According to a recent U.S. Department of Housing and Urban Development report, an estimated 670,000 individuals in the United States were homeless on a single day in 2007 and 120,000 of these individuals were chronically homeless (
1 ). Veterans composed approximately 15% of the sheltered homeless adult population in 2007 (
1 ) and nearly 33% of the adult male homeless population in a 1996 survey (
2 ). Despite efforts to address homelessness among veterans, increasing numbers of veterans returning from service in Afghanistan and Iraq are becoming homeless or are at risk of becoming homeless (
3 ).
Persons experiencing homelessness have higher rates of substance use and problems with mental health, physical health, and legal and employment issues (
4,
5,
6,
7,
8 ). Substance use may be the most salient factor causing homelessness (
9 ).
Given the complexity of problems affecting homeless individuals, designing substance abuse treatment that addresses the needs of this population is challenging. For example, day treatment for cocaine dependence reduced drug abuse among nonhomeless participants but incurred 100% dropout among homeless participants (
10 ). Homeless individuals with substance use disorders have nearly 50% fewer successful treatment outcomes than those stably housed (
11 ). Providing direct housing assistance seems to help. Addition of housing for homeless individuals with substance use disorders in behavioral day treatment improved drug abuse outcomes and decreased homelessness (
12,
13,
14 ). Other potential treatment modalities include case management and integrated models of care (
15,
16 ). Long-term supported housing services, which included intensive case management, improved both housing and substance use outcomes among homeless veterans (
17,
18 ).
Although supported housing programs are associated with improved substance use outcomes in civilian and veteran populations, few veterans seeking substance abuse treatment have access to such long-term programs. Many housing programs require a period of abstinence before referral, making them inaccessible to many veterans with substance use disorders. Although U.S. Department of Veterans Affairs (VA) treatment programs may address homelessness through transitional housing, such as domiciliaries, or through relationships with community programs, such resources are often limited. Despite these realities, few studies have explored the impact of housing status on outpatient treatment outcomes and service utilization.
In this secondary analysis, we examined data from a cohort of veterans entering outpatient substance abuse treatment who were randomly assigned to receive primary care on site in an addiction treatment setting or at a primary care clinic (
19 ). We evaluated the prevalence of homelessness over 12 months, examined associations between demographic and baseline characteristics and housing status, and explored associations between housing status, treatment outcomes, and utilization of other VA services. On the basis of prior studies cited, we hypothesized that homeless veterans would be more severely impaired at baseline, have poorer treatment outcomes after analyses controlled for baseline severity, and utilize services more than those with more stable housing.
Methods
Participants
From March 2000 until March 2003, veterans (N=2,731) entering treatment at the VA Puget Sound Health Care System (VAPSHCS) Addiction Treatment Center (ATC) were screened for enrollment in a prospective, randomized controlled trial of on-site versus referral primary care (
19 ). Eligibility criteria included one or more self-reported chronic general medical conditions, elevated blood pressure, or abnormal laboratory screen. Veterans with primary care providers or general medical problems in three or more organ systems were excluded. A total of 720 veterans were thus assigned randomly to receive primary care either in the ATC (on site) or the General Internal Medicine Clinic of VAPSHCS (referral). Participants received substance abuse treatment as clinically indicated via group and individual formats, as well as specialty referrals to inpatient and residential programs. Ongoing treatment participation was not a requirement for continued study participation or for receiving primary care.
The study was approved by the University of Washington Human Subjects Committee. After completely describing the study to the participants, study staff obtained written informed consent. Participants were assessed at baseline and at three, six, and 12 months postbaseline. Veterans who did not complete at least one follow-up visit (N=78; 32 housed, 42 homeless, and four unknown at baseline) were excluded from this analysis because their housing status over the study course could not be determined. The housing status of an additional 20 participants was indeterminable either because of missing data (N=3) or because they were living primarily in restricted settings, such as jails, residential facilities, or halfway houses (N=17); these participants were excluded, for a final sample of 622.
Classification of homelessness
Housing information was obtained at baseline and three, six, and 12 months later via Form 90, which uses the timeline follow-back method (
20 ). Participants were asked how many days they were living in their own home or apartment, living with others (but paying no rent), or homeless in the past 90–180 days (at baseline and 12-month assessments, days assessed for homelessness ranged from 90 to 180 based on the date of last drink; at three- and six-month assessments, homelessness in the past 90 days was assessed). An established definition of literal homelessness in the literature is living in shelters, cars, bus stations, abandoned buildings, or outdoors (
21,
22 ). We adopted this definition and used a previously documented method, which classifies homelessness as self-report of spending one or more nights "literally homeless" (
23 ). Participants reporting no days of homelessness were classified as housed provided that they lived either in their own home or in marginal housing, such as with friends or family, for at least 30 days in the period of interest.
