Ensuring equitable access to needed mental health services is a national policy priority (
1,
2 ). Assertive community treatment (ACT) programs provide needed services for individuals with serious mental illnesses. Programs are designed to enhance clients' functional independence, facilitate community reintegration, and prevent or delay rehospitalization. Researchers have examined ACT programs with regard to their costs, adaptability, and efficacy. Multiple literature reviews indicate that receipt of ACT services is associated with reduced inpatient psychiatric utilization and with greater housing stability, client satisfaction, and quality of life (
3,
4,
5 ). In general, program costs are comparable with those of other types of community-based care (
6 ), and ACT programs have been found to be cost-effective when targeted for individuals who have had high hospital use (
7,
8,
9,
10 ) and when the programs maintain fidelity to the treatment model (
9 ). Indeed, ACT is an accepted evidence-based practice for patients with schizophrenia (
11 ).
Although there is recognition that ACT services are frequently unavailable (
5 ), we know of no studies that have examined receipt of ACT services among individuals who were eligible for them yet not already receiving them. In the Veterans Affairs (VA) health system such research can be conducted, given the comprehensive national VA administrative data regarding diagnoses and services utilization. Research examining these issues may inform policy efforts to ensure access to needed mental health services.
Each year in the national VA health system, over 200,000 patients have diagnoses of schizophrenia, bipolar disorder, or other psychoses. Most of these veterans have limited incomes or have disabilities related to their military service (
12 ). Veterans with serious mental illness who are at high risk of psychiatric rehospitalization are eligible for the VA's ACT program, which is called mental health intensive case management (
13 ). At the end of fiscal year (FY) 2003, 63 VA ACT teams were fully operational (with data for at least ten clients), 4,108 patients were enrolled in these programs, and program expenditures were $27 million. Across sites, the average Global Assessment of Function score for enrolled patients was 39.5±5.5 out of 100, with lower scores indicating poorer functioning (
13 ). Essential components of VA ACT programs include an intensive interdisciplinary team approach to treatments delivered in home and community settings, high staff-to-client ratios, and fixed team responsibility for total patient care (
2 ).
Most ACT programs in the United States are based in urban areas, where there are greater concentrations of health services, community resources, and potential clients. Although there are ACT programs in some rural areas, rural ACT programs have had difficulty with model fidelity, partly because of staff turnover, professional isolation, and lack of ongoing training (
14,
15 ).
This study examined VA ACT services receipt, or "initiation," in FY 2004 among VA patients who met the VA ACT program's eligibility criteria in FY 2003 yet did not receive ACT services in FY 2001–FY 2003. We describe patterns of services initiation, and we evaluate patient and ACT program characteristics as predictors of initiation. Services initiation was assessed in terms of receipt of any VA mental health intensive case management services. Also, we assessed sustained use of services (defined as having at least .8 visits per week for the rest of the year after the first visit).
Initiation of ACT services involves both provider and client behaviors. For example, in the course of treatment encounters, providers may request an ACT consultation. ACT teams then contact potential clients to confirm eligibility and assess willingness to participate.
We considered two dimensions of access that may influence this process: geographic accessibility and provider resource availability (
16 ). Studies indicate that greater distance from VA health care facilities and less inpatient bed availability limit the volume of health system services utilization and the continuity of care among VA patients with mental illness (
17,
18 ). Given the ACT program's emphasis on intensive local delivery of services, we hypothesized that veterans living farther from teams and those whose nearest team had fewer open slots would be less likely to receive ACT services.
Methods
Design
Among all patients in the VA health system who were eligible for and not already receiving ACT services, we examined services initiation in a one-year period.
