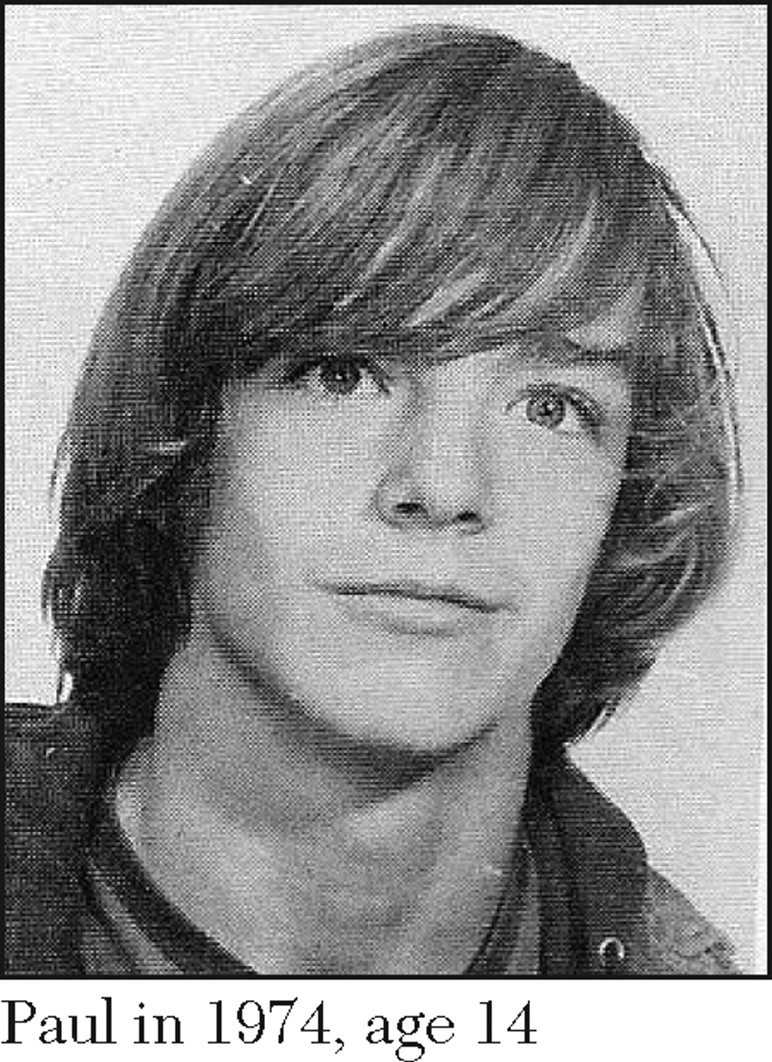
A ditty we used to sing to my brother Paul when we were little:
Tall Paul
Tall Paul
Tall Paul
He's my all
My twin brother, Paul, was among the thousands of patients who were released from the New York State hospital system in the deinstitutionalization process. Although a noble ideal—that all have a right to live with other members of society—there are some in the mentally ill population who should never be expected to live on their own and who need constant supervision. Paul was one of them.
Paul's first major psychotic episode was in 1976 at the age of 16. After a three-day observation, he was admitted to a private hospital; the diagnosis was schizophrenia. A year later, my parents' insurance "maxed out," and they were advised to commit him to the state psychiatric hospital. It was the only option to ensure that they could financially take care of their nine other children. Paul never left the state hospital system, except for short visits home or day outings, until the hospital closings caught up with him in 1998, 22 years after his commitment.
Paul was extremely resistant to any type of drug, behavioral, or cognitive therapy. He mellowed somewhat over the years, but never a day went by without his talking of something that never happened, like being killed by one of his best friends, making millions as a Kung Fu star in Korea, or having 200 children born from where his teeth once were.
Paul's lucidity was fluid. He could ask after my sons, and he loved to show me all of the pictures of his nieces and nephews in his wallet. He could play a game of pool or go bowling, but his conversations were always interspersed with a medley of delusions. Always.
My family agonized over Paul's commitment. Paul was my twin. How could I be happy when he was in "there"? Still, I went on with my life—I had to. I moved away, went to college, and got married. I even had my own set of twins. It was a blessing and a curse—a constant reminder of the twin life I had lost.
Early on, Paul's delusional ranting sometimes ruined holiday gatherings, upsetting more than the children. We loved Paul, but we were relieved to take him back to the hospital after some visits. Most ended in a pool of tears. As much as my parents, siblings, and I felt sadness, guilt, and loss, we knew that Paul could not live with us. He was very sick, and we could not manage his 200-pound frame, which still showed signs of the football player he had been.
As time wore on, we realized that Paul would never get better. I also realized neither I nor my parents "did this" to him. The drugs (PCP, acid—anything he could get his hands on) probably triggered his psychosis and might have made it much worse. I tried to forgive myself for sometimes enjoying my life. I cried less often, sent him cards and gifts on his birthday, and visited him when I was home every year or so. I sporadically sought help for my "chronic, low-grade depression."
Paul and the other patients displaced from the hospital closings were redirected onto only one track: independent living. He was put into a transitional group home on the hospital grounds, then moved to another transitional group home within an assisted-living complex, and then finally to his own apartment within the assisted-living complex. He took cooking and other life skills classes.
At first I was overjoyed. He was finally out from behind locked doors and barred windows. I think about it now and marvel at how naïve I was to think that Paul was still going to be taken care of.
About a year after Paul started his new, independent life, my sister Katherine was visiting and noticed that Paul looked skinny. She hadn't seen him in a few weeks. She eventually learned from Paul's roommate that Paul's food stamps card didn't work anymore. She found out that Paul had been knocking on doors, begging for cigarettes and food. Another time, Paul was picked up by police because he was "menacing" people on the street, yelling at them, and claiming that they stole his liver. The police took him straight to the hospital.
After the food stamps incident, Katherine met with Paul's case workers and doctors. They were still talking about moving him to an even less supervised environment—his own studio apartment. It was mind-numbingly absurd. On the one hand, the doctor acknowledged that Paul was so drug resistant that he would never get better. On the other, the case workers said that for Paul to receive help in filling out his food stamps renewal form, he was required to first ask for assistance, something he lacked the insight to do. The case workers had no idea that Paul had so little food and did not seem to acknowledge his level of disability. And now they were telling my sister that Paul would be transitioned to a completely unmonitored living environment.
Katherine remarked, "Stray dogs are treated more humