Despite the fact that psychiatric disorders (schizophrenia, mood and organic brain disorders) and their treatment may lead to oral diseases, awareness of dental status and oral health care needs among patients with these disorders is lacking (
1,
2,
3 ). Risk factors for poor oral health in this population include both patient-related and service-related variables. Patient-related risk factors include smoking heavily (
4 ), neglecting oral hygiene (
5,
6 ), having a diet rich in carbohydrates (
7 ), and abusing alcohol and drugs (
8 ). Service-related factors include lack of suitable dental clinics, lack of budgeted funds to provide dental services and poor accessibility of dental services (
9 ), insufficient concern of psychiatrists (
10 ), and the use of psychotropic medications that can cause dry mouth (
11,
12 ), which contributes to oral health problems.
In Israel, two large epidemiological surveys of oral health and care needs among hospitalized psychiatric patients have been carried out within the past 12 years. The first survey was conducted in 1997, and it compared a representative cohort of psychiatric inpatients with the general population. The survey found that there was "urgent need for an intervention program to improve dental health care in chronic psychiatric inpatients" (
10 ). As a result of the survey, considerable collaborative efforts were made by the Division of Dental Health and the Division of Mental Health Services at the Israeli Ministry of Health to improve the existing dental services within the psychiatric inpatient system (
13 ). These included supplementing the infrastructure and dental equipment, increasing manpower in the existing clinics, and establishing a central supervisory system in the Division of Dental Health at the Ministry of Health to ensure that the dental clinics were properly set up (ten out of 14 mental health centers had on-site dental clinics and were overseen by this system). Regulations were issued by the Ministry of Health that stated that every inpatient hospitalized for longer than a year (long-stay inpatient) will receive regular dental examinations and continuous treatment. Hospitals that do not have a dental clinic are required to outsource dental services. Four out of 14 mental health centers in Israel began referring patients to off-site community dental health clinics. The Ministry of Health covered expenses for in-house and outsourced dental services for long-stay inpatients. A special budgetary item for long-stay inpatients was created in 1998 for this purpose (
13 ). In addition, the Community-Based Rehabilitation of the Mentally Disabled Act of 2000 stated that the state is responsible for funding dental treatments for outpatients with mental illness who are considered to be disabled according to criteria of the National Insurance Institute of Israel (
14 ). The second survey was undertaken in 2006 to assess the effectiveness of this reorganization (
15 ).
In the study presented here we compared data from these surveys to determine changes in dental health and oral care needs between the two large cohorts representing the psychiatric inpatient population before (1997) and after (2006) the reform of dental services in psychiatric hospitals in Israel.
Methods
Sample
The data analyzed in this cross-sectional study came from the two large-scale surveys (
10,
15 ). Both surveys used the same methodology, sampling procedure, and instruments and were approved by the Ministry of Health's institutional review board. Briefly, 18 psychiatric hospitals in 1997 and 14 psychiatric hospitals in 2006 were surveyed. These hospitals provided treatment for approximately 98% of inpatients with chronic psychiatric disorders. For both surveys, a list of all patients hospitalized for longer than one year was compiled. The prereform cohort consisted of a random sample of 10% (N=431) of these patients, and the postreform cohort consisted of a random selection of 13% (N=254). Standard demographic data (age and gender) and information on the clinical diagnoses (according to
ICD-10 codes [16]) were collected from the medical records at both time points.
Procedure
In both 1997 and 2006 the dental examination was carried out by two experienced clinicians using a dental mirror and probing techniques, while the patient sat in front of a window, under natural light. Patients from closed wards and bedridden elderly patients were examined within the wards. Patients were checked for state of the teeth and presence of restorations (for example, fillings, veneers, crowns, implants, bridges, and dentures), state of the soft and hard tissues, and periodontal status. After oral examination of each patient, the dentist recorded the number of decayed, missing, and filled teeth (DMFT) in the permanent dentition. The classic DMFT index—based on in-field clinical examination of individuals by using a dental probe, dental mirror, and cotton rolls—is one of the most common methods for assessing the prevalence of dental caries and the need for dental treatment in various populations. The DMFT component scores and the DMFT index score (sum of the three components) (
17 ) were calculated. It should be kept in mind that because the DMFT index is done without X-ray imaging, it underestimates the prevalence of dental caries and the need for treatment (
18 ).