Sample
Using the VA's National Psychosis Registry, we identified all 6,553 VA patients who were eligible for mental health intensive case management services in FY 2004 and had not received these services in the prior three years (FY 2001–FY 2003). Using standard VA program eligibility criteria, we assessed patient eligibility for ACT services on the basis of diagnosis and hospitalization history (
2 ). Individuals were considered eligible if they had received a diagnosis of schizophrenia (
International Classification of Diseases, Ninth Revision [
ICD-9 ] diagnoses 295.0–295.4 and 295.6–295.9), bipolar disorder (296.0–296.1 and 296.4–296.8), or other psychoses (297.0–297.3, 297.8–297.9, 298.0–298.4, and 298.8–298.9) at some point during FY 2001–FY 2003 and had at least three inpatient psychiatric stays or more than 30 inpatient psychiatric days in FY 2003. After exclusion of 13 patients with missing data, the analytic sample included 6,540 patients.
Measures
Services initiation was indicated by use of ACT services in FY 2004 (October 1, 2003, through September 30, 2004). In sensitivity analyses, we examined initiation of sustained ACT contacts, for which we used a dichotomous measure of whether patients had at least .8 ACT visit per week, prorated for time after initial ACT services utilization. This definition of sustained use was derived from VA criteria used to identify current ACT patients as qualifying for "complex class" status for purposes of health system resource allocation. Patients are eligible for this status when they have had at least 41 ACT visits in a fiscal year (
13 ).
In selecting model covariates, we applied the Andersen model of predisposing, enabling, and need factors that affect utilization (
19 ). This model provides a helpful framework for conceptualizing factors affecting health services utilization. Predisposing factors included age as of the start of FY 2004, gender, marital status (coded as married or other), and race and ethnicity (coded as white, minority, or unknown).
Enabling factors included military service-connected disability status, homelessness (a negative enabling factor), available slots with the nearest ACT team, presence of an ACT team at the VA medical center where patients received the majority of their VA health care, and proximity of the nearest ACT team. Service-connected disability status was identified from encounter data and the VA's compensation and pension file. Patients who have disabilities as a result of their military service have priority eligibility for VA health services. Service connection was measured with a dichotomous indicator of having or not having any service-connected disability. Homelessness was indicated by a variable in the VA's outpatient procedure data,
ICD-9 diagnosis code V60.0, or by services utilization in specific outpatient clinics or inpatient "bed sections," which are similar to non-VA inpatient wards or departments (
17 ).
We identified the locations of ACT teams and the number of available slots at each ACT site in FY 2003 (
13 ). Open slots at the nearest team were calculated as the difference between the ACT team's maximum number of patients (based on a maximum caseload ratio of 15 clients per clinical full-time employee [2]) and its actual number of patients in FY 2003.
As in previous studies (
17,
18,
20 ), we assessed distance to the nearest facility with a VA ACT team. Our measure was straight-line miles from the location of the center of the population ("population centroid") of the patient's zip code of residence. Straight-line distance may be a reasonable proxy for travel time (
21 ). We also assessed whether there was an ACT team on site at the VA facility where the patient's last inpatient psychiatric stay occurred.
Need factors included primary psychiatric diagnosis category, substance use disorder diagnosis, and total psychiatric inpatient days in FY 2003. Primary psychiatric diagnosis category was assigned on the basis of diagnosis category (schizophrenia, bipolar disorders, or other psychoses) recorded most frequently in VA encounters in FY 2003 or, if none were recorded in FY 2003, then in FY 2002 or FY 2001. Ties were resolved with the following ordering: schizophrenia, bipolar disorder, then other psychoses (
18 ). Substance abuse or dependence was indicated by diagnosis codes 303.x, 304.x, or 305.x (
12 ). The total psychiatric inpatient days during FY 2003 was calculated from VA inpatient records.
Data analysis
We estimated multivariate logistic models of VA ACT services initiation and sustained utilization. The method of generalized estimating equations (GEE) with a logistic link was used to estimate the model (
22 ). GEE was used to adjust standard error estimates for potential correlation of VA ACT use among patients near a particular VA ACT team. The correlation structure was specified as compound symmetry.
In sensitivity analyses, we examined potential nonlinear (that is, not strictly proportional) relationships between distance from teams and services initiation, using quadratic distance effects, Loess curve assessment (
23 ), and spline analysis. Finally, we evaluated predictors of ACT services initiation among eligible patients who resided within 60 miles of teams, because one hour's driving time has been proposed as a practicable limit for teams.