Participants were classified into four groups on the basis of housing status at baseline and at final follow-up for which data were available: housed at baseline and at final follow-up (consistently housed; N=255, 41%), met criteria for homelessness at baseline and at final follow-up (consistently homeless; N=168, 27%), housed at baseline but homeless at final follow-up (housed baseline-homeless final; N=51, 8%), and homeless at baseline but housed at final follow-up (homeless baseline-housed final; N=148, 24%).
Outcome variables
Addiction Severity Index (ASI) composite scores were the primary outcome measures. ASI composite scores rate severity in seven areas affected by substance use problems (medical, employment, alcohol use, drug use, family and social life, legal, and psychiatric) (
24 ), focus on the 30 days before the interview, and are sensitive to changes in severity over time. Scores range from 0 to 1, with higher scores indicating greater problem severity. The ASI is acceptable for use with homeless individuals with substance use disorders (
25,
26 ). Additional substance use outcomes included 30-day abstinence from alcohol and drugs as determined from ASI data. Participants reporting one or more days of use were classified as nonabstinent, as were those with missing abstinence data.
Engagement in substance abuse treatment was defined as attending two or more treatment appointments in three consecutive 30-day periods after treatment initiation. Length of treatment was determined by the number of days in treatment up to the last visit before dropout.
The VA electronic medical record was used to calculate the number of outpatient visits and hospitalizations during the study, and the Decision Support System was used to determine participants' total cost of care at VAPSHCS (
27 ).
Data analysis
Baseline differences among housing groups were examined by using linear and logistic regression models for continuous and dichotomous variables, respectively. Likewise, logistic and linear regression models were used to compare the baseline characteristics of the full sample to participants who were excluded from analyses because they had no follow-up visit or their housing status was indeterminable (N=98).
Analyses of outcomes were adjusted for randomized treatment location (on-site or referral primary care), age, primary substance (alcohol, cocaine, opioids, or other), presence of any psychiatric condition at baseline per medical record review, race, baseline alcohol or drug abstinence, and final assessment time point (three, six, or 12 months). Analyses of 12-month outcomes were adjusted for baseline scores on the respective dependent variables. Multivariate logistic and linear regression models were used to analyze dichotomous (30-day abstinence at 12 months, treatment retention, and hospitalizations) and continuous (length of stay in treatment and 12-month ASI composite scores) outcomes, respectively. Multilevel mixed-effects linear regression models were used to examine change in ASI composite scores over time by housing group. This analysis yielded individual change parameters based on available data and was less vulnerable to distortion by missing data for participants who did not attend one or more follow-up assessments. Main analyses compared the continuously housed group with the three homeless groups. Postestimation Wald tests were used to examine differences between the homeless groups.
VA costs were analyzed with the Wald test, which allows for a comparison of mean costs of log-normal data and considers both zero and nonzero costs and is less susceptible to problems of skewness caused by zero costs (
28 ).
Results at p<.05 (two sided) were considered significant. Postestimation results at p<.01 are reported. All analyses were conducted with Intercooled Stata, version 9.2. Robust standard error estimates were used whenever possible.
Baseline data were available for the full sample of 622 veterans, as were data on treatment retention, service use, and cost. ASI 12-month data were missing for 111 participants who did not complete the 12-month assessment. As stated above, participants with missing data at 12 months were coded as nonabstinent. Analyses of 12-month ASI scores did not include participants with missing data, for a sample size of 511 (82% of the full sample). Linear and logistic regression models for continuous and dichotomous variables, respectively, were used to test for baseline differences between those with and without 12-month data. Tests of change over time used all available data points and included all participants.
Results
Impact of missing data
Participants included in the analyses (N=622) had higher baseline ASI drug composite scores than those who were excluded (N=98) ( β =.03; 95% confidence interval [CI]=.00–.05, p=.019). The included and excluded groups did not otherwise differ on demographic variables, presence of a psychiatric condition, primary substance of use, other baseline ASI composite scores, or baseline abstinence. No baseline differences were detected between participants with (N=111) and without (N=511) missing 12-month ASI data.
