Psychopathology can worsen with increasing age, especially when it remains untreated or co-occurs with medical conditions or substance abuse, and it tends to reduce life quality, longevity, and intervention adherence (
1,
2,
3,
4,
5,
6,
7,
8 ). Although outpatient treatment of mental illnesses has been increasingly emphasized for this population, some persons with greater symptom severity rely on inpatient care, and it is not uncommon for rehospitalization to be needed within a few months of discharge (
9 ). However, few analyses are available on recent patterns and predictors of psychiatric rehospitalization among elderly persons. A better understanding of early readmission could help mental health professionals be alert to risks of readmissions that may result in high personal and economic costs.
Using data for all elderly Medicare beneficiaries (
10 ) who met inclusion criteria and were hospitalized for psychiatric reasons in the first half of 2002 (N=41,839), this study examined relative influence of the length of baseline hospitalization and presence of baseline comorbidity on the hazard of geropsychiatric rehospitalization within six months of discharge. The intent was to inform practices that prevent, when possible, the life disruption of repeated inpatient stays.
The relationship between the length of the baseline hospitalization and readmission in the next few months is complex. For example, a patient might have a short stay that achieved adequate stabilization because the mental illness was relatively manageable, and the short stay would not affect the probability of rehospitalization. For a different patient, the same length of stay might be too short, which translates into discharge of a poorly stabilized patient at higher risk of readmission. However, when longer stays reflect more severe or difficult-to-manage clinical conditions, an early readmission may be caused by enduring disease characteristics or personal circumstances that would have been difficult to modify in a prior hospitalization. Despite this complexity, the economic and clinical importance of psychiatric rehospitalization points to the potential value of better understanding how well it can be predicted by characteristics of a baseline stay, as well as by other patient characteristics, such as comorbidity and demographic characteristics. Data on the full Medicare population allows examination of these associations.
Most investigations in this area focus on geropsychiatric hospitalization rather than early readmission, and almost all are cross-sectional and descriptive (
8,
11 ) rather than longitudinal. Two longitudinal investigations were conducted before 1996. One of the studies found that among elderly persons with serious psychopathology, those who were unmarried and those with strained family relations were more likely than their respective comparison groups to be hospitalized (
12 ). The other study found that most elderly inpatients (78%) retained their preadmission living arrangements after discharge (
13 ).
More recently, researchers have focused on the sociodemographic and clinical description of geropsychiatric inpatients and on service use. A majority of investigations assessing clinical profile (
6,
9,
14 ) report that depression or bipolar disorder is the most common reason for admission; that primary conditions often co-occur with anxiety disorders, substance abuse, or personality disorders; and that presence of dementia or cognitive impairment among elderly inpatients complicates diagnosis and treatment. Except for gender and marital status, few associations between characteristics and readmission have been reported (
14 ).
Research suggests that about .6% of elderly persons on Medicare are hospitalized nationally for mental illness (
15 ). Among these hospitalizations, differences exist between admissions to psychiatric units of general hospitals and medical units of general hospitals. Younger age and more psychiatric comorbidity are more common in the former, and older age and more medical comorbidity are more common in the latter (
16 ).
Thus, except for prediction of medical versus psychiatric admissions (
16 ), studies of inpatient psychiatric stays of elderly Medicare beneficiaries (and most other elderly populations) are descriptive and cross-sectional rather than inferential. Surprisingly, given the scope of the problem, only one conclusion can be reached empirically in relation to geropsychiatric recidivism within a short time of hospital discharge (typically three to six months)—it occurs at a rate comparable to that of the nonelderly (
17 ).
Our study used 2002 data and appears to be the first longitudinal investigation of geropsychiatric inpatient care for a large national population of elderly persons with Medicare, and it is among the first to examine influence of both length of baseline inpatient stay and presence of comorbidity at baseline on risk of psychiatric rehospitalization. Length of stay and co-occurring conditions can both reflect elevated symptom severity (
18 ) and signal vulnerability for early readmission. We examined differences in these two characteristics between persons with a primary index diagnosis of an affective disorder (for example, depression and bipolar disorders) and those with a primary index diagnosis of a nonaffective disorder (for example, schizophrenia and substance abuse) after predicting psychiatric readmission in the entire study population from baseline psychopathology type, baseline length of hospital stay, and baseline presence of comorbidity with psychiatric, medical, and substance use disorders. Although we could not control for other potentially important influences on readmission, most notably social support and prior service use, we adjusted for gender, age, ethnicity, geographic region, facility location (urbanicity), expenditures of the state mental health agency, and community characteristics (for example, local median incomes).