All analyses were completed with SAS, version 9.1. This project was approved by the institutional review board at the Ann Arbor VA medical center.
Results
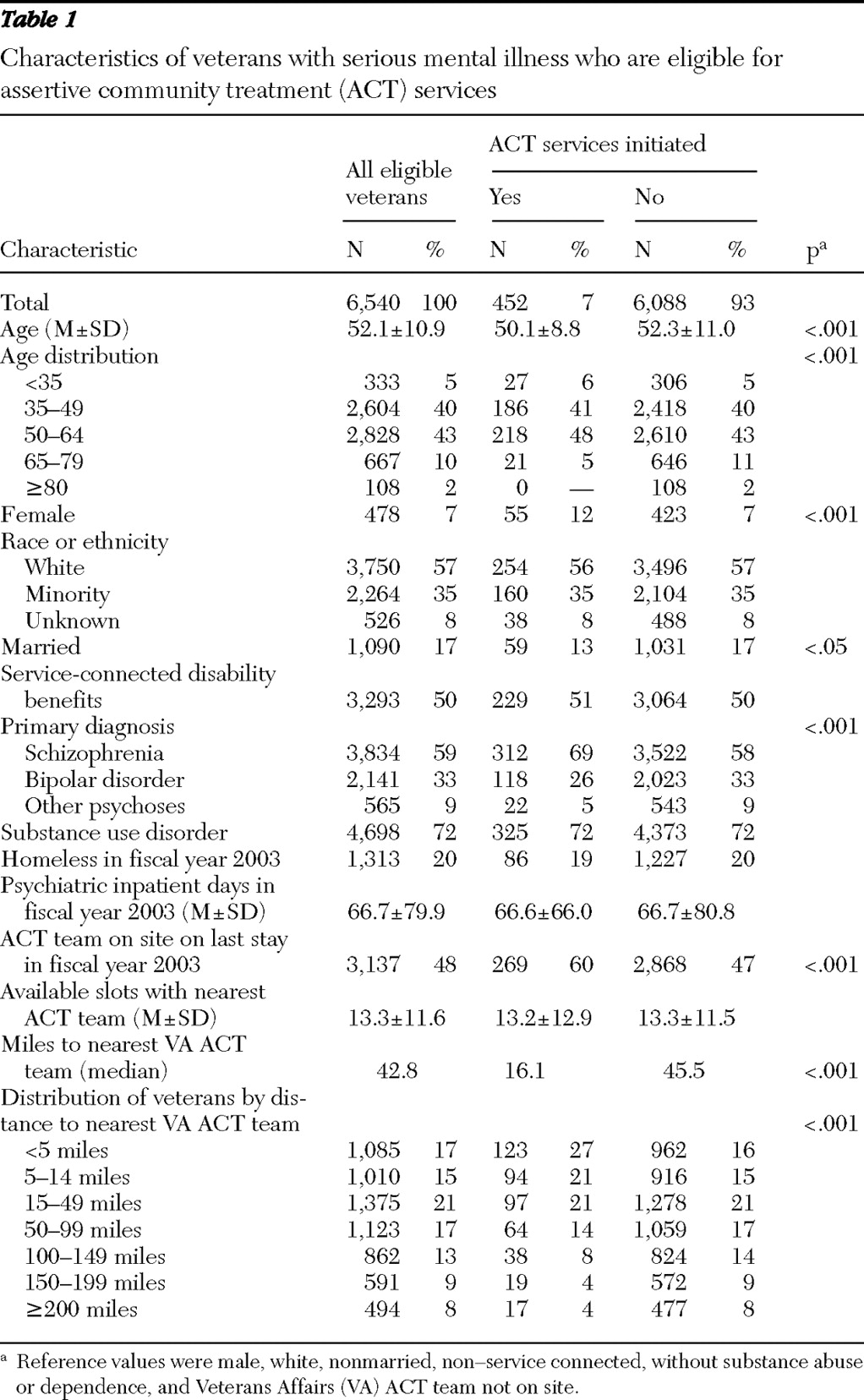
Among the 6,540 veterans in our analyses, all of whom met program eligibility criteria and had not received VA ACT services in the prior three years, 452 (7%) received ACT services in FY 2004, with 207 persons (3%) meeting criteria for sustained receipt of services. In bivariate analyses (
Table 1 ), individuals who received services were younger and more likely to be female and unmarried, to have schizophrenia, to have had their most recent inpatient stay at a VA medical center that had an ACT team, and to reside nearer to a team. Patients aged 50 to 64 were most likely to receive ACT services. Receipt of ACT services was not associated with the number of open slots with the nearest ACT team.