Participant characteristics
Of the 622 participants, 49% (N=306) reported being housed at baseline and 51% (N=316) were homeless for one or more days. Sixty-five percent (N=404) of the total group met criteria for homelessness at baseline or at one or more follow-up assessments at three, six, or 12 months.
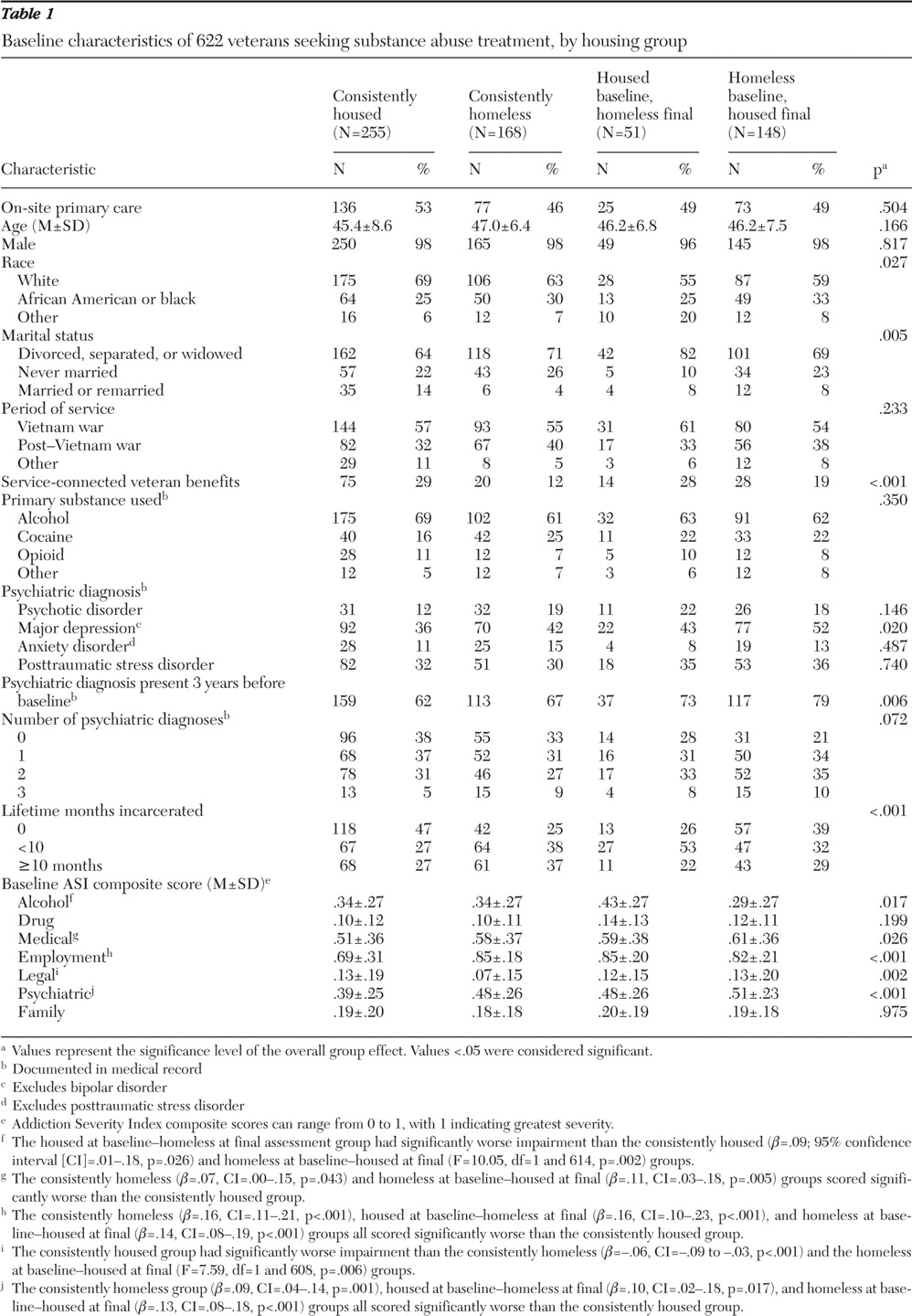
Table 1 summarizes demographic and baseline characteristics of each housing group. The groups differed with respect to whether they received VA service-connected disability benefits, race, marital status, and incarceration history. No differences were detected in primary substance used. Participants in the homeless groups tended to be more likely than the consistently housed group to have co-occurring psychiatric diagnoses in general and major depression in particular. The groups were not significantly different on other baseline variables.