Methods
Use of Medicare claims
After obtaining approval from the Rutgers University Institutional Review Board, we took data from year 2002 Medicare Provider Analysis and Review (MedPAR) files. The files contain stay-level data summarizing information from Medicare claims (submitted by providers to the Centers for Medicare and Medicaid Services [CMS]) for inpatient stays in hospitals or skilled nursing facilities. Using the
International Classification of Diseases, 9th Revision, Clinical Modification (
ICD-9-CM ), we identified MedPAR stays with a primary admission diagnosis of depression, bipolar disorder, schizophrenia, substance abuse, or other more commonly occurring mental illnesses, excluding dementia or organic disorders. [An appendix showing the
ICD-9-CM codes used to classify these various psychiatric disorders, along with the codes for comorbid medical conditions, is available as an online supplement at ps.psychiatryon line.org.] The data yielded information on length of hospital stay (total days, including those covered by Medicare and by additional payers), demographic characteristics of the inpatient, and up to nine secondary diagnoses of comorbid medical or psychiatric conditions recorded during the stay. Comorbid conditions were identified using the
ICD-9-CM . Conditions were chosen for analysis because of their high prevalence or centrality in prior research on mental illness and hospitalization among the elderly (
7,
19 ).
Study population
Our study population included all persons age 65 or older who were enrolled in fee-for-service Medicare throughout 2002. Those with health maintenance organization coverage (about 15% of all beneficiaries) were excluded, because data on hospitalization for this group did not involve claim submission to the CMS. In addition, persons in skilled nursing facilities were excluded in order to maintain focus on community-dwelling individuals. We selected only persons who were hospitalized in the first six months of 2002 to ensure that a follow-up time window of six months was available in each case in order to model psychiatric rehospitalization. All administrative data were deidentified before analysis.
Regional differences and state mental health spending
The state in which a facility was located was grouped into four regions (Northeast, Midwest, South, and West). Expenditures of the state mental health agency per capita were taken from national estimates (
20 ), and divided into four categories, or quartiles, including lowest (less than $50), highest ($93 or more), and two intermediate ranges.
Community context of the facility
By using rural-to-urban continuum codes (
21 ) and linking them to MedPAR data by county of hospitalization, urbanicity was defined on a 9-point continuum that we divided into three categories: metropolitan areas (urban areas), nonmetropolitan areas adjacent to an urban location, and nonmetropolitan areas not adjacent to an urban location. Data on community context were taken from the U.S. census and linked by ZIP code to the psychiatric hospital location. These data included median community income (four categories, or quartiles, ranging from lowest, less than $31,170, to highest, $50,012 or more), percentage black or Hispanic (quartiles ranging from lowest, less than 4.65%, to highest, at least 32.90%), and percentage foreign born (quartiles ranging from lowest, less than 1.66%, to highest, at least 11.25%).
Analyses
Because follow-up time was censored at six months and many elderly beneficiaries were not hospitalized during this time, Cox proportional hazards regression was used to describe whether psychiatric rehospitalization was observed. Predictors of readmission included demographic variables, primary and secondary baseline diagnoses, length of baseline hospital stay, factors relating to geographic location of the facility, and community context of the facility.