Overall, 3,470 patients (53%) lived within 50 miles of an ACT team, whereas 862 patients (13%) lived between 100 and 149 miles from a team and 1,085 patients (17%) lived at least 150 miles from a VA ACT team. The median distance to the nearest facility with a VA ACT team was 43 miles. Median distance was 16 miles among patients who received ACT services in FY 2004, compared with 46 miles among those who did not receive these services.
Similar results were observed with regard to receipt of sustained ACT services use. Patients who received sustained ACT services in FY 2004 were more likely to be younger, to be female, to reside nearer to facilities with ACT teams, and to have an ACT team at their local VA medical center. In addition, they were more likely to have military service-connected disabilities and less likely to have been homeless.
Loess curve analysis was used to examine odds of initiating ACT services, by distance from the nearest team. This nonparametric method produces smoothed locally weighted regression estimates. This analysis indicated that the odds of initiating ACT services were greatest among patients living nearest to teams. Odds fell as distance increased, with the marginal effects of distance being greatest in the first 30 miles. The slope fell relatively slightly from 30 to about 100 miles, beyond which the slope fell more steeply.
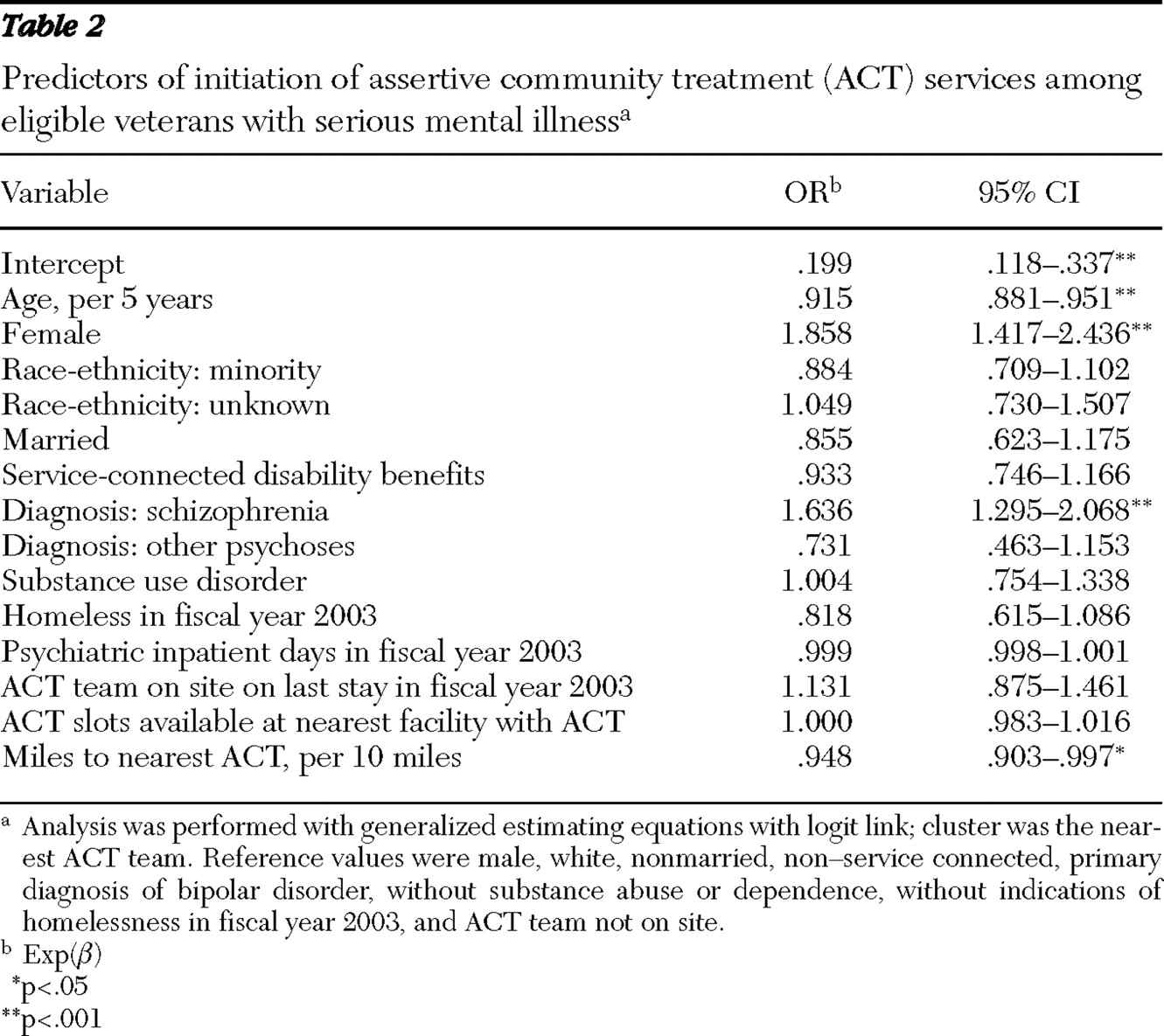