The housing groups differed at baseline on several ASI composite scores (
Table 1 ). The housed baseline-homeless final group scored significantly worse on the composite for alcohol use problems relative to both the consistently housed and the homeless baseline-housed final groups. On the medical composite, the consistently homeless group and the homeless baseline-housed final group scored significantly worse than the consistently housed group. All groups experiencing some homelessness scored significantly worse relative to the consistently housed group on the employment and psychiatric composites, with no differences detected on these measures between the three groups experiencing homelessness. The consistently homeless group reported significantly fewer legal issues than the consistently housed group and the homeless baseline-housed final group. No significant differences were detected in composite scores for drug or family problems.
Treatment retention and length of treatment did not differ significantly between the groups. Roughly 65% of participants in each group remained engaged in treatment for 90 days, and the average length of treatment across groups was 144.4±113.5 days (data not shown).
Substance abuse treatment outcomes
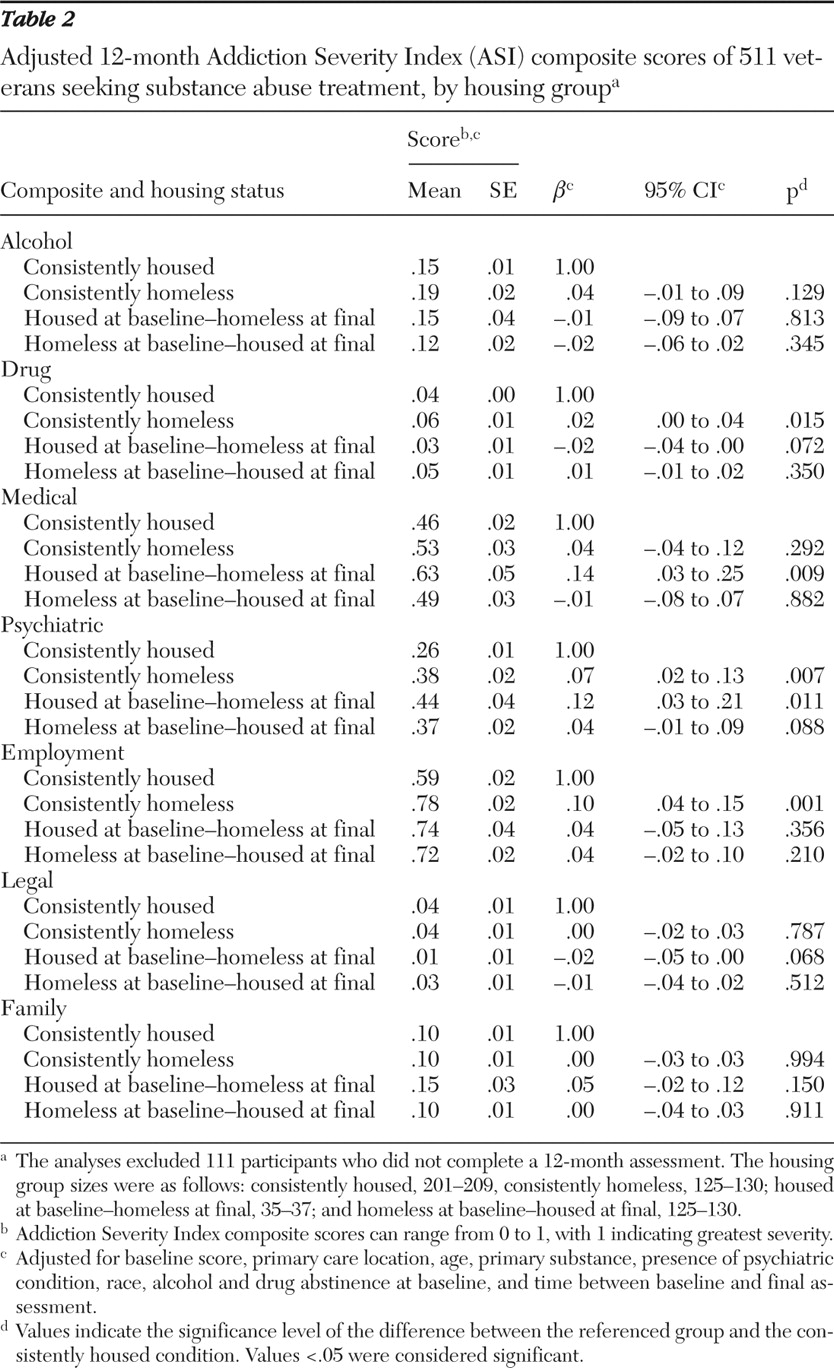
Twelve-month ASI outcomes. Table 2 shows 12-month ASI scores by housing group. Mean adjusted 12-month composite scores concerning alcohol use problems improved from baseline in all groups, with no significant differences detected between the housing groups. Although the 12-month drug composite scores were low among all groups, the consistently homeless group tended to have higher scores (indicating greater severity) than the consistently housed group and the housed baseline-homeless final group (adjusted F=11.95, df=1 and 486, p<.001). In addition, the consistently homeless group scored significantly worse on psychiatric and employment composite scores than the consistently housed group. Veterans who were housed at baseline and homeless at final follow-up had poorer psychiatric and medical composite scores than the consistently housed group and had poorer medical composite scores than the homeless baseline-housed final group (adjusted F=7.09, df=1 and 491, p=.008). No differences were seen on legal or family composite scores.