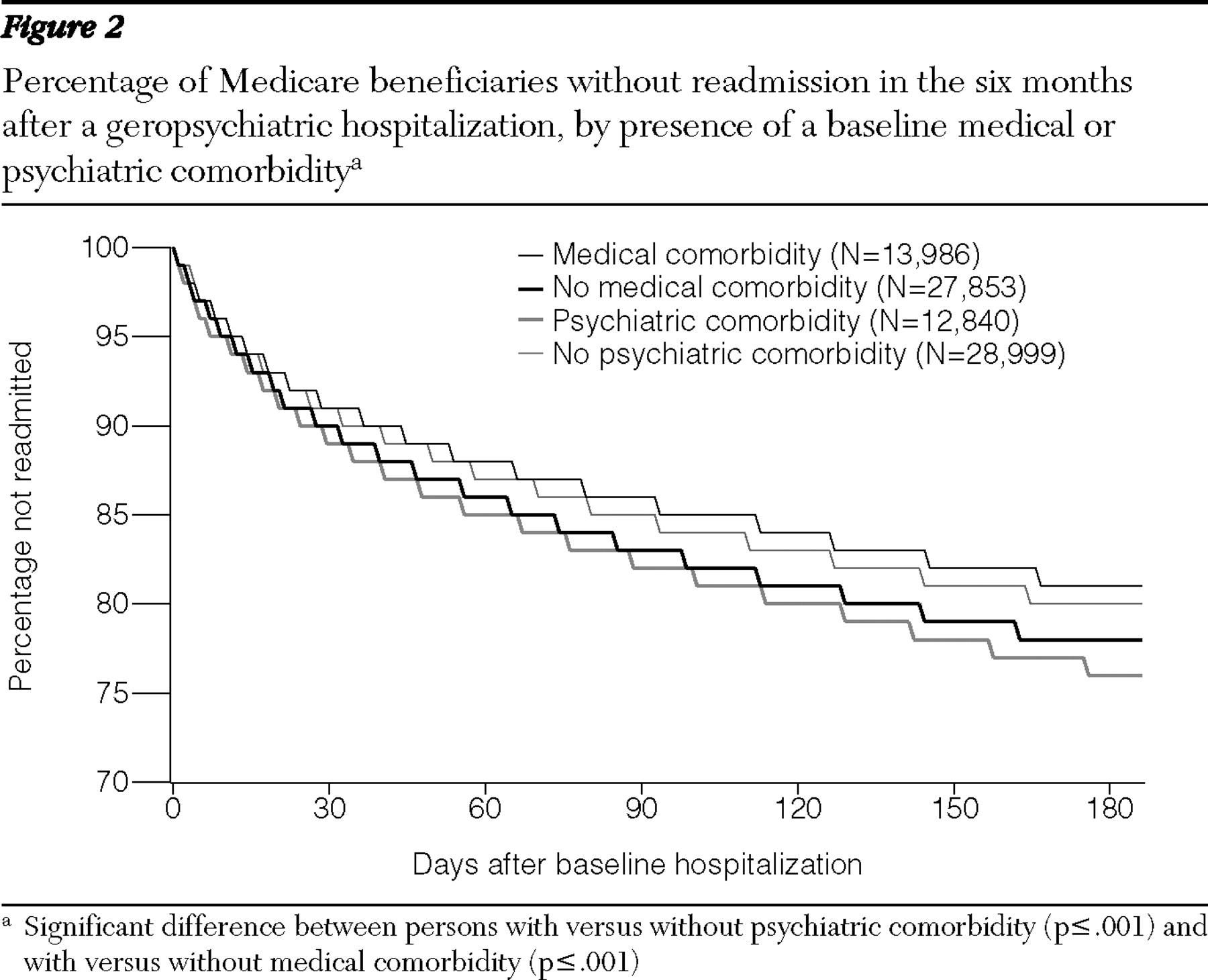
For bivariate comparisons (for example, time to readmission for depression versus schizophrenia or time to readmission for persons with versus those without medical or psychiatric comorbidity), we used the Kaplan-Meier technique. We plotted survival curves and used log-rank tests to compare differences in time to hospital readmission in relation to both primary baseline psychopathology type (for example, schizophrenia versus bipolar disorder) and presence versus absence of baseline medical or psychiatric comorbidity.