Data analysis
All analyses were performed with SPSS, version 14.0. Mean±SD DMFT index scores and component scores are presented. Differences between the pre- and postreform cohorts were tested with chi square statistics or Mann-Whitney test (as appropriate) for nominal data and two-tailed t tests for continuous data. The level of statistical significance was set at .05.
Results
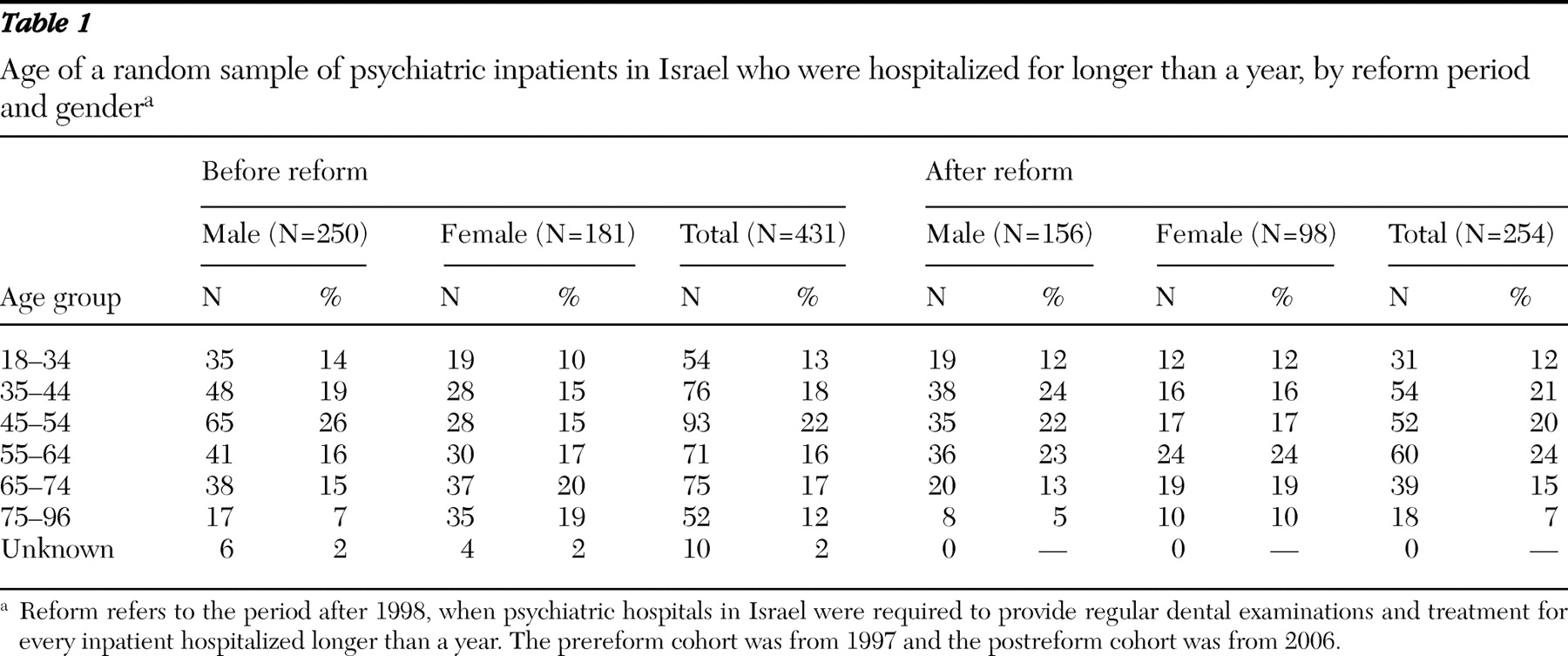
Table 1 presents age and gender distribution in the two cohorts. The cohorts were comparable, except for female patients aged 75–96, who were overrepresented in the prereform cohort (
χ 2 =8.54, df=5, p<.01).
