Each year substance abuse and dependence affect more than one in eight Medicaid beneficiaries, a higher prevalence than in Medicare or privately insured populations (
1 ). Direct Medicaid-funded treatment for addictions accounts for less than 2% of total expenditures, but the impact of substance use disorders on Medicaid programs may be much broader (
2 ).
Many mental and physical illnesses are more prevalent and more severe among patients with substance use disorders (
3 ). Several studies show greater mental health service use and higher mental health treatment costs for individuals with mental illness and a co-occurring alcohol or drug use disorder (
4,
5 ). Higher physical health care utilization or costs for patients with substance use disorders have been demonstrated in an academic medical center (
6 ), a privately insured population (
7 ), and a Medicaid health maintenance organization (
8 ). One study estimated that one-fifth of all Medicaid-funded hospital stays during the early 1990s were related to substance abuse or dependence (
9 ).
However, associations between substance use disorders and expenditures for general medical care have not been assessed at the level of state Medicaid programs, where many key policy decisions are made. Differences in individual risk factors and epidemiology make it difficult to generalize from private insurance or single providers to the more general impact on Medicaid-funded services within a state. Failure to capture all the costs related to substance use disorders may explain some states' low investment in addictions treatment.
Interest in and awareness of substance-related problems in primary care is growing (
10 ). Both psychiatric and substance use disorders are increasingly treated in the general medical sector (
11,
12 ), where primary care physicians now have more effective medications for treating substance abuse and dependence (
13 ). Emerging evidence suggests that good primary care is important for improving addictions outcomes (
13,
14,
15 ). Nevertheless, general medical conditions often take precedence over addictions in diagnosis and treatment in primary care settings.
Evidence for the impact of addictions treatment on medical expenditures is inconsistent, with some studies finding cost offsets and others not (
16,
17,
18,
19 ). Of particular concern to Medicaid programs are aging populations, in which substance use disorders are predicted to double between 1999 and 2020 (
20 ). Medical comorbidities increase with age, and substance use disorders may have an even greater impact on the health of middle-aged and older adults than on younger groups. Zywiak and colleagues (
16 ) found that medical cost offsets for women increased with age, suggesting that addictions treatment might improve the efficiency of care for some older adults.
In this study we examined Medicaid expenditures associated with substance use disorders among beneficiaries with behavioral health diagnoses in six diverse states. Using Medicaid claims and multiple regression analyses, we identified associations between diagnosed substance use disorders and other factors and expenditures for behavioral health and general medical care. We focused particular attention on expenditures for patients with diagnoses of substance use disorders that were attributed primarily to diagnoses other than mental or addictive disorders (that is, attributable to general medical disorders) and compared general medical expenditures among age groups.
Methods
Data
Medicaid claims for calendar year 1999 from Arkansas, Colorado, Georgia, Indiana, New Jersey, and Washington were obtained from the Centers for Medicaid and Medicare Services (CMS MAX files). Twelve-month diagnosed prevalence of mental disorders was identified from principal and additional International Classification of Disease, 9th Edition ( ICD-9 ) diagnoses 295.x to 300.x and 302 to 315. Substance use disorders were identified through diagnoses of alcohol or drug abuse or dependence, including ICD-9 codes 291.x, 292.x, 303.x, 304.x, 305.x (excluding tobacco), and 648.3. Fee-for-service claims were combined with encounter-level data submitted by managed care providers to compile a record of all Medicaid beneficiaries diagnosed as having behavioral health disorders.
All beneficiaries from 21 through 64 years of age without Medicare or private insurance were included in the analysis. The data included demographic information for each beneficiary, diagnoses for each treatment event in 1999, pharmaceutical claims, location of treatment (inpatient, outpatient, or long-term care facility), and the amount paid by Medicaid.
Beneficiaries with behavioral health disorders were classified in three mutually exclusive groups: those with severe mental illness, those with a psychiatric disorder but without severe mental illness (other mental illness), and those with an alcohol or drug use diagnosis and no additional psychiatric disorder (substance use disorder only). The severe mental illness and other mental illness categories were further divided into subgroups with and without co-occurring substance use disorders. For purposes of this analysis, severe mental illness was defined as psychoses, bipolar disorder, and major depression ( ICD-9 codes 295.x, 296.x). Other mental illness included all other psychiatric diagnoses not classified as a severe mental illness ( ICD-9 codes 297.x to 302.x, 306.x to 310.x, and 312.x to 315.x).