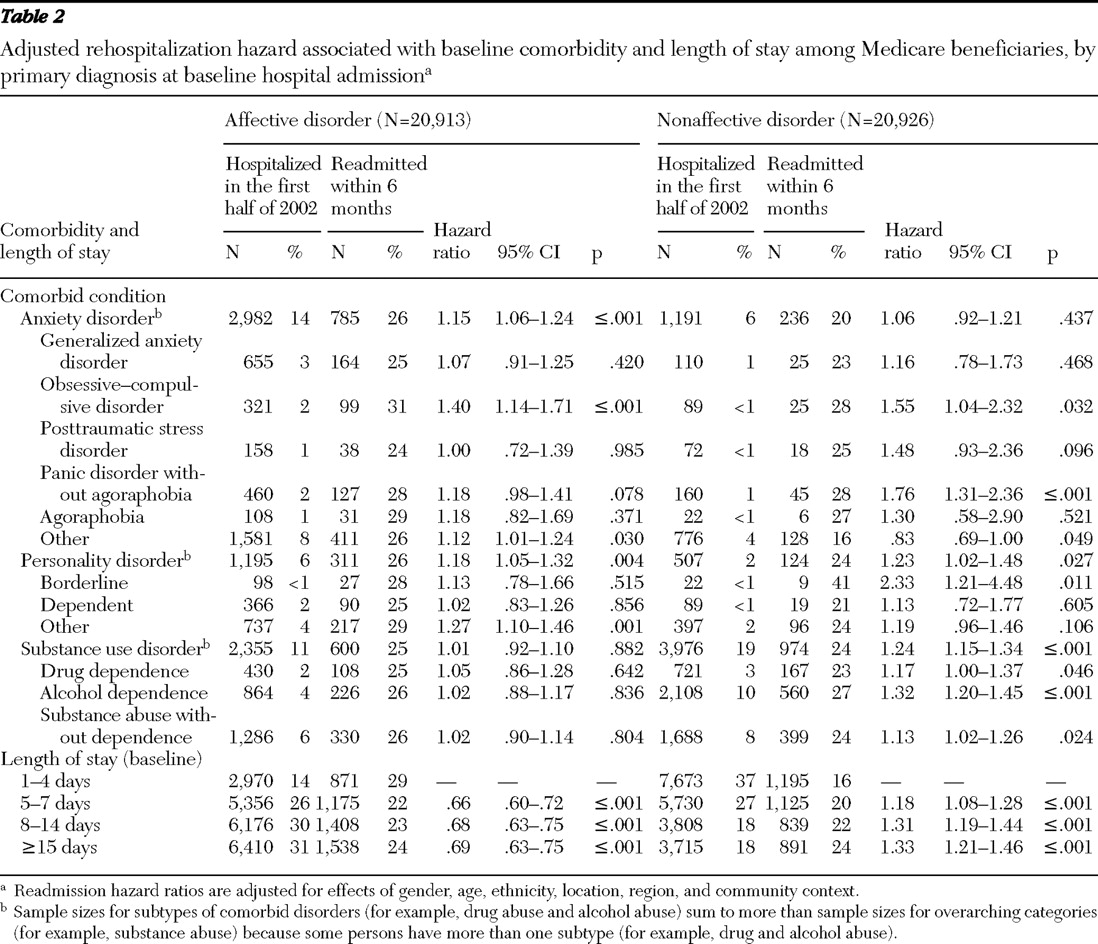
Length of stay and comorbidity were examined among persons with affective disorders at baseline (for example, depression and bipolar disorders) and those with nonaffective disorders at baseline (for example, schizophrenia and substance abuse) by fitting separate proportional hazard models predicting psychiatric readmission in each of the two groups from duration of baseline hospitalization and presence of baseline co-occurring conditions (anxiety disorder, personality disorder, or substance use disorders) or subtypes of conditions (for example, agoraphobia, dependent personality disorder, or alcohol dependence). Each model adjusted for effects of gender, age, ethnicity, location, region, and community context (data not shown). Two-sided Satterthwaite t tests then compared differences between the estimated parameters (based on standard errors from the model) to see if the comorbidity association was different between one primary diagnostic group versus another. We chose to analyze affective disorders versus nonaffective disorders because the distinction is theoretically and clinically clear and because relative to other common diagnostic distinctions (for example, schizophrenia versus other disorders), it divided our study population evenly and allowed for greater statistical power.
Results
Twenty-two percent of beneficiaries with baseline hospitalization were rehospitalized within six months (
Table 1 ). Readmission rates differed by primary index diagnosis (
Figure 1 ). Adjusted readmission hazard for schizophrenia (hazard ratio [HR]=2.63, p≤.001) and bipolar disorder (HR= 2.51, p≤.001) was greater than the readmission hazard for depression (HR=1.75, p≤.001) and substance use disorder (HR=1.38, p≤.001) ("other" psychiatric diagnoses was the reference group).
Comorbidity
Substance use disorder was the most commonly occurring comorbid psychiatric condition at the initial hospital stay, followed by anxiety disorder, depression, and personality disorder (
Table 1 ). About one-quarter of persons with at least one of these conditions were rehospitalized, and each condition increased (13%–28%) the adjusted readmission hazard within the first six months. More generally, persons with psychiatric comorbidity had greater readmission hazard than those without it (
Figure 2 ).
