Studies of the population with serious mental illness (that is, schizophrenia or major affective disorder) suggest that about 50% have general medical conditions (
1,
2 ) that are largely undiagnosed and untreated and may cause or exacerbate psychiatric symptoms (
3 ). Increasingly, research suggests that persons with serious mental illness have a greater risk than the general population of contracting and transmitting infectious diseases, such as HIV, hepatitis B, and hepatitis C (
4,
5,
6,
7 ) and that the costs associated with their treatment are higher than those for persons without mental illness (
8 ). A retrospective study of patients in state psychiatric hospitals found that the prevalence of hepatitis B (23.9%) and hepatitis C (21.5%) was significantly higher than that found in the general U.S. population (
9 ), where the prevalence of hepatitis B is 5% (
www.hepb.org ) and the prevalence of hepatitis C is 1.8% (
10 ). Estimates of HIV in the population with serious mental illness range from 4% to 23%, compared with a range of .4% to .6% in the general population (
5,
11 ). The prevalence of diabetes among persons with serious mental illness is reported to be 11% (
12,
13 ), compared with 7% in the general population (
www.diabetes.niddk.nih.gov ).
Despite high rates of infectious and metabolic conditions among individuals with serious mental illness, screening for these conditions does not occur routinely in psychiatric settings. This brief report explores the prevalence of metabolic and infectious conditions among patients admitted to acute care psychiatric units of a tertiary care hospital system. For this study, patients' leftover blood samples that were originally drawn for other laboratory tests were given an anonymous identification number and tested for various metabolic syndromes and infectious diseases. This information was compared with abstracted data from patients' medical records (also given an anonymous identification number) in order to determine the prevalence of these disorders in this sample. This report also discusses the potential benefits of routine screening in psychiatric inpatient settings.
Methods
The study sites were two inpatient psychiatric units that were part of the University of Pennsylvania Health System. Both units used a single clinical laboratory system for performing blood testing. A total of 656 adult psychiatric patients were admitted over 18 months (2003–2005). The study sample included 588 patients for whom blood samples were available.
An observational-naturalistic study design was used simulate universal screening in order to document evidence of the magnitude and type of metabolic disorders and infectious diseases in the sample. Our hypothesis was that a high percentage of previously undetected (or unrecorded) metabolic or infectious diseases known to be prevalent in this population would be found among patients in the study cohort. Our study compared abstracted medical records (coded with an anonymous identification number) with the results of laboratory blood tests (also coded with an anonymous identification number) that were run for the purposes of this study to determine the prevalence of these disorders.
The study was approved by the institutional review board at the University of Pennsylvania, which provided oversight of the study. Fasting blood samples for the majority of the study cohort were drawn routinely from patients after admission; however, universal screening for the conditions of interest was not routinely employed. Laboratory orders were based on the clinical judgment of treating physicians. Investigators did not interact with members of the treatment team regarding laboratory orders or test results. All laboratory analyses were performed using manufacturer recommended methods.
The criteria for a clinically positive test result for various metabolic syndromes were as follows: glucose levels over 140 mg/dl, cholesterol levels over 180 mg/dl, and triglyceride levels over 180 mg/dl. The precision of the hepatitis B surface antibody test, hepatitis C antibody test, and HIV antibody test is 5%, 20%, and 20%, respectively. Positive hepatitis C and HIV results were confirmed by Western blots. The total number of blood test results obtained for each patient in this study depended on the amount of blood that was left over after the laboratory ran physician-ordered assays and on whether the blood samples had already been tested for any of the metabolic syndromes and infectious diseases that our study was examining—that is, if enough blood was available, all six metabolic and infectious diseases would be tested for (either by request of the treating physician or study investigators) to simulate universal screening.
Admission reports were obtained daily from central scheduling. In the event that patients did not have orders for tests of interest in this study, their blood samples were intercepted before they were discarded by the clinical laboratory. The samples were then blinded with a study identification number and sent for analysis of the remaining tests using procedures developed by Brady and colleagues (
14 ) for detecting HIV in an emergency room sample at University of Pennsylvania Health System. Clinical data were abstracted from a review of admission histories, physical examinations, standardized nursing assessment forms, and discharge summaries, which were supplemented by electronic records of all inpatient and outpatient services rendered in the University of Pennsylvania Health System for one year before admission. Abstracted medical record data were paired with results of laboratory tests obtained by the study team using the anonymous study identification number. Analysis involved calculation of the prevalence of metabolic disorders found by this study and by physician-ordered tests. The percentage of each undetected disorder was constructed by calculating the number of cases missed by the treatment team (clinical record review) over the number of positive results found by physician-ordered and study-ordered laboratory blood tests.
Results
The mean±SD age of the 588 patients was 42±14 years; 305 (52%) were female. A total of 180 (31%) were white, 370 (63%) were African American, 18 (3%) were Hispanic, and nine (2%) were of another race or ethnicity. A total of 359 persons (61%) had a co-occurring lifetime disorder of drug abuse, and 335 (57%) had a diagnosis of alcohol use disorder. Among those with drug dependence, cocaine dependence was the most common (N=159, 27%). With respect to psychiatric diagnoses at the time of admission, 329 (56%) had a major depressive disorder and 194 (33%) had a schizophrenia spectrum disorder. Height and weight measured on admission showed that 347 patients (59%) had a body mass index (BMI) of 25 or higher and that 200 (34%) had a BMI greater than 30.