We used the Chronic Illness and Disability Payment System (CDPS) to estimate overall disease burden for each individual (
21 ). The CDPS is a predictive risk model developed for Medicaid populations that uses demographic, eligibility, and diagnostic data from claims from a previous year to develop risk scores for expected expenditures during a future year. For purposes of this study, we used scores for the current year to adjust for differences in co-occurring conditions across the various psychiatric and substance use disorder groups described above.
Expenditures
Expenditures are payments made by Medicaid for behavioral health and general medical treatment, including medications. We assumed that a primary diagnosis usually represents actual treatment for the respective disorder. It is possible that some conditions are diagnosed but not treated or that conditions are treated without the appropriate diagnosis. However, given the high rates of comorbid substance use and psychiatric disorders and the probability that some beneficiaries received addiction and psychiatric treatment during the same visit, we chose not to present expenditures for substance use and psychiatric disorders separately. Medicaid claims data do not permit a detailed examination of the type or quality of these treatments. Claims with a principal diagnosis of a mental or substance use disorder were classified as behavioral health expenditures. All other claims were classified as general medical payments. We included all medications used to treat mental or substance use disorders as behavioral health expenditures regardless of whether the person had a primary behavioral health diagnosis. Expenditures for all other types of medications were classified as medical expenses.
Analysis
The analysis focused primarily on the association between diagnoses of substance use disorders, alone or combined with a mental illness, and medical expenditures. Each state was analyzed separately to account for differences in Medicaid benefits, state policies, and variations in medical practice. Median yearly psychiatric and medical expenditures were calculated for beneficiaries with severe mental illness and other mental illness with and without a co-occurring substance use disorder. We used median expenditures because they are a more accurate measure of central tendency than means when extreme values are present. Because a large portion of total payments was driven by inpatient care, probability of inpatient treatment was analyzed separately.
Adjusted effects of substance use disorders on psychiatric and medical payments were next estimated by using semilogarithmic linear regression models. Estimates were adjusted for several confounders expected to be associated with utilization of health care. We adjusted for CDPS score, presence of severe mental illness, age, and whether the beneficiary qualified for Medicaid because of a disability. Other potential confounders included in the model were gender, racial minority status, and continuity of Medicaid coverage, measured as number of months enrolled in Medicaid. Several county-level variables that could affect utilization of services in each setting were also included in earlier versions of the models as potential confounders but were later removed because they were not significant. They included total number of inpatient beds and total number of physicians per 1,000 individuals, median family income, proportion with a high school diploma or higher, and proportion of the population classified as urban. Interactions among explanatory variables were examined in preliminary analyses and an age-by-substance use disorder term was included in one model. For purposes of comparing effects of risk adjustment on expenditures, we also analyzed the data using an almost identical model but omitting CDPS scores.
We separately identified the presence of ambulatory care-sensitive conditions (chronic obstructive pulmonary disease [COPD]; diabetes; asthma; ischemic heart disease; hypertension; congestive heart failure; pneumonia; cellulitis; dehydration; gastroenteritis; hypoglycemia; kidney and urinary tract infections; and severe ear, nose, and throat infections), but we did not include this in the regression model because several of the conditions overlap with conditions measured by CDPS scores (
22,
23 ). (Ambulatory care-sensitive conditions represent diagnoses for which primary care can effectively prevent hospitalization.)
Approval for this study was obtained from the committees for the protection of human subjects at the University of Massachusetts Medical School and at Dartmouth Medical School.