The opposite pattern was found when a medical comorbidity was present (
Figure 2 ). Having cancer, cerebrovascular disorder, dyslipidemia, or congestive heart failure decreased the adjusted readmission hazard for a psychiatric illness, albeit not equally. Having dyslipidemia or congestive heart failure reduced the hazard by about 15%, whereas having cancer or cerebrovascular disorder reduced it by about 25% (see
Table 1 ). Diabetes had very little influence. In general, persons with any of these medical conditions were less likely than other persons to have a psychiatric rehospitalization (
Figure 2 ).
Community context
Persons hospitalized in facilities in the Midwestern, Southern, and Western parts of the country had about 13% lower adjusted readmission hazard than did those in the Northeast. Regarding median income of the community, elderly persons hospitalized in neighborhoods with the two highest income ranges had about 10% lower hazard of rehospitalization than did those hospitalized in the lowest income range. Also, elderly persons hospitalized in communities with the largest percentage of foreign-born persons had about 10% greater adjusted readmission hazard than did those hospitalized in communities with the lowest percentage.
Baseline length of stay and comorbidity
Adjusted readmission hazard associated with length of baseline hospitalization and presence of comorbidity at baseline is shown in
Table 2 . A baseline stay of five or more days for an affective disorder was associated with a reduced readmission hazard (HR=.68, CI=.63–.73, relative to shorter stays), yet the opposite was true of rehospitalization for a nonaffective disorder (HR=1.26, CI= 1.17–1.35, p≤.001). Among those with a stay of four or fewer days, 29% of persons with affective disorders and only 16% of persons with nonaffective disorders were readmitted, yet among those with stays of 15 or more days, differences in readmission rates between those with affective disorder and those with nonaffective disorders were not apparent in readmission rates (24% in both groups).
Findings regarding psychiatric comorbidity differed between those with affective disorders and those with nonaffective disorders (
Table 2 ). For affective disorders, the presence of most personality disorders had a significant impact on readmission rates (dependent and borderline personality disorders were the exception), as did "other" anxiety disorder. For nonaffective disorders, the presence of comorbid alcohol dependence, panic disorder, borderline personality disorder, and drug dependence each had a significant impact. Obsessive-compulsive disorder increased the readmission hazard for both groups.
Discussion
About a fifth of hospitalized Medicare beneficiaries were readmitted for a primary psychiatric condition within six months of inpatient discharge. As anticipated from prior research (
14 ), the readmission rate was much higher (by about 50%) for persons with a primary diagnosis of bipolar disorder or schizophrenia than for those with other disorders. Beneficiaries with psychiatric comorbidities had a larger readmission hazard, after other factors were adjusted for. In contrast, medical comorbidities decreased readmission hazard, perhaps because persons with serious physical illnesses were rehospitalized more often for primary medical conditions than for primary psychiatric conditions; individuals with pressing health problems or their service providers must sometimes prioritize treatment for medical issues over psychopathology, because of competing demands for time or resources (
16,
22,
23,
24 ). Or perhaps persons with serious physical illnesses had more contact with the health care system, including outpatient mental health services, that helped avert an inpatient stay.
Statistically significant effects were found for sociodemographic characteristics and community context, but variables in this domain appeared generally less predictive of rehospitalization than did the clinical variables.
Length of stay, comorbidity, and readmission prevention
To reduce readmission following geropsychiatric hospitalization, results suggest that outpatient service providers could focus on persons with clinical characteristics related to length of prior hospital stay and comorbidity type. Readmission hazard associated with these two characteristics appears to differ between the group with affective disorders and the group with nonaffective disorders, although obsessive-compulsive disorder seemed to increase readmission hazard in both groups. For nonaffective disorders, longer length of the most recent psychiatric hospital stay or presence of alcohol dependence, drug dependence, panic disorder, or borderline personality disorder increased readmission hazard. For affective disorders, readmission hazard was increased by the presence of personality disorders other than borderline or dependent personality disorder, the presence of "other" anxiety disorder, or by having a short prior hospitalization.
To the extent that practical or ethical problems may make it difficult to randomly assign patients to conditions, our findings can provide guidance for planners, despite the limitations of observational data. In theory, the need for some of the early rehospitalizations might be reduced by implementing primary, secondary, and tertiary interventions.