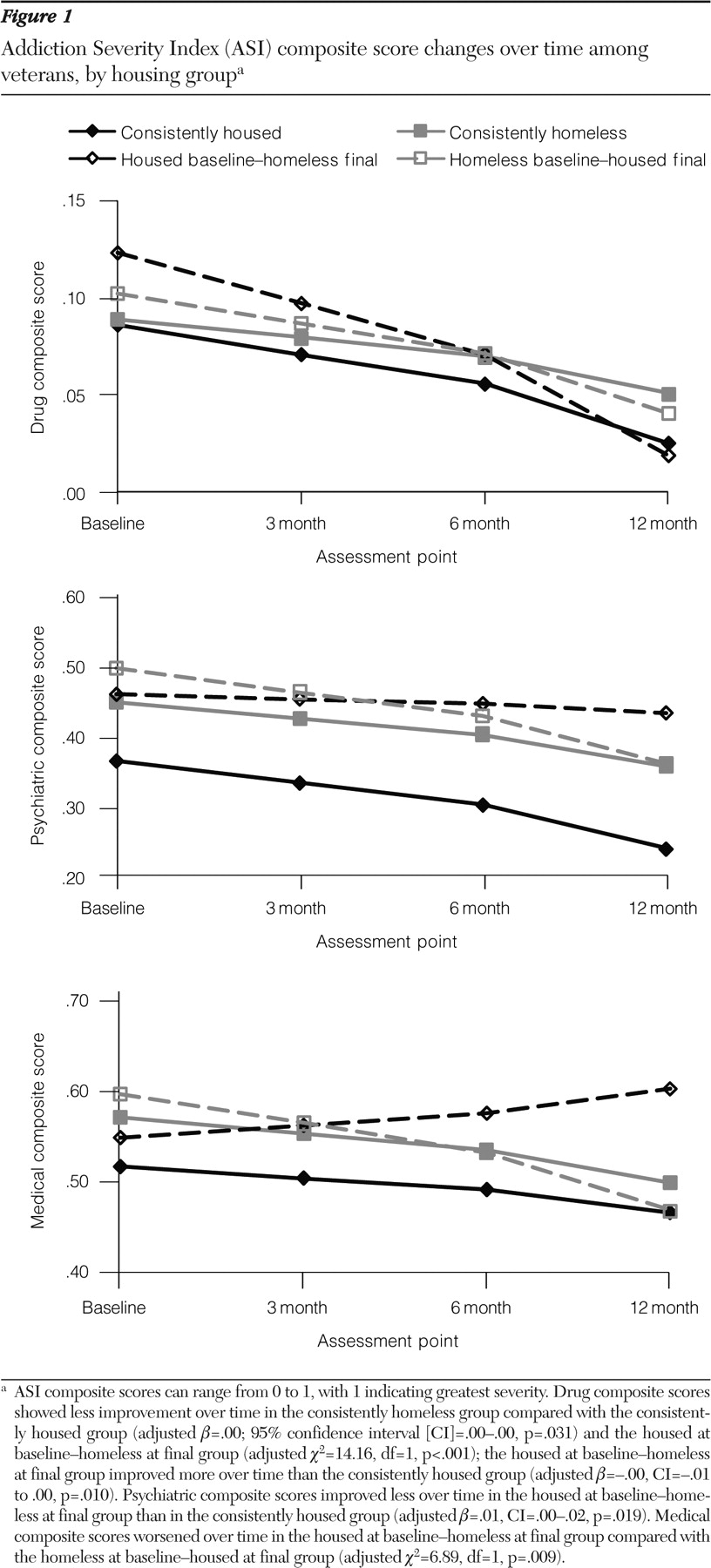
Change over time in ASI composite scores. Figure 1 plots the ASI drug, psychiatric, and medical composite scores over time among the four housing groups. Although on average all groups improved, drug composite scores improved less in the consistently homeless group than in the consistently housed group and the housed baseline-homeless final group, whereas the housed baseline-homeless final group improved more over time than the consistently housed group. Psychiatric composite scores improved less in the housed baseline-homeless final group than in the consistently housed group. In addition, the housed baseline-homeless final group's medical composite scores significantly worsened over time relative to the homeless baseline-housed final group. Legal composite scores showed less improvement over time in the consistently homeless group than in the consistently housed group (data not shown; adjusted
β =.00, CI=.00–.01, p=.008). No other ASI composite categories showed significant differences across housing groups in change over time.