Results
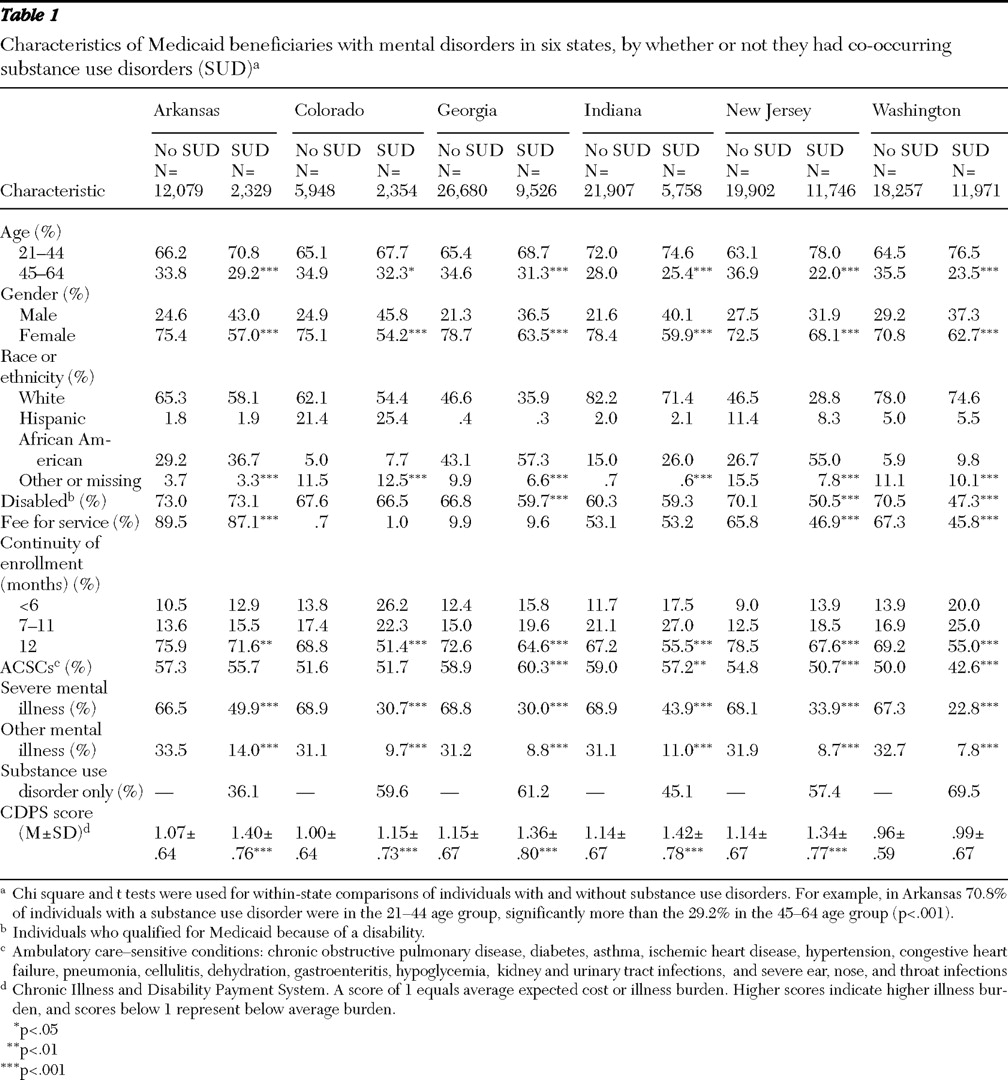
A total of 148,457 persons met selection criteria, and 43,457 (29.3%) had diagnoses of substance use disorders. Results for the six states are shown in
Table 1 . [A table listing the Ns for the percentages presented in
Table 1 is available as an online supplement at
ps.psychiatryonline.org .] The percentages of beneficiaries with diagnoses of substance use disorders were 16.1% in Arkansas, 28.4% in Colorado, 26.3% in Georgia, 20.8% in Indiana, 37.1% in New Jersey, and 39.6% in Washington. Younger age, male gender, ethnic or racial minority group membership, and shorter periods of Medicaid enrollment were positively associated with having a substance use disorder (p<.05). The most frequently observed ambulatory care-sensitive conditions in all states combined were COPD (16%), diabetes (10%), and asthma (9%). Rates of these conditions were similar across states. In the group with severe mental illness and the group with other mental illness, a co-occurring substance use disorder was significantly associated with higher prevalence rates of these co-occurring physical conditions in Georgia, Indiana, New Jersey, and Washington; rates were lower for those with diagnoses of substance use disorders alone (p<.05). CDPS scores for individuals with a substance use