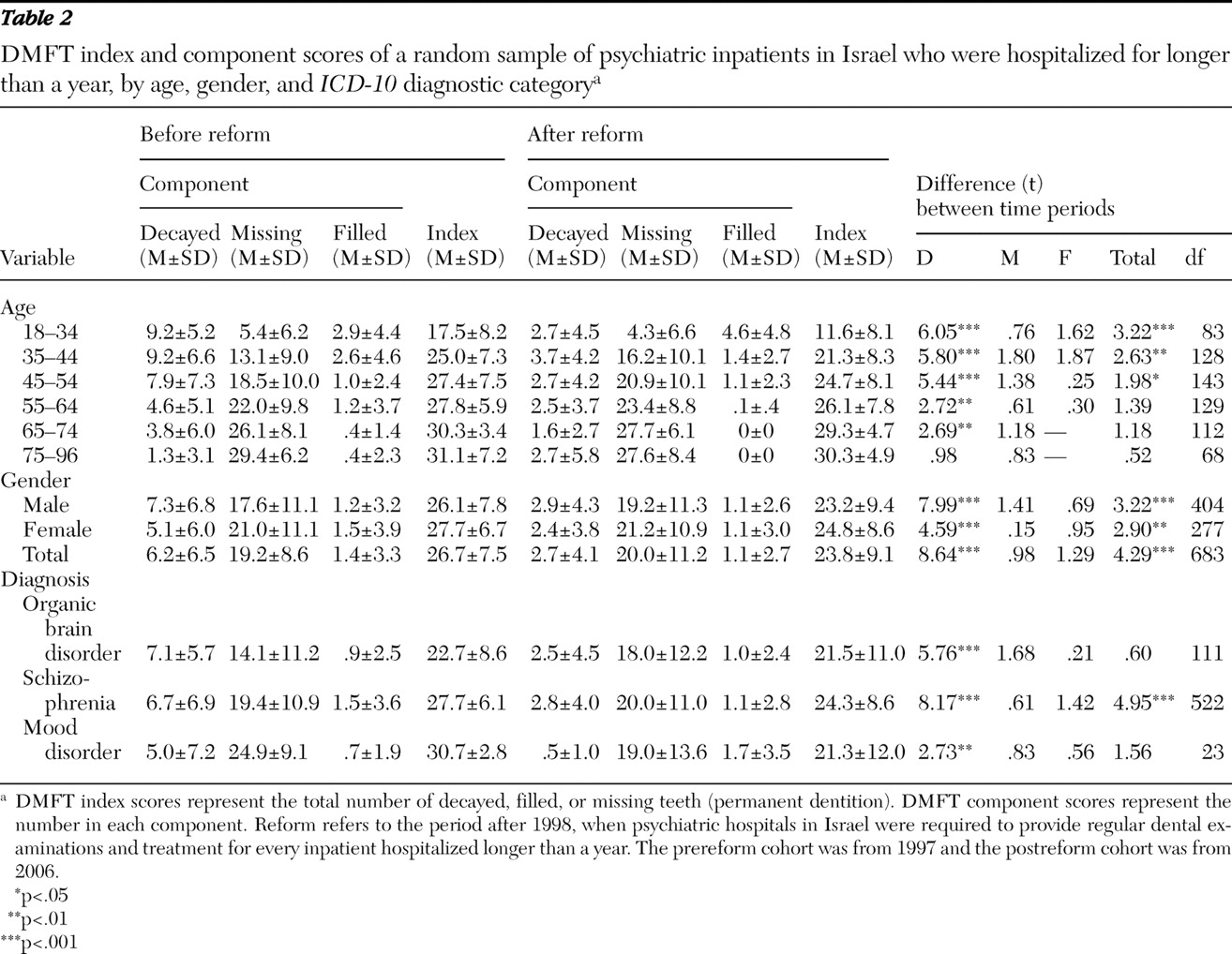
Table 2 compares DMFT index scores and DMFT component scores between the cohorts according to age, gender, and
ICD-10 diagnostic category. As can be seen, there were significant differences in mean DMFT index scores between the two cohorts. The findings varied by DMFT component and by demographic and clinical characteristics.
Gender effect
For both genders, significantly lower mean DMFT index scores and DMFT decayed component scores were found in the postreform cohort, compared with the prereform cohort. No statistically significant cohort and gender differences were found in DMFT filled and missing component scores.