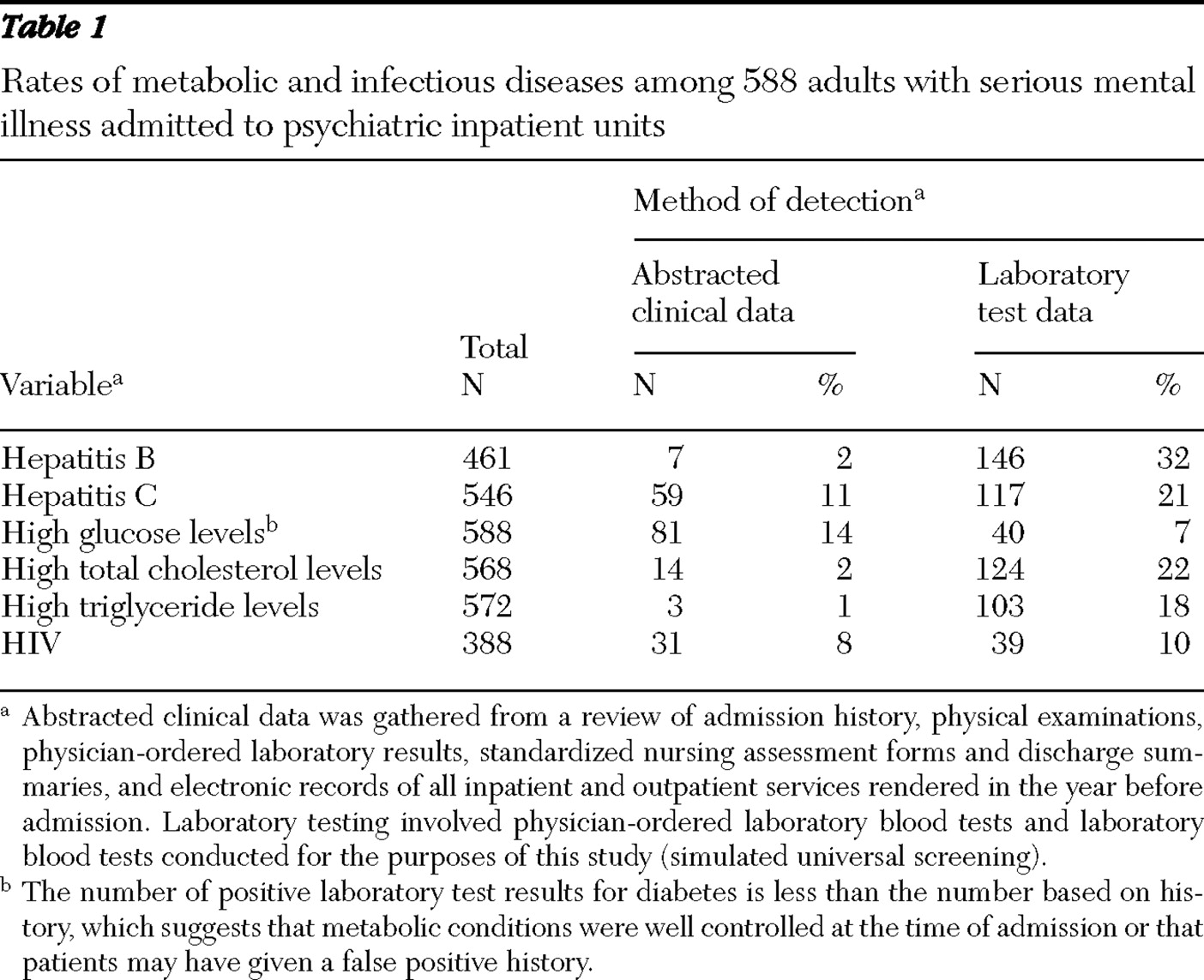
Table 1 shows the positive results for the metabolic and infectious diseases, as measured by reviewing medical records and by laboratory findings. Laboratory results showed that 146 patients (32%) had hepatitis B antibodies, 117 (21%) had hepatitis C antibodies, and 39 (10%) had HIV antibodies. Glucose levels higher than 140 mg/dL were found among 41 (7%) patients, total cholesterol levels greater than 180 mg/dL were found among 124 patients (22%), and triglyceride levels higher than 180mg/dL were found among 103 (18%) patients.
