Religion is a significant cultural theme of American life that has been well documented. National surveys have shown that about 95% of Americans affirm that they believe in God (
1,
2 ). In addition, 42% reported attending church in the past week (
2 ), and nearly 75% of Americans reported that religious beliefs grounded their approach to life (
3 ). It is therefore not surprising that clergy members play an important role in the lives of Americans, providing counseling and other services for parishioners and their family members. In fact, the clergy plays a heavy role in the treatment of mental illness, serving approximately 40% of Americans with mental health problems (
4 ). Some studies have even shown that clergy members are more likely than psychiatrists and psychologists combined to be sought out for guidance with mental health problems (
5,
6 ). Research on collaboration between mental health providers (particularly psychiatrists) and clergy members is somewhat limited in terms of volume of data, but it is clear that collaboration between the two professions could enhance treatment of mental health problems and help to destigmatize mental illness.
The volume of Americans turning to the clergy for assistance with mental health issues is staggering. Even of individuals who identified themselves as "not religiously active" and "seldom attending religious services," 16% reported seeking help from clergy members for personal problems (
6 ). Studies have shown that women, people who have been widowed, and elderly persons all tend to turn to a religious clergy member rather than to a mental health specialist (
5 ). An interesting fact is that clergy members equal mental health specialists in the number of individuals who have sought their care and have diagnoses of major depression, bipolar disorder, schizophrenia, obsessive-compulsive disorder, and antisocial personality (
5 ).
This fact raises the natural question of whether members of the clergy are adequately trained to counsel persons with major psychiatric illnesses. A survey of nearly 2,000 Methodist pastors revealed that although 95% believed that incorporating counseling training into seminary was important, 25% felt that their seminary training had significantly contributed to their competence as pastoral counselors (
7 ). The clergy has reported referring less than 10% of those counseled to mental health specialists (
8,
9,
10 ), yet 50% to 80% of clergy members have reported that counseling training in seminary and postseminary continuing education was inadequate (
8,
10,
11,
12 ) and 45% stated that they received no training on referral criteria (
10 ).
Much of the literature on clergy mental health training was published in the 1970s and 1980s. Whether the systems for training clergy have since adapted to the reality that clergy serve as frontline mental health workers remains unknown. In addition, little is known about the clergy's work in areas underserved by mental health care providers. This survey study examined the level of preparedness to recognize and treat mental illness among Hawaii's Protestant clergy and lay church employees.
Methods
This study surveyed ministers and lay church workers in the state of Hawaii to ascertain their perceptions regarding mental illness, its cause, contributing factors, and beneficial treatments. A database service was contacted to create a list of Protestant Christian churches in the state of Hawaii with the following denomination classifications: mainline (Episcopalian, Lutheran, Methodist, Presbyterian, and United Church of Christ), independent (Baptist or general Christian), charismatic (Assemblies of God, Four Square, and Pentecostal), and Seventh Day Adventist. Catholic, Greek Orthodox, and other churches were excluded from the search because of limitations in study funding and time.
Pastors from the qualifying churches were sent a packet with a letter of introduction, a copy of the survey, and instructions on how to complete the survey online. The letter of introduction included contact information for the primary investigator and the university's institutional review board, and consent was obtained in the first question of the survey. Pastors were asked to distribute the survey to other clergy on staff and to lay workers in the church who were directly involved with the church's ministry. Potential participants also received a reminder by phone call. The survey took about ten minutes to complete. Information including opinions about the role of clergy as frontline mental health workers, level of education, and amount of training in mental health was obtained. Ability to recognize symptoms of mental illness was assessed, along with attitudes regarding the referral process. Participants also were given two case vignettes and asked to comment on them. In the first case, an energetic young church volunteer has begun speaking incessantly about his spiritual awakening and is no longer sleeping or attending to his hygienic needs. In the second case, an elderly woman whose husband was reported to have passed away six months ago appears to be overwhelmed by her grief and has stopped attending church activities.
Data were collected between August and October 2006. Descriptive analyses were performed. Chi square analyses were conducted to examine the relationship between demographic information, hours of training, mental illness recognition, importance of shared beliefs, root causes of mental illness, counseling, and stated concerns. Logistic regression was conducted to determine the variables most closely associated with the importance of shared beliefs.