Age effect
For the young and middle-age groups (18–54 years), mean DMFT index scores were significantly lower in the postreform cohort, compared with the prereform cohort. However, there were no between-cohort differences for the older age groups (55–96 years). The DMFT decayed component score was markedly lower in the postreform cohort than in the prereform cohort for all age groups, except for the oldest age group (75–96 years), where no significant difference was noted. In contrast, for all the age groups, no significant between-cohort differences in DMFT filled and missing component scores were found (
Table 2 ).
Clinical diagnosis
Independent of clinical diagnosis (organic brain disorder, schizophrenia, or mood disorder), compared with inpatients in the prereform cohort, those in the postreform cohort had lower scores on the DMFT decayed component. Mean DMFT index scores were significantly lower in the postreform cohort for inpatients with a diagnosis of schizophrenia (p<.001).
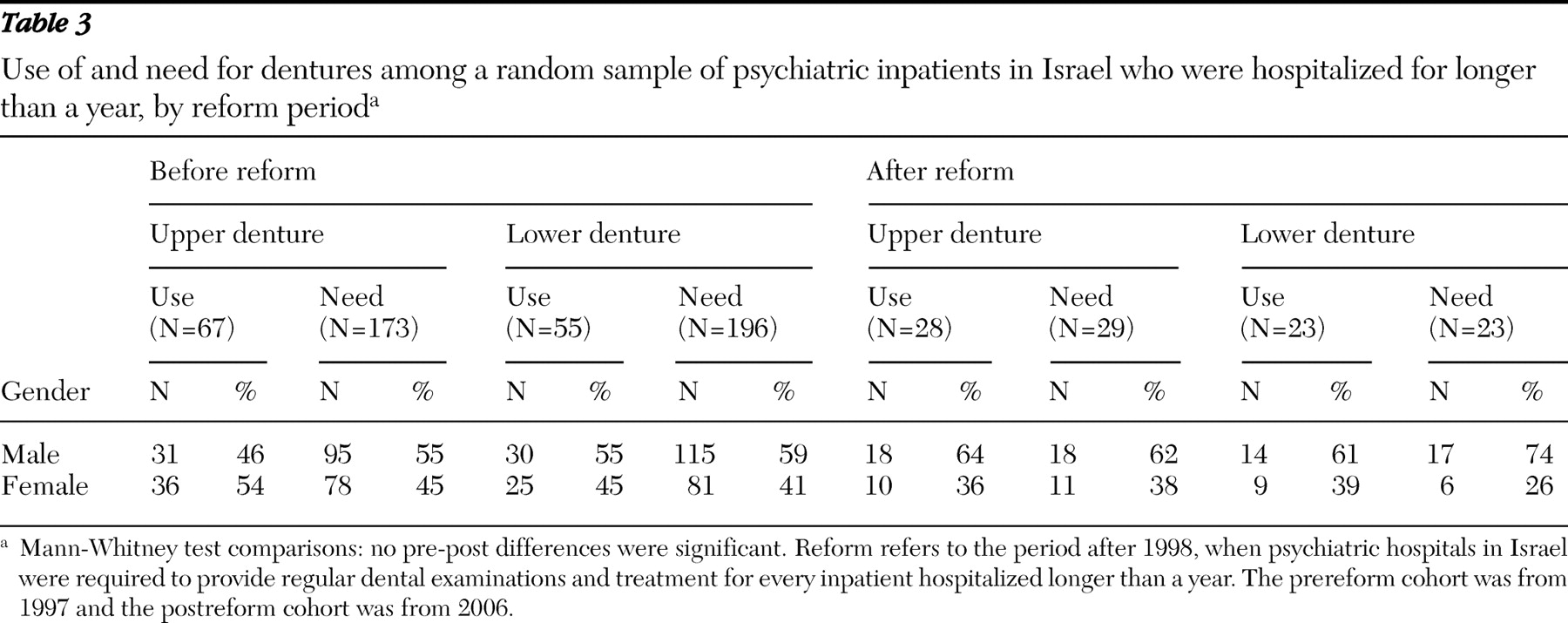
Table 3 shows that no between-cohort differences were found in the use of and need for dentures. However, there were significant gender differences in the postreform cohort, with male patients having more use of upper dentures (z=2.14, p<.05) and more need for lower dentures (z=3.24, p<.001), compared with female patients, whereas no such differences were noted in the prereform cohort.