disorder were significantly higher in all states for the groups with severe mental illness and with other mental illness. [A table presenting the scores for these two diagnostic groups is available as an online supplement at
ps.psychiatryonline.org. ]
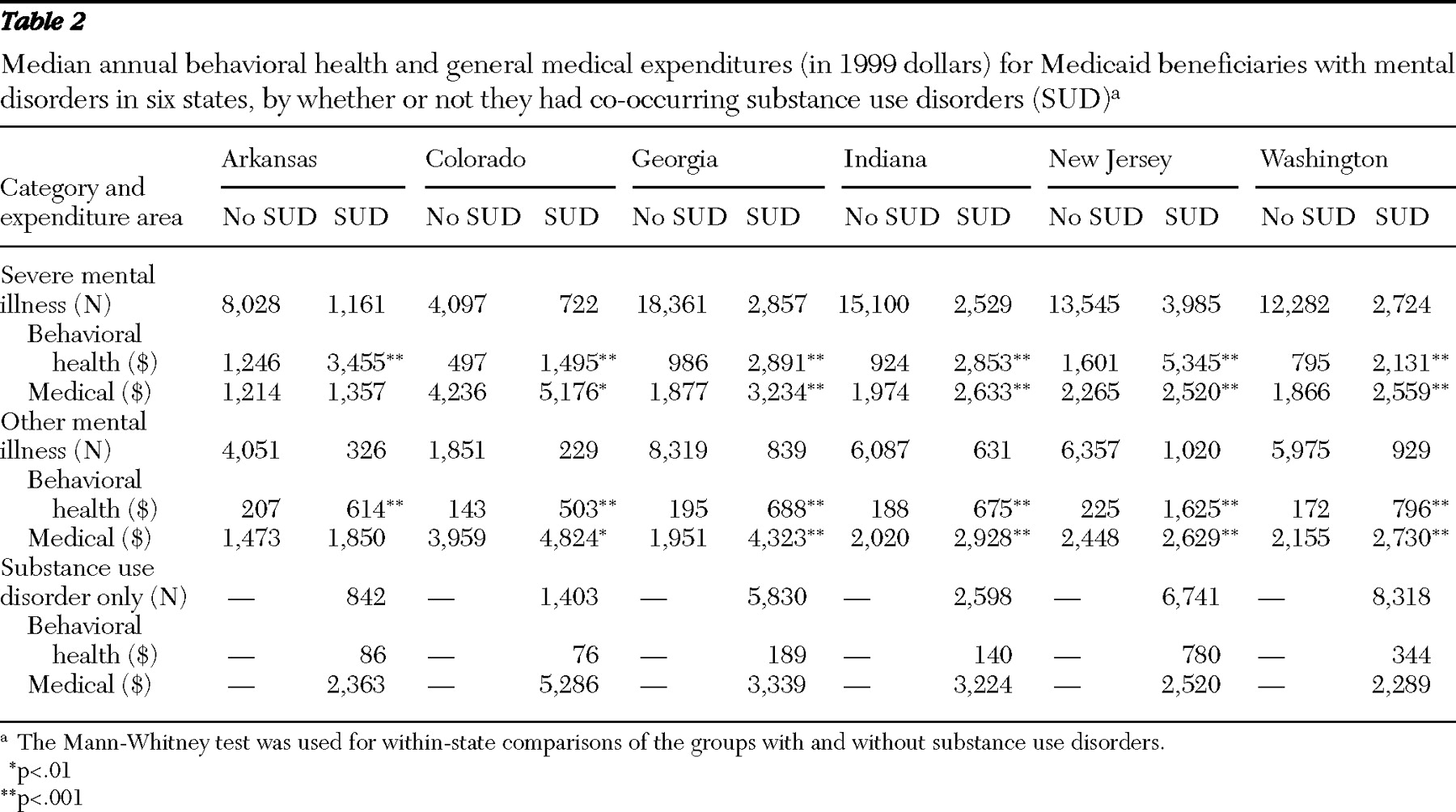
Table 2 shows median behavioral health and medical expenditures for individuals with severe mental illness, other mental illness, and a substance use disorder alone. Total spending varied widely from state to state, but a co-occurring substance use disorder was associated with higher expenditures for behavioral health care and higher total expenditures in all states and with higher medical expenditures in five of the six states. Medical expenditures were generally higher than behavioral health expenditures, except for persons with severe mental illness in Arkansas and New Jersey. In all three diagnostic groups, medical spending was highest in Colorado and behavioral health spending was highest in New Jersey. Other states varied in rank depending on the spending category. For example, Arkansas ranked second in behavioral health spending related to treatment of substance use disorders for beneficiaries with severe mental illness and last in behavioral health spending for beneficiaries with a substance use disorder alone.