Results
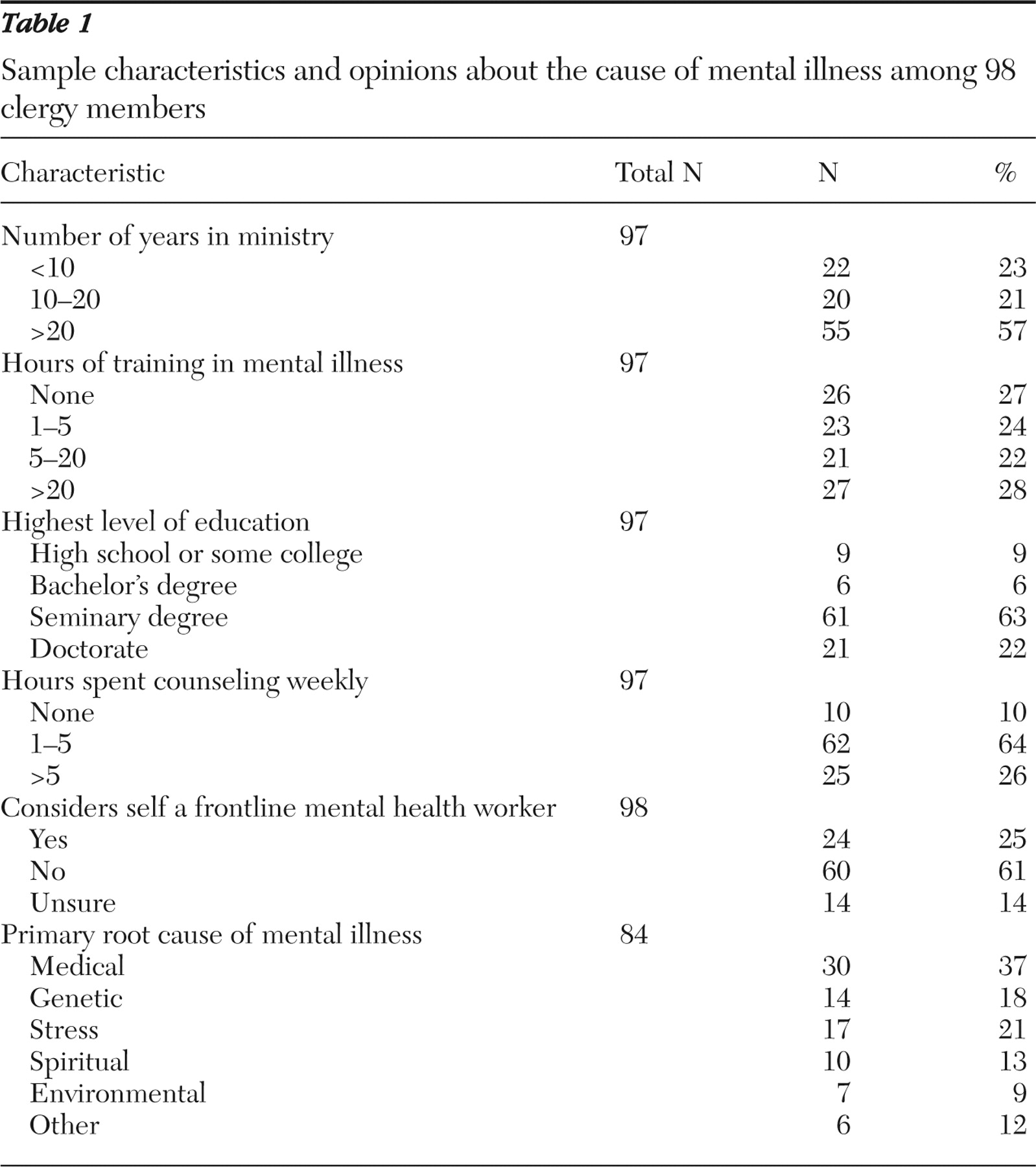
Ninety-eight clergy members responded to the survey. Information on race and age was not collected. Seventeen respondents were female and 81 were male. The sample is described in
Table 1 . Most of the respondents reported having served more than 20 years in ministry and having a seminary degree. There was an equal distribution between groups in terms of the number of hours of mental illness training completed, but 90% reported spending time counseling weekly. Most respondents did not consider themselves to be frontline mental health workers, but those who did were more likely to have had more than 20 hours of training in mental health (
χ 2 =22.37, df=6, p=.001). Respondents with a doctorate were also most likely to have completed more than 20 hours of training in mental health, and those with a college degree or below were most likely to report having had no mental health training (
χ 2 =4.61, df=1, p=.032).
Participants were asked whether they felt that their training was adequate to recognize mental illnesses, such as major depression, bipolar disorder, and schizophrenia. A total of 29% (28 clergy members) responded yes, 55% (54 clergy members) responded no, and 16% (16 clergy members) were unsure. Respondents with more than 20 years in ministry were more likely to feel adequately trained to recognize mental illness, but the difference was not significant. Those with more than five hours of training in mental health were significantly more likely to feel adequately trained to recognize mental illness ( χ 2 =27.88, df=6, p<.001). There was no significant difference in the interaction of ability to recognize mental illness with level of education or with the number of hours spent counseling.
Participants were asked whether a mental health professional's religious beliefs should match those of the client referred for treatment. Respondents were asked to comment on whether shared religious beliefs are essential, important, or not essential. Most respondents reported that they are important (40 clergy members, or 41%) or not essential (43 clergy members, or 44%), but 15% (15 clergy members) reported that shared beliefs are essential. The four variables most strongly associated with whether a respondent considered shared beliefs essential were level of education (less than a doctorate level, log likelihood=-24.83, df=2, p=.040), church group (Seventh Day Adventists and charismatic, log likelihood=-26.01, df=3, p=.032), whether the person considered himself or herself to be a frontline mental health worker (log likelihood=-25.94, df=2, p=.013), and spending more than five hours counseling per week (log likelihood=-24.94, df=2, p=.036). The number of hours of mental health training received was not associated with the response to this question.