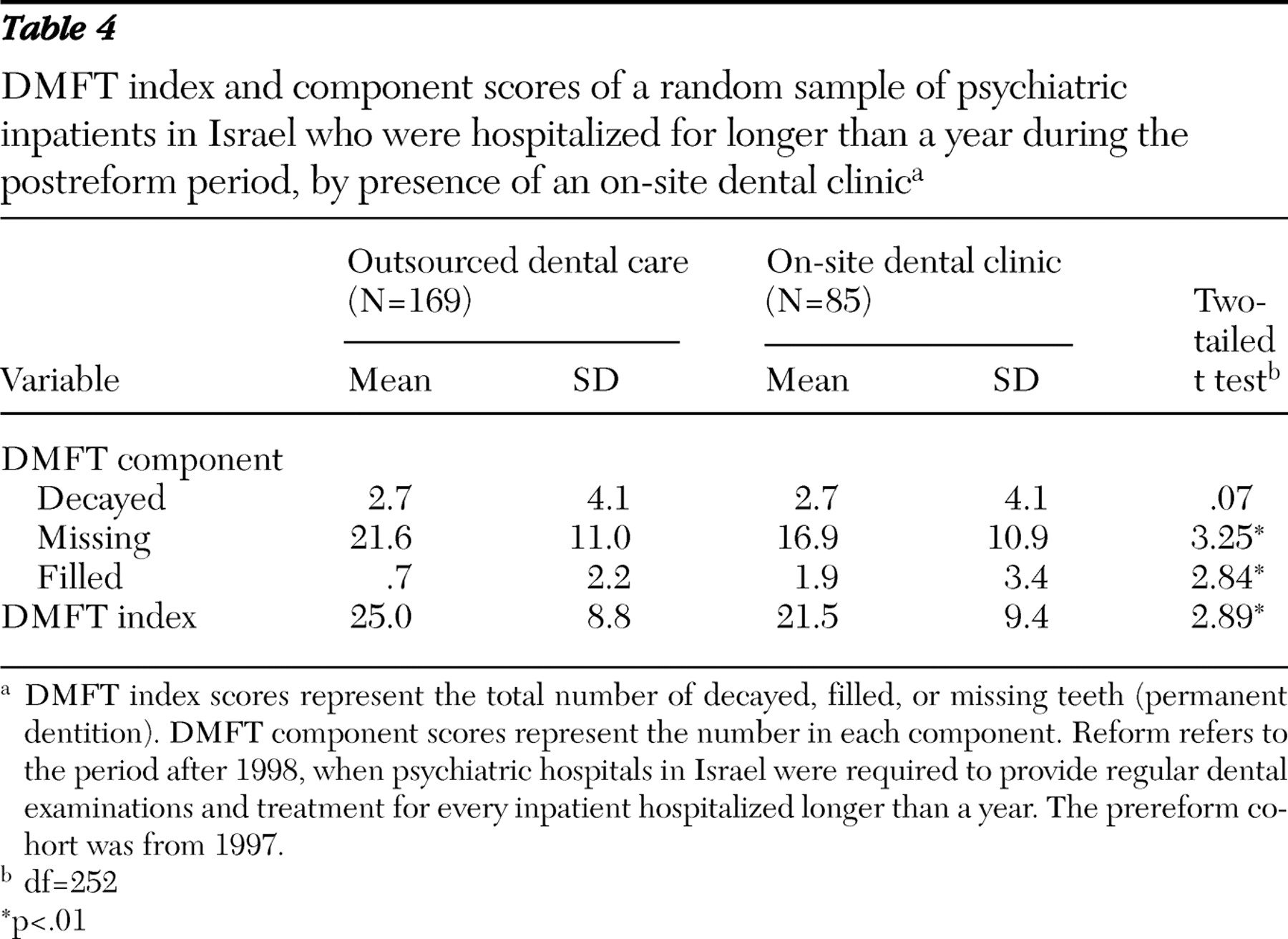
In order to test the assumption that implementing dental services in psychiatric hospitals was responsible for the detected differences between the two cohorts, we compared mean DMFT index scores and DMFT component scores between two subgroups of psychiatric inpatients in the postreform cohort—that is, 85 inpatients from hospitals having an on-site dental clinic and 169 inpatients from hospitals that outsourced dental services (
Table 4 ). We found that compared with patients in hospitals that outsourced dental services, those in hospitals with an on-site dental clinic had significantly lower DMFT index scores and DMFT missing component scores (p<.01 for both) and a higher DMFT filled component scores (p<.01).