Twelve-month abstinence. The adjusted proportions of participants reporting abstinence from alcohol and drugs at 12 months (with missing data assumed to reflect nonabstinence) were as follows: consistently housed, .50 (CI=.44–.56); consistently homeless, .43 (CI=.36–.52); housed baseline-homeless final, .38 (CI=.25–.54); homeless baseline-housed final, .51 (CI=.43–.59). No significant differences in 12-month abstinence were detected between housing groups.
Service utilization and costs
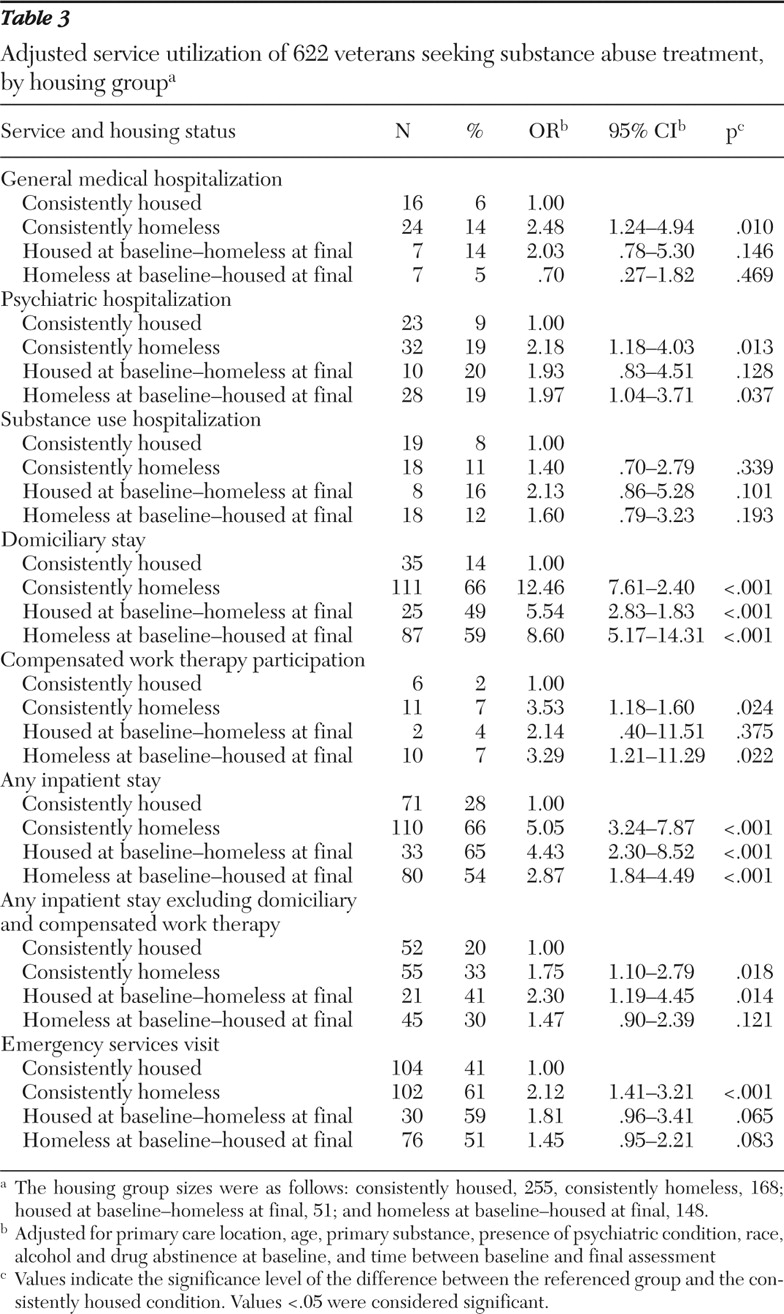
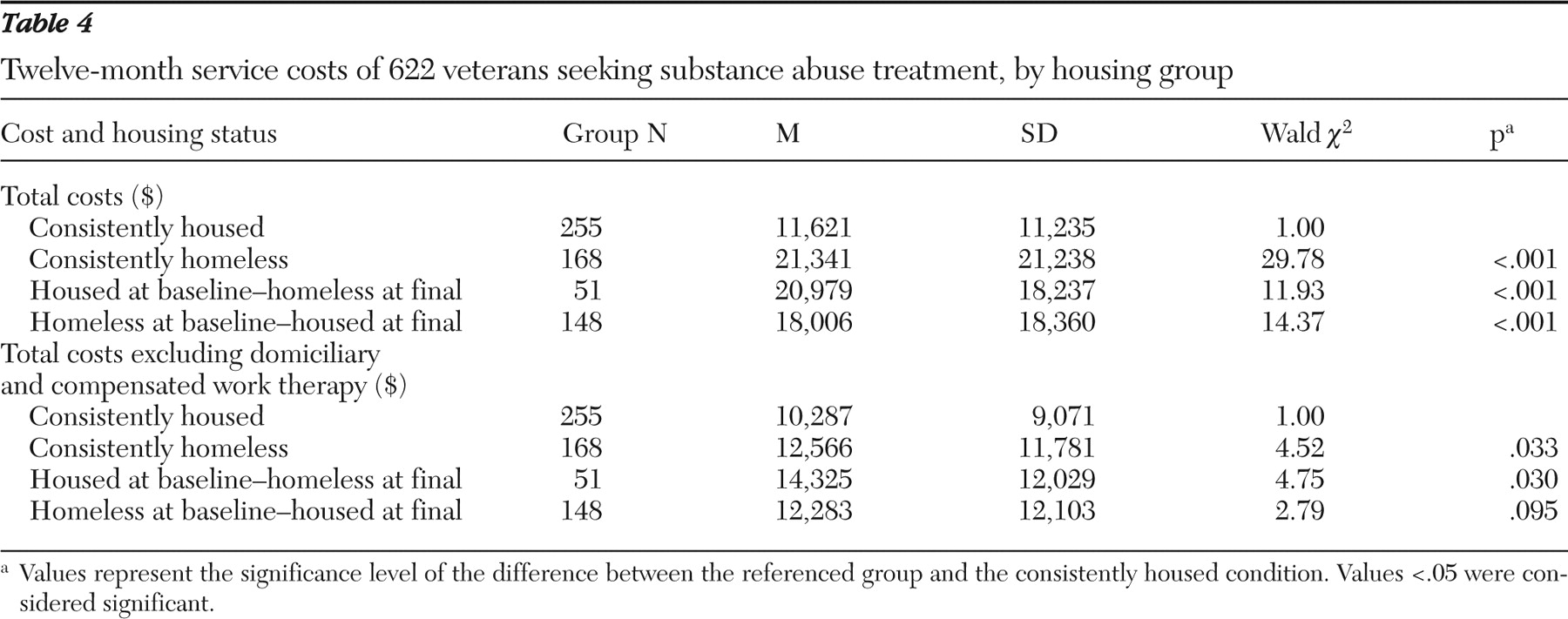
VAPSHCS service utilization and costs for the one year of study participation are presented in
Tables 3 and
4, respectively. All homeless groups were more likely than the consistently housed group to have one or more inpatient admissions. After removing VA domiciliary and compensated work therapy stays, which are geared to homeless individuals, from analyses of inpatient admissions, we found that the groups that were consistently homeless and homeless at final assessment were more likely than the consistently housed group to have an inpatient admission. The consistently homeless group was more likely than the consistently housed group to have a psychiatric hospitalization and was more likely than the consistently housed group and the homeless baseline-housed final group to have a general medical hospitalization (adjusted
χ 2 =7.78, df=1, p=.005). The proportion of participants with a psychiatric hospitalization was higher in the homeless baseline-housed final group than in the consistently housed group. These differences in service utilization were reflected in higher total treatment costs for all homeless groups compared with the stable group (
Table 4 ).