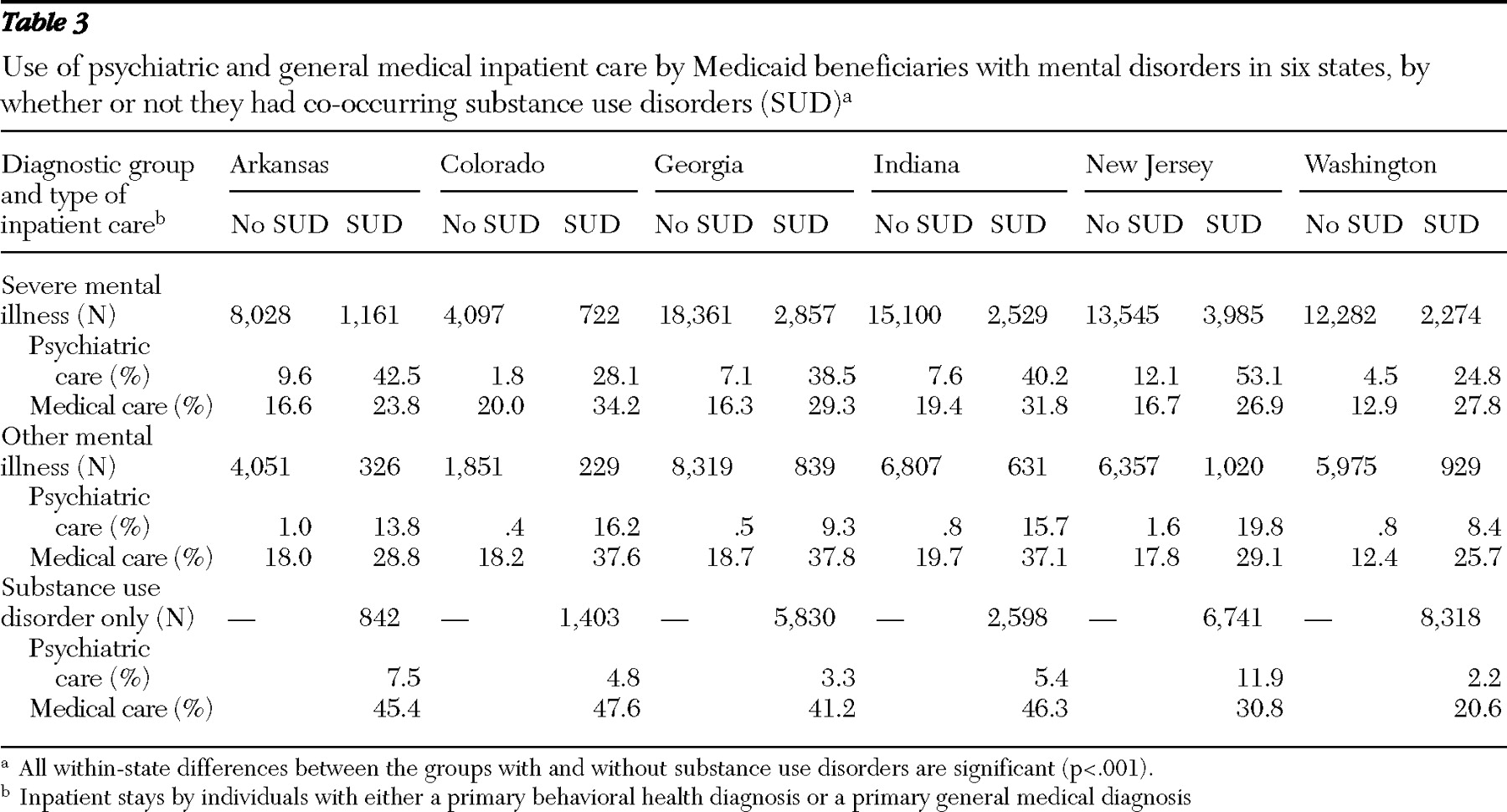
Additional analyses, shown in
Table 3, indicated that in all states diagnoses of substance use disorders were associated with significantly higher rates of hospitalization for inpatient psychiatric care and for inpatient medical care. [A table listing the Ns for the percentages presented in
Table 3 is available as an online supplement at
ps.psychiatryonline.org .] Payments for both types of inpatient treatment were higher for patients with substance use disorders than for those without such disorders in all states (data not shown). Higher expenditures for outpatient medical care were associated with substance use disorders in five states. Expenditures for medication were not significantly associated with substance use disorders.