Participants were asked their opinions of the primary root cause of mental illness. Medical cause was the most commonly cited cause (
Table 1 ). Respondents who reported spending the greatest number of hours counseling per week were most likely to cite environment as the primary root cause of mental illness (
χ 2 =19.01, df=10, p=.040). Primary causes listed under "other" were difficult to categorize given the wide range of responses—for example, "demonic oppression or possession," "unresolved anger … or the result of idolatry in the family line," "medications prescribed by doctors," "family's lack of intimacy," and "lack of authentic community and a sense of belonging and security within that community." The number of hours of mental health training a clergy member had completed was not significantly associated with how he or she answered this question.
Twenty-four clergy members (25%) indicated that they would self-counsel for both case vignettes, 37 clergy members (38%) would counsel for one of the cases, and 37 clergy members (38%) would counsel for neither case. Analysis of the case vignettes showed no statistically significant differences between reported adequacy of training and self-counseling. However, more than 40% of the 24 clergy members who reported inadequate training indicated that they would provide counseling for these cases. Twenty-nine percent of respondents (18 clergy members) reported insufficient skills, and another 29% (18 clergy members) responded no when asked whether they had any concerns about working with parishioners with mental illness. Others cited safety concerns, limited resources, and poor collegiality shown to them by mental health professionals.
Discussion
The clergy surveyed felt inadequately trained in recognition and treatment of mental illness. However, there was a strong tendency to counsel regardless of level of training or feelings of adequacy and despite reporting a belief that the most common cause of mental illness is medical. This was reflected in the case vignettes; more than 40% of respondents who admittedly lacked training said they would counsel the individuals described in the vignettes. These dramatic findings demonstrate that many clergy members were not adequately trained to treat mental illness but proceeded with doing so. Their "patients" were not being referred to psychiatrists partly because clergy members' ability to identify serious mental illness was lacking or absent. This finding speaks to the need for collaboration—and for mental health providers and ministers alike to recognize both the benefits of and barriers to collaboration—so that more can be done to enhance the treatment of persons with mental illness.
Collaboration can be enhanced by addressing several barriers. Some clergy members have expressed concern that mental health specialists may undermine or show contempt for the faith of individuals who are referred (
13 ), and poor collegiality between professions was cited in this study. Awareness and sensitivity on the part of psychiatrists may go a long way in breaking down this barrier. In addition, some clergy members were more likely to consider shared religious beliefs between the provider and the treatment seeker to be essential, especially respondents with less education than a doctorate degree, clergy members from Seventh Day Adventist or charismatic churches, and those who spent more time in weekly counseling services. Surprisingly, the amount of training received in mental health care was not associated with a minister's opinion of whether shared beliefs were essential. This barrier could limit the amount of referrals from clergy to mental health professionals.
One of the major themes permeating the literature is the role of clergy members as frontline mental health workers (
14 ), a theme mentioned significantly more often in secular than in religious journals (
15 ). However, there is a clear disconnect between the number of clergy members who provided counseling services to their parishioners and the number who considered themselves to be frontline mental health workers.
Although this survey opened a channel of communication between the religious and psychiatric communities in Hawaii, there are some limitations to consider when interpreting the data. First, not all types of churches were surveyed, and results may not be applicable to religions other than those included in this project. A much broader study should be attempted to include the myriad religions represented in local and other American communities. Second, this study was limited to clergy in Hawaii, and the ability to generalize results could be questioned. It is suspected that Hawaii's clergy is similar to cohorts on the mainland, as many clergy members have likely received their training outside of Hawaii because of the current lack of a seminary in the state. But such similarities cannot be guaranteed without comparative studies. Third, the rate of response to the survey could not be calculated, because clergy were asked to distribute the survey to other clergy and lay ministers on staff.
Also, during the phone call reminders, a few potential participants indicated that they were suspicious of the motives of the primary investigators. Some ministers related fears that data would somehow be used to prevent clergy from continuing to work with parishioners with mental illness, and, despite reassurances, a few stated that they would not participate. This situation may create bias in the data, and results therefore may not be fully representative. Despite these limitations, few studies on this topic have been done in the past decade. Given the high number of Americans who seek clergy for counseling services, this is a topic that should be given ongoing consideration.
Conclusions
It seems to be the case that more specific training is needed for clergy in terms of recognition and treatment of mental illness. Knowledge of when to refer parishioners to mental health professionals as well as what the clergy may expect after referral would be ideal topics for such training. Many clergy surveyed commented on their ability to provide transportation for a parishioner who needs to see a physician or to help encourage medication adherence. Psychiatrists may consider including clergy in treatment planning or in hospital crisis interventions. Despite the obstacles, collaboration between clergy members and psychiatrists is essential. Awareness, sensitivity, and an open-minded approach by both psychiatrists and clergy members may provide an advantage for religious mental health consumers.
Acknowledgments and disclosures
This research was funded, in part, by an educational research grant from the Akeroyd Foundation. The authors thank Reverend Ian Farrell for his assistance in conceptualizing the project and contacting potential survey participants.
The authors report no competing interests.