Multivariate GEE analyses indicated that patients were more likely to initiate services if they were female (odds ratio [OR]=1.86) and if their primary psychiatric diagnosis was schizophrenia (OR=1.64, compared with bipolar disorder) (
Table 2 ). Older age and greater distance from treatment teams were associated with lower likelihood of receiving ACT services (OR=.92 per five years in age; OR=.95 per ten miles).
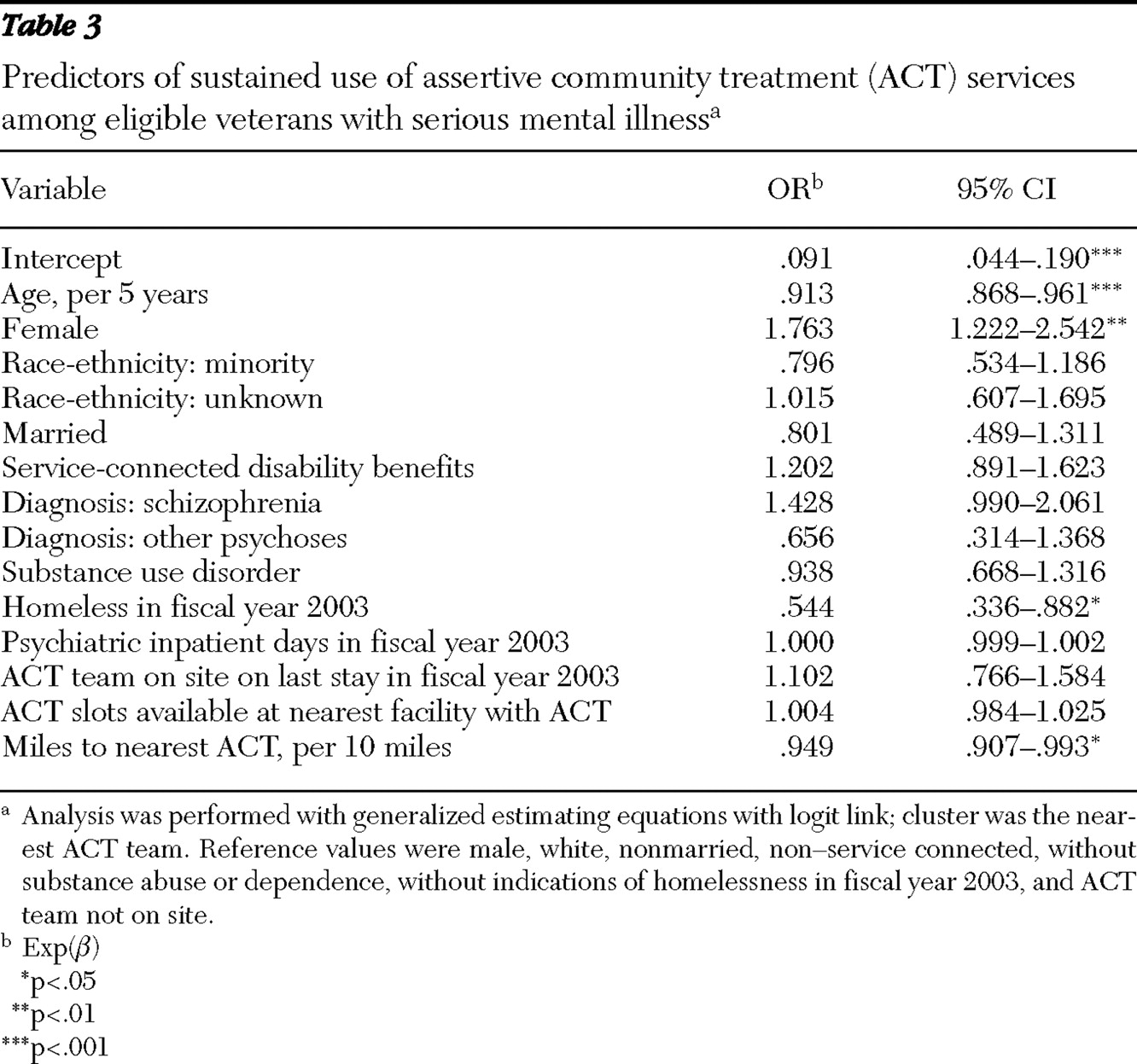
Similar results were observed regarding sustained receipt of ACT services (
Table 3 ). However, in those analyses patients who were homeless were less likely to have sustained use of services (OR=.54), and diagnosis type was not significant.
In sensitivity analyses limited to individuals living within 60 miles of a team (N=3,377), 9% of eligible patients (331 individuals) received ACT services. Individuals were significantly less likely to receive services if they were older (OR=.91 per five years in age) or lived farther from teams (OR=.84 per ten miles). They were significantly more likely to receive these services if they were female (OR=1.83) or if their primary psychiatric diagnosis was schizophrenia (OR=1.72). Estimates of sustained ACT use (observed among 4%, or 147 individuals, of eligible patients living within 60 miles of a team) indicated similar associations; however, neither distance nor psychiatric diagnosis category was significant, and homelessness was associated with lower likelihood of sustained use (OR=.51).
Multivariate models provided additional evidence of a nonlinear relationship between distance and ACT services initiation. On the basis of the Loess curve analysis, we tested a two-knot spline analysis in which line segments were joined together at 30 and 100 miles. Results indicated a significant shift in the relationship at 30 miles, with a flattening of the slope past 30 miles.
Discussion
To our knowledge, this study is the first to examine initiation of ACT services among eligible persons. Among patients who were eligible for yet not already receiving VA ACT services, most received no ACT services in the following year (6,088 out of 6,540, or 93%). And virtually all patients did not receive sustained ACT services (6,333 out of 6,540, or 97%).
In multivariate analyses, we found that patients were more likely to receive ACT services if they had schizophrenia or were older or female. This may reflect more acute need for ACT services among patients with schizophrenia. We note that in bivariate assessments, individuals aged 50 to 64 were most likely to receive ACT services, whereas those aged 65 and older were less likely. It is unclear whether female patients' greater likelihood of using VA ACT services reflects greater need for ACT services among female patients, a higher perceived acceptability of ACT among female patients, a higher likelihood that female patients are identified by providers as needing ACT, or a combination of these factors. Further research is needed to understand these factors in relation to ACT services initiation.