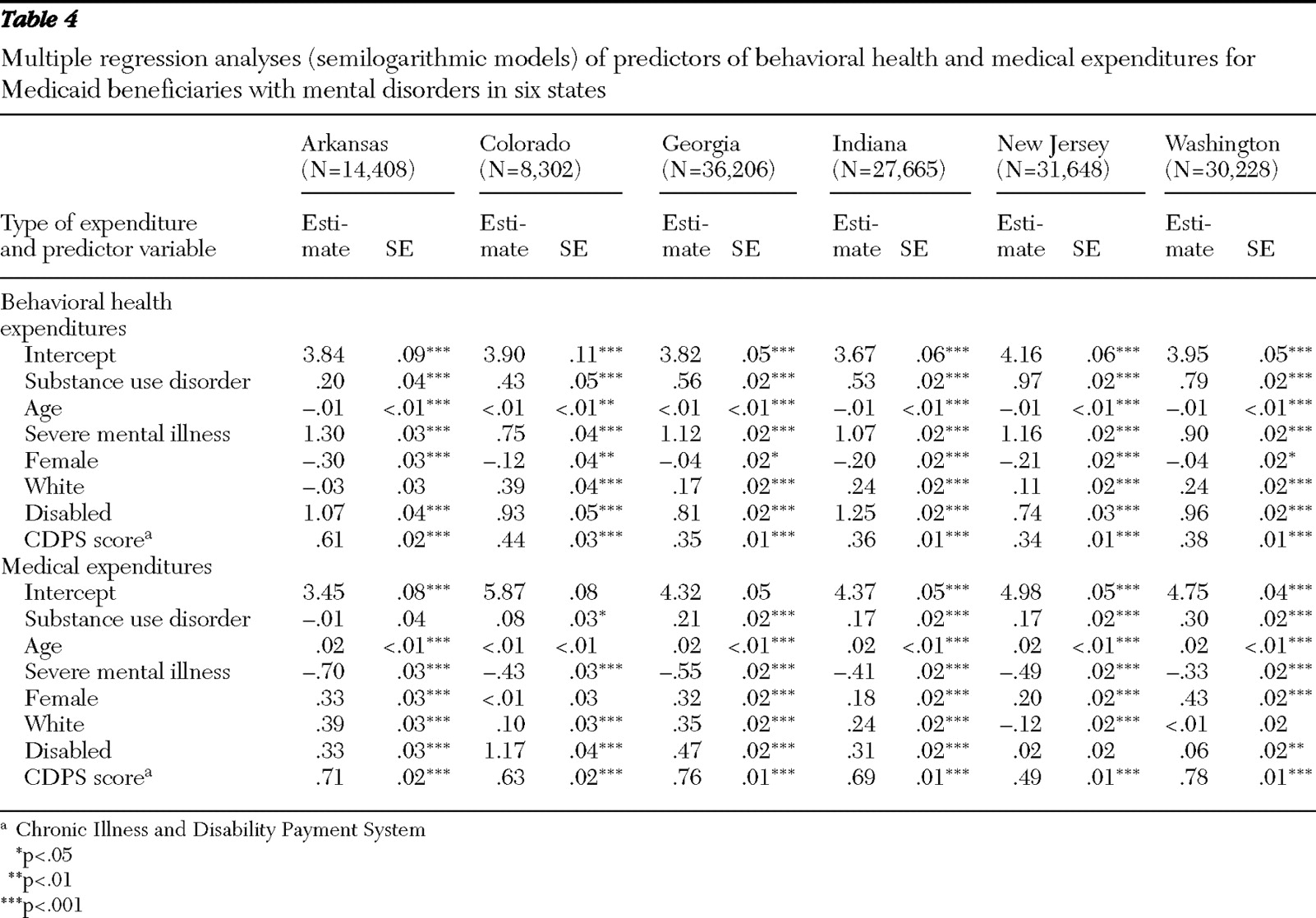
Multiple regression analyses using log-transformed expenditures and adjusting for confounding (
Table 4 ) showed significantly higher behavioral health expenditures in all states and higher medical expenditures in five of six states for individuals with a substance use disorder compared with those who had other behavioral diagnoses. In the model omitting CDPS scores, substance use disorder coefficients were higher and statistically significant in all states. [A table presenting the results of the model omitting CDPS scores is available as an online supplement at
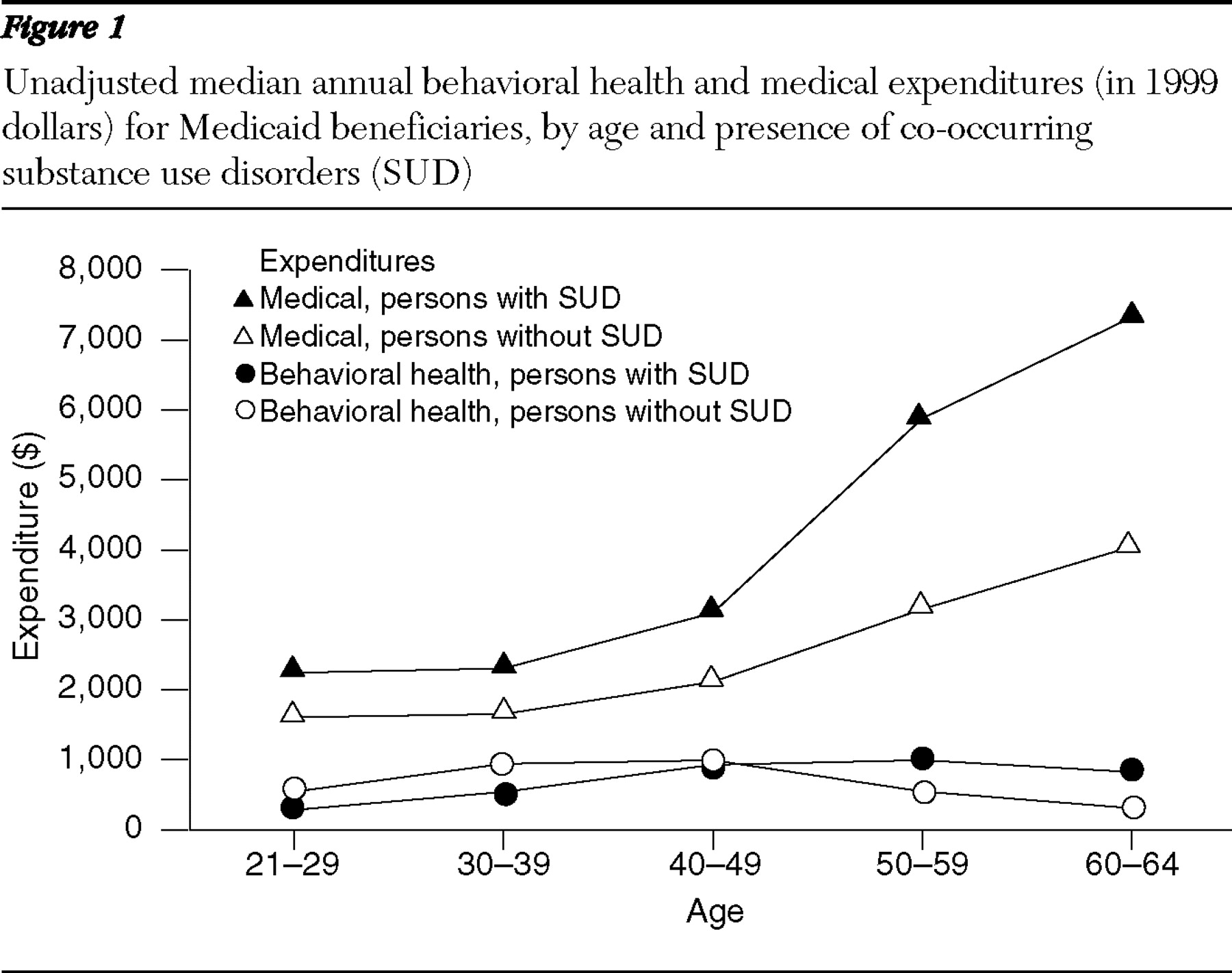
ps.psychiatryonline.org. ] The interaction between age and presence of a substance use disorder (not shown in
Table 4 ) was significant for medical expenditures, indicating that the spending gap between those with and without a substance use disorder increased with age (
Figure 1 ). Average behavioral health expenditures did not change significantly with age.
Overall, models had large sample sizes and estimates were robust to alternative model specifications, including untransformed or truncated outcome variables and discrete-choice ordinal models. Each model passed goodness-of-fit chi square tests. Tests for independence revealed acceptably low correlations among explanatory variables.
Discussion
Medicaid beneficiaries with substance use disorders used more medical care and had higher medical expenditures than beneficiaries with other behavioral health conditions but no substance use diagnosis. Despite wide variation in average spending levels, a consistent pattern of higher expenditures for general medical and behavioral health emerged across the states. When simple unadjusted expenditures for beneficiaries with behavioral health diagnoses are summed, the six study states paid $104 million more for medical care and $105.5 million more for behavioral health care delivered to individuals with substance use diagnoses than for care given to persons with other behavioral health disorders but no substance use diagnosis. These totals do not include Medicaid expenditures for beneficiaries with dual coverage from Medicare or another insurer, nor do they account for expenditures related to undiagnosed substance use disorders. It is unlikely that these missing expenditures would make the proportion attributable to medical care any lower.