The consistently homeless group was more likely than the consistently housed group to use emergency department services (
Table 3 ). Differences also were seen in changes in the likelihood of using emergency services over time, with the homeless baseline-housed final group becoming less likely to utilize emergency services over time compared with the consistently housed group (adjusted odds ratio=.58, CI=.45–.76, p<.001) and the consistently homeless group (adjusted
χ 2 =7.32, df=1, p=.007).
Discussion
Our findings indicate that the problem of homelessness among veterans with substance use disorders remains large, with 65% of 622 veterans in this study spending at least one night homeless at some point during an 18-month period. Consistent with the literature (
4,
5,
6,
7,
8 ), this study found that participants experiencing homelessness during the six months before study enrollment had more severe alcohol, medical, employment, legal, and psychiatric problems than participants with housing.
Participants on average, regardless of housing status, benefited from treatment. Surprisingly, and in partial contradiction to our hypothesis, those in the homelessness groups were comparable to the consistently housed veterans with respect to treatment engagement at 90 days and average number of days in treatment. These outpatient treatment retention numbers for homeless participants are higher than some have previously reported (
10,
11 ). Most homeless veterans in our study accessed short-term housing support through a domiciliary program; it is not known how many may have received care through community programs. These services may have increased treatment retention.
After we controlled for baseline severity, final ASI drug and psychiatric composite scores were better among veterans consistently housed than among those in the consistently homeless group. These differences indicate that, in partial support of our hypothesis, stable housing may be associated with slightly more positive treatment outcomes among veterans in outpatient substance use treatment. However, such differences were not reflected in final ASI alcohol composite scores or abstinence rates, which did not appear to differ at outcome between homeless and housed groups.
Consistent with our hypothesis and with previous literature showing increased use of acute care services among homeless individuals (
29,
30 ) and high service utilization among homeless veterans (
31 ), the homeless veterans in our study used more services and had higher total costs than housed veterans even when other service costs such as domiciliary and compensated work therapy were removed.
This study has limitations. Although the data were gathered prospectively, this was a secondary analysis from a study originally designed to examine the effect of on-site versus referral primary care on addiction treatment outcomes. Although our definition of homelessness—experiencing one or more nights of "literal homelessness" during the assessment period—was supported in previous studies (
21,
22,
23 ), it does not include the marginally housed individuals living doubled-up with friends or family and does not account for duration of homelessness. Our primary outcome measures were ASI composite scores. Although the ASI has been validated in this population (
25,
26 ), other studies have shown that using multiple assessments over time can improve precision in estimating substance use among homeless persons with mental illness (
32 ). Treatment utilization and costs are limited to the VAPSHCS and do not reflect outside resources that participants may have obtained. Finally, our study was conducted at a single VA medical center with a largely male population, so these results may not be generalizable to non-VA homeless individuals.
Conclusions
This study helps to describe homeless veterans seeking outpatient substance abuse treatment and provides an initial examination of how housing status relates to treatment outcomes, as well as VA health care utilization and costs over 12 months. Although the relationship between housing status and treatment outcomes is a complex one, our results suggest that associations exist between stable housing, lower VA utilization, and more positive treatment outcomes among veterans with substance use disorders. These data indicate that a substantial number of homeless veterans are accessing short-term VA housing services; however, the ultimate impact of such services is unclear given that most individuals who were homeless at baseline continued to experience homelessness before final follow-up. Further research is needed to identify practical and effective interventions that both assist homeless veterans with substance use disorders in accessing and maintaining stable housing and improve treatment outcomes. Given the influx of younger veterans with housing and substance use problems, the need for additional knowledge about how to address these issues takes on considerable urgency.
Acknowledgments and disclosures
This study was based on work supported by grant SUI 99-109-1 from Health Services Research and Development, U.S. Department of Veterans Affairs, and by the Center of Excellence in Substance Abuse Treatment and Education at VA Puget Sound Health Care System, Seattle.
Dr. Saxon has worked as a consultant to Reckitt Benckiser Pharmaceuticals and received research support from Ortho-McNeil Janssen, Titan Pharmaceuticals, and U.S. World Meds, as well as honoraria from Forest Pharmaceuticals, Alkermes, and Cephalon. The other authors report no competing interests.