral milieu management models, such as token economies, have largely fallen out of favor and been criticized for contributing to the very behaviors they seek to target (
39 ).
Our study needs to be considered in light of its limitations. First, given that several milieu changes were instituted at the same time as part of the CPS model of care, our results do not permit a clear delineation of which exact components were active in reducing use of restraint and seclusion. Some of those other key operational changes included more consistent inclusion of families and caregivers in treatment, extension in visiting hours and phone call accessibility, formalization of family education and support programs to teach the basic elements of the model, and initiation of the weekly multidisciplinary supervision meeting described earlier. Second, we did not include objective measures of aggression (
34 ) or of patient outcomes (
40,
41 ), both of which would have strengthened our results. Third, we did not include information on psychotropic medications (particularly emergency use and use as needed) or on the involvement of hospital security services. Fourth, we have no systematic data on child injuries, and the data on staff injuries that we included were limited and provide no detail as to injury type, severity, or possible relationship to restraint or seclusion events. Fifth, we did not include objective measures of adherence to the CPS model, such that drift in fidelity over time and across the many staff members cannot be quantified. Finally, we did not formally assess the perceptions of staff, children, and patients' families concerning the implementation of the new model of care—and particularly during times of increased injuries. Using available instruments (
42 ) to track these attitudes over time at the individual and organizational levels could help address resistance to change and help maintain hard-earned gains.
Despite these shortcomings, our study has noteworthy strengths. First, its five-year observation period is unique and provided baseline and follow-up periods long enough to establish that changes were not transient or simply a result of seasonal variations. Second, our study extends preliminary experience with the CPS model in another inpatient setting (
20,
22 ), thus providing support for the generalizability of the model. Moreover, our incorporation of remote training and staff supervision through videoconferencing supports the transportability of the model and represents an innovation that may be especially relevant to other facilities contemplating its adoption. Finally, to the best of our knowledge this is the first study to apply a well-described, conceptually grounded, and manualized intervention to reduce use of seclusion and restraint in a pediatric setting.
Conclusions
In summary, restraint and seclusion reduction was possible and safely implemented in an inpatient setting through the concerted adoption of the CPS model of care. Future replication and research efforts are warranted to test the model in other child psychiatric settings. Indeed, our findings should be considered pilot data to support a randomized clinical trial to more formally test the efficacy and effectiveness of CPS in real-world settings. Such a trial could be designed with different facilities (or with different units within larger settings such as state hospitals) as the unit of study and randomization.
Apart from replication and more formal testing in inpatient settings, adaptations to other relevant facilities could be considered. Although specifically applied to a high-utilization psychiatric inpatient setting in our pilot study, the CPS approach could conceivably be adapted to the care of aggressive and volatile children in other settings, including pediatric floors of hospitals, residential schools, juvenile justice settings, or pediatric emergency services. In all of these settings the resort to restraints remains a standard practice in acute situations. Exploring adaptations to these and other relevant pediatric settings seems worthwhile and likely feasible when one considers that the CPS model was originally developed for the management of aggressive and oppositional outpatients (
25 ) and was only later adapted to the specific requirements of an inpatient environment. Given the serious risks that have been associated with the use of restraint and seclusion, pursuing alternative approaches to the management of aggressive children and adolescents remains a pressing clinical priority.
Acknowledgments and disclosures
This project was supported in part by the Connecticut Yankees, the Albert J. Solnit Endowment at the Yale Child Study Center, and Mr. and Mrs. Joshua Needleman. The authors thank Fatih Ozbay, M.D., and Douglas Leslie, Ph.D., for assistance on an earlier draft and the staff of the Children's Psychiatric Inpatient Service, whose commitment and tireless efforts led to the changes described herein.
The authors report no competing interests.