In this context, primary prevention of recidivism begins before hospital discharge. Premature discharge should be avoided, especially among persons with affective disorders who are discharged quickly (in one to four days), for they appear more likely than their counterparts with longer stays to be rehospitalized. Use of specialized discharge planning, linkage, and aftercare is needed for those with affective disorders who are discharged quickly and for four other high-risk populations. The first high-risk population includes persons who have an affective disorder accompanied by a personality disorder other than dependent or borderline personality disorder or an "other" anxiety disorder. The second includes individuals with a nonaffective disorder accompanied by alcohol dependence, drug dependence, panic disorder, or borderline personality disorder. The third population includes all persons with the longest lengths of stay, and the fourth includes those with obsessive-compulsive disorder. In primary prevention of rehospitalization among persons fitting these clinical profiles, hospital staff could use "bridging strategies" in order to strengthen connection to community interventions before discharge (
25 ).
After discharge, secondary prevention of rehospitalization by outpatient staff can begin with use of administrative records or patient interview to determine length of most recent hospitalization and presence of varying forms of comorbidity among persons with affective disorders and those with nonaffective disorders. The information can be used to assess risk of early rehospitalization, and services can be offered that have been shown to prevent early rehospitalization—for example, psychiatric medication and psychotherapy (
26,
27 ), family involvement in care (
28 ), and assertive community treatment (
29 ). If early readmission is necessary, then both inpatient and outpatient staff can use a tertiary care approach to assess whether interventions that were not received could have helped to prevent rehospitalization, and then staff could plan for improved inpatient progress, aftercare attendance, and overall outpatient involvement strategies.
Limitations and suggestions for further investigation
Findings of the study presented here should be interpreted with caution because of the limitations inherent in using administrative data (
30,
31 ). Claims-based measures of hospitalization provide accurate data indicating that an inpatient stay occurred, how long it lasted, and what conditions were diagnosed. But they cannot profile a patient's participation or gains in treatment during the stay. Clinical history and symptom-level description of persons with geropsychiatric illness were unavailable to us, as were data on symptom severity, stage of illness, or outpatient care availability and use. Information on context was also limited. Factors related to social disadvantage may have been found to have a more substantial impact on readmission if they were assessed by using sources other than census data. In addition, we were unable to examine readmission among persons who relied exclusively on private funds for hospitalizations, but given the scope of Medicare coverage, these numbers are not likely to be large.
Finally, readmissions for reasons that were not primarily psychiatric were not examined in order to preserve study population homogeneity. We did not wish to include in our study population the persons who were readmitted to hospitals with primary medical conditions that were largely unrelated to mental illness or only partially associated (for example, falls or heart attacks caused in part by muscular rigidity or obesity, respectively, or other side effects of psychiatric medication). Study strengths include longitudinal focus on all Medicare beneficiaries in a homogeneous study population of elderly persons hospitalized at baseline with serious psychopathology. The size of the study population allowed us to examine more closely than most prior studies the readmission risk associated with subtypes of comorbidities that accompany all of the major primary mental illnesses, and we included more community context than is found typically in most clinically oriented research.
Future studies relying on primary data collection could further examine baseline length of stay, presence of various comorbidity types, and other potential indicators of symptom severity. Investigators could also focus on benefits of psychiatric medications or quality and type of other outpatient services in preventing recidivism among the elderly. Research is also needed on intervention nonadherence and readmission among persons with different clinical profiles and on benefits of referral and use of aftercare services after psychiatric hospital discharge.
Conclusions
Psychiatric rehospitalization is common among elderly persons. Efforts to reduce readmissions could focus on persons with risk factors related to length of baseline hospitalization and co-occurring disorders (for example, anxiety disorder, personality disorder, or substance abuse) that accompany major mental illness. Tailored efforts are needed because risk factors for readmission appear to differ in affective and nonaffective conditions.
Acknowledgments and disclosures
This study was supported by grants R01-MH-60831, R01-MH-076206, andR01-MH-058984 from the National Institute of Mental Health (NIMH) and by the Agency for Healthcare Research and Quality (AHRQ) through a cooperative agreement for the Center for Research and Education on Mental Health Therapeutics at Rutgers (grant U18-HS-016097), as part of AHRQ's Centers for Education and Research on Therapeutics Program.The content of this article is solely the responsibility of the authors and does not necessarily reflect the official views of NIMH or AHRQ.
The authors report no competing interests.