Although it is no surprise that medical expenditures increase with age, more research is needed to determine why the growth rate was so much greater for individuals with substance use diagnoses. Possible explanations include higher prevalence of physical illness, the cumulative health impact of long-term substance abuse, greater reluctance among older adults to seek addiction treatment in specialty settings (preferring primary care instead), and more severe chronic disease among mature adults with addictions. Regardless of the explanation, the significantly higher rate of increase in expenditures associated with substance use disorders indicates that older beneficiaries with addictions should be a particular focus of attention. Addressing the medical needs of aging Medicaid beneficiaries with addictions is likely to have a rapidly escalating impact on state budgets as populations age.
Reasons for higher medical expenditures among people with diagnoses of substance use disorders are not completely clear, but the findings offer some hints about potential cost drivers. Differences in the effects of a substance use disorder on medical costs in models with and without CDPS risk adjustment indicate that higher rates of co-occurring physical problems associated with addictions contributed significantly to higher expenditures. More frequent hospitalization coupled with higher rates of ambulatory care-sensitive conditions suggests that beneficiaries with substance use disorders may lack adequate primary and preventive care. By definition, ambulatory care-sensitive conditions represent diagnoses for which primary care can effectively prevent hospitalization. Hospital admissions are a significant driver of expenditures in Medicaid populations, and a recent analysis suggests that the additional investment in outpatient care needed to reduce hospitalizations could be offset by savings (
24 ).
Adjustment for disease burden lowered the impact of substance use disorders on medical expenditures somewhat, but a significant difference remained. One explanation for the remaining difference is that substance abuse and dependence are associated with greater severity of physical illness as well as higher rates of comorbid physical conditions. In a separate study, Ford and colleagues (
6 ) found that substance abuse was associated with more severe medical illness and lower rates of treatment compliance.
Reliance on Medicaid claims limited our analysis in some ways. Claims-based diagnoses may be less accurate than those typically developed with the structured tools and processes used in other types of research. It is likely that substance use disorders were underdiagnosed in our sample, and persons identified with claims-based diagnoses of substance use disorders may represent a subgroup of beneficiaries who have more severe addictions or are more likely to seek treatment. If those identified with diagnoses of substance use disorders have more severe addictions, our analysis would overestimate average individual expenditures somewhat while underestimating the total impact of substance use disorders on Medicaid budgets. Substance use disorders are not routinely detected in primary care settings or community mental health care settings, perhaps because of the extra burden of recording substance use diagnoses on a claim form, without financial incentive in most cases. Although we did not find differences between beneficiaries enrolled in managed care and fee-for-service plans, it should be noted that managed care firms receiving a capitated payment have weaker incentives to report services accurately. For these reasons and because beneficiaries with Medicare or other insurance were excluded from the analysis because of incomplete claims histories, we consider these expenditure estimates to be a particularly conservative measure of the impact of substance use disorders on total Medicaid budgets.
The wide variation across states in the percentage of beneficiaries with substance use disorders and in total expenditures is not easily explained by differences in Medicaid policy, managed care penetration, or overall state spending for addictions or mental health treatment. However, New Jersey and Washington, the states with the highest percentage of beneficiaries with diagnoses of substance use disorders, also had the highest per capita direct state spending for addictions treatment, suggesting a possible association between spending and recognition of substance abuse or dependence. Further exploration of the reasons for state variation in spending is beyond the scope of data available for this study.
One alternate explanation for our findings is that more generous reimbursement or simply fewer administrative restrictions for medical care encourages cost shifting from behavioral health to medical billing codes. The existence or extent of this problem cannot be measured with the study data; however, it seems unlikely to be the sole explanation for the consistently observed differences in expenditures, hospitalizations, and rates of ambulatory care-sensitive conditions across the study states. This form of cost shifting obscures the overall impact of addiction on Medicaid programs, making it more difficult to recognize and effectively address the issue.
Conclusions
Substance use disorders were found to be associated with significantly higher Medicaid expenditures for treatment of physical health problems among beneficiaries with behavioral health disorders. Although additional work is needed to understand the underlying reasons for higher medical expenditures, our analysis suggests that significant improvements could be made by targeting the medical needs of beneficiaries with substance use disorders. Focusing on ambulatory care-sensitive conditions may reduce hospital admissions. A variety of other approaches have been suggested to improve the quality or reduce the cost of health care among persons with behavioral health disorders (
25,
26,
27 ). Our findings suggest that interventions for aging populations may be particularly important for improving health and managing Medicaid expenditures.
Acknowledgments and disclosures
Preparation of this paper was assisted by grant 049822from the Robert Wood Johnson Foundation Substance Abuse Policy Research Program.
The authors report no competing interests.