Few studies have examined associations between use of ACT services and ACT program characteristics (
24 ). We examined ACT providers' availability (measured as the number of slots open with the nearest team) and geographic accessibility. We did not find support for the hypothesis that provider availability was associated with services initiation. However, the hypothesis that geographic accessibility barriers influence ACT program initiation was supported. Veterans living farther from VA ACT teams were less likely to receive services, and the marginal effects of distance were most pronounced in the first 30 miles.
These findings are consistent with previous work documenting the impact of the "friction of space" on health services utilization (
17,
18 ). Because of greater travel burdens, providers may be less willing to enroll patients who are farther away, and remote patients may be less willing to receive ACT services from more distant providers. However, it is possible that the observed associations could reflect other factors, such as unmeasured differences in need for services among patients living farther from ACT teams.
Prior studies have found greater residential mobility among VA patients with schizophrenia or bipolar disorder compared with other patients; homelessness is also associated with greater mobility (
20 ). In this study, patients who were homeless were less likely to receive sustained ACT services. We conclude that ACT engagement is less enduring among individuals who are not stably housed.
As the locus of VA psychiatric services has shifted substantially from institutional to outpatient settings, patients with serious mental illness are increasingly reliant on programs such as ACT. Unfortunately, most patients eligible for ACT who were not already receiving ACT services did not receive them. These findings validate concerns regarding access to ACT services (
5,
25 ).
Study findings suggest that geographic accessibility barriers may affect health services utilization, even in the case where providers, rather than patients, are doing the traveling. Given limited time and resources, ACT teams may be more likely to provide services to eligible patients who live nearby than to those living farther away.
Major strengths of this analysis include the large study population (including all VA patients who met program eligibility criteria and who were not already receiving VA ACT services) and the use of comprehensive health system diagnosis and utilization data to assess program eligibility and services initiation. However, administrative data are subject to data entry errors and missing data problems. Furthermore, although they provide objective measures of program eligibility, in terms of diagnosis and high psychiatric hospitalization history, they may be imperfect indicators of actual need for ACT services or of recognition of need for services. We note that patients with serious mental illness may be less aware of co-occurring general medical conditions than other patients (
26 ). For example, it was not possible in this study to include independent measures of mental health functioning. Also, despite national VA directives, individual ACT programs may use their own criteria for allocating program resources, and it was not possible in this study to assess local program criteria.
Furthermore, study data did not include indicators of non-VA services utilization. In general, there is conflicting evidence as to whether VA patients living in remote areas are more likely to receive non-VA health services (
27,
28 ). We believe that persons included in the study—all of whom met criteria for high VA hospital use—were unlikely to have received ACT services from non-VA providers. Whereas we assessed ACT services initiation in a single fiscal year, future studies could instead follow patients from the time when they first met program eligibility criteria.
Finally, it is unclear to what extent our study findings may be generalized to other populations with serious mental illness or to ACT programs in other settings. Many ACT-eligible patients appear to be underserved in the VA health system, which is the largest integrated health system in the United States. Access to ACT may be equally problematic in state public mental health systems and in other settings.
Conclusions
This report documents the need to enhance ACT program access. Focused efforts are needed to address the care needs of all patients with serious mental illness, particularly those who reside in remote locations. And further research is needed to understand provider and patient decision making regarding ACT services initiation. In the course of psychiatric admissions for individuals with serious mental illness, program eligibility and enrollment status should be evaluated routinely. Policy directions include increasing the number and size of ACT programs, improving outreach for more patients living in more remote areas, and developing programs to meet the needs of patients who live in those areas. These needs include enhancement of remote case management and telepsychiatry capacities and enhancement of mental health resources in community-based outpatient clinics, as well as improving our understanding of why ACT services fail to be delivered to eligible patients.
Acknowledgments and disclosures
This study was supported by contracts VA MRP-03-320 and VA IIR-06-115-1, by the Veterans Integrated Services Network 5 VA Capitol Network Mental Illness Research, Education and Clinical Center, and by the VA Serious Mental Illness Treatment Research and Evaluation Center.
The authors report no competing interests.