Discussion
In this study we compared the oral health and dental care needs of two epidemiologically defined cohorts representing psychiatric inpatients in Israel before and after a major reorganization of dental services in the psychiatric hospital system. Our findings showed significant differences between the cohorts, demonstrating the substantial beneficial effects for oral health and care needs of these patients over time. After the reform, inpatients had fewer carious teeth and lower DMFT index scores, and these findings were independent of gender, age, and clinical diagnosis.
Two alternative explanations for these findings are possible. The first is that the observed positive changes are a result of the beneficial reorganization of dental services that was carried out between the two surveys. Indeed, during this period ten out of 14 psychiatric hospitals surveyed were provided with a dental clinic with necessary equipment and manpower. This explanation is supported by our finding that in the postreform cohort, patients in hospitals with in-house dental services had significantly fewer missing teeth, significantly more filled teeth, and significantly lower DMFT index scores, compared with those in hospitals where dental services were outsourced.
However, an alternative explanation is that the better dental status in the postreform cohort is not a direct effect of the dental reform. Instead, it may be attributed to the indirect effects of intense deinstitutionalization that occurred during the same time period. In 2000 the Community-Based Rehabilitation of the Mentally Disabled Act was introduced, which set up an integrated organizational framework to secure sufficient funding for the long-term outpatient rehabilitation for persons with mental illness (
19 ). In addition, the act (
14 ) secured special funding for dental care for this group of outpatients. A massive reduction in the number of inpatient beds along with parallel growth in the number of community-based facilities (
20 ) might have led to a situation in which patients with better dental status left the hospital and those with relatively poorer dental status remained. This would explain why there was not a significant change in DMFT index scores between the two periods in the older age groups. In these groups (55–74 years), DMFT index scores remained unchanged, although DMFT decayed component scores decreased over time. This finding suggests that the older inpatients—who, as a group, may have had a greater need for inpatient treatment and poorer dental health—continued to stay in hospitals during the postreform period, whereas their younger counterparts—who, as a group, may have had less need for inpatient treatment and better oral health—were moved from hospital to the community. This theory is supported by a study demonstrating poor oral health and increased dental treatment needs among patients in psychiatric institutions for elderly persons (
21 ).
Clinical diagnostic category and gender of the inpatients were not associated with dental health status. At the same time, we found gender differences in the use of and need for dentures during the postreform period. Although there was a trend toward improvement over time among men, no such tendency was observed among women. Further investigation is needed to explain this finding.
Limitations of this study are related to its cross-sectional design. A prospective cohort design is required to determine whether there is a causal relationship between the reform and the variables under study. Additional analyses of the two cohorts controlling for time spent in the hospital and severity of psychopathology would have helped to determine whether we were correct in hypothesizing that the postreform cohort consisted of inpatients who were not discharged from the hospital to a community residence because of the severity of their psychopathology. Unfortunately, we were unable to assess the severity of psychopathology for these inpatients. Another shortcoming of this study is that because of a small number of patients receiving psychotropic drug monotherapy, we were not able to control for changes in psychotropic drug use (introduction of second-generation antipsychotics) that occurred during this period. The massive change from first- to second-generation antipsychotics, which have a safer side-effect profile—in particular second-generation antipsychotics are less likely to cause dry mouth—could affect our results. However, treatment with second-generation antipsychotics is also related to increased appetite and consuming a rich carbohydrate diet, both of which could have a negative effect on dental hygiene.
Conclusions
Our findings suggest that an improvement in the dental health of this at-risk population resulted from the improved access to dental health care services in the psychiatric hospital system. However, because oral disease levels still remain high, further steps are necessary to treat these diseases and to prevent their progression. On-site dental services were shown to be better than outsourced services. In addition to the improvements in dental health services described in this report, implementing existing oral health promotion programs (
6,
9,
22 ) among persons with psychiatric disorders may be useful.
Acknowledgments and disclosures
Dr. Ponizovsky was supported in part by the Ministry of Immigrant Absorption.
The authors report no competing interests.