The treatment team missed a considerable proportion of patients with an infectious disease and had mixed results in the detection of metabolic disorders. The number of positive cases identified by the study team that were not identified by clinical history or clinician-ordered tests was 139 (95%) for hepatitis B, 58 (50%) for hepatitis C, and eight (21%) for HIV. For metabolic disorders, the interpretation of missed cases was somewhat complicated, because many of the patients with medical records indicating the presence of diabetes or high cholesterol did not have positive laboratory findings according to our study findings. For example, the clinical history of 81 patients (14%) indicated that they had diabetes, whereas only 40 (7%) of all tested patients had positive glucose tests according to laboratory findings. The discrepancy was likely due to the fact that many of the patients had their conditions under control at the time of admission. However, of the 40 patients who did test positive for high glucose levels, seven patients (18%) did not have a written clinical history of diabetes and their physicians had not ordered glucose testing. For cholesterol, 110 (89%) of those with positive tests were missed by physicians, and 100 (97%) with elevated triglyceride levels were undetected.
Discussion
Given the high levels of metabolic and infectious disease found among persons with mental illness, psychiatric inpatient settings appear to be a good place to consider universal screening for the conditions reported here, provided that such screening is integrated with a workable system to provide follow-up medical care. The inpatient stay provides a unique opportunity to be proactive in detecting common medical conditions, which may have gone unnoticed as a result of inadequate primary health care and fragmented health care financing. Such a financing system provides a disincentive to providing combined general medical-psychiatric treatment. However, hospitals can be an ideal place to provide such treatment, because they have an existing infrastructure to conduct tests, review results, provide educational interventions, and offer referrals for treatment after discharge.
Why then isn't screening for these conditions done routinely? One likely reason is that the focus of care in inpatient psychiatric units is on stabilizing acute exacerbations of psychiatric illness. The result can be a missed opportunity to attend to medical conditions that may not be directly related to the psychiatric stay but that add substantial morbidity. Another is that physicians may perceive that individuals with serious mental illness have poor adherence to medical regimens and that identification of the problem will not lead to patients' being active in addressing the problem. Both of these reasons can be challenged, because failure to identify conditions that are treatable can lead to higher future costs (
8 ) and because sufficient evidence exists that persons with serious mental illness have similar if not higher levels of adherence to medical regimes, compared with other groups of individuals with chronic conditions (
15 ).
A further reason for the lack of routine testing may be the guidelines provided by the U.S. Preventive Services Task Force, which do not support routine testing for asymptomatic hepatitis B or hepatitis C, asymptomatic type II diabetes, and impaired glucose functioning. They do, however, strongly recommend universal testing for HIV and lipid disorders (
www.ahrq.gov ). A more rigorous approach to testing the population with serious mental illness may be necessary, on the basis of the high rates of metabolic and infectious diseases found this study.
Needless to say, universal screening is not a solution to the problem identified in this study, although it may be a necessary first step. To increase the effectiveness of care, universal screening should be linked to well-integrated, accessible systems of medical information and general medical-psychiatric care. For example, patients who have been previously found to be infected with HIV or hepatitis C need not be screened repeatedly for these illnesses. Finally, the cost of universal screening must be examined and aligned with improvements in general medical and psychiatric outcomes for patients with serious mental illnesses. Mental health carve-outs that offer per diem reimbursements for inpatient psychiatric care, as was the case for the units in this study, provide disincentives for addressing all but the most acute medical problems during psychiatric hospitalization.
There are three study limitations related to our prevalence estimates that should be mentioned. The first is that the prevalence rates may not be generalizable to other populations because one of the psychiatric units had psychiatric patients with current drug and alcohol use disorders, where the infectious disease rates are known to be very high, and because blood draws may not have been done after patients had fasted, which could lead to an overestimate of some metabolic disorders. The second limitation is that patients may have reported information regarding some conditions, although physicians may not have recorded it. This might explain why, in some cases, testing was not ordered. This, however, should not be the case for ascertainment of metabolic status, which requires repeated testing for appropriate medical care. Finally, we may have overestimated the cholesterol problem in our study population, because the American Heart Association is currently saying that cholesterol levels under 200 mg/dl are desirable, whereas we used a more stringent criterion of 180 mg/dl.
Conclusions
This study suggests that the documented awareness of metabolic and infectious diseases in psychiatric inpatient records falls short of the prevalence of these illnesses among patients being treated for acute psychiatric problems. Without routine testing, psychiatric physicians and nurses cannot consider the full extent of treatment-disease interactions among their inpatients (for example, use of medications with hepatic or metabolic side effects). Thus the public health consequences of coexisting medical and psychiatric diseases are not being addressed in acute psychiatric settings, and an important opportunity for individual patient education, health promotion, and referral for medical care is being missed (
16 ). Future studies should be done to calculate the benefit of universal screening and the effectiveness of treatment on reducing costs.
Acknowledgments and disclosures
This research was supported by a grant titled Potential Tradeoffs Between Metabolic Illness and Infectious Disease from Eli Lilly and Company, grant RO1-DA-015627-05 from the National Institute on Drug Abuse, a grant titled HIV Prevention Program among Substance Abusing SMI from the National Institute on Drug Abuse, grant RO1-NR-008851-05 from the National Institute of Nursing Research, and grant RO1-NR-008851-05 titled Nursing Intervention for HIV Regimen: Adherence Among SMI from the National Institute of Nursing Research.
The authors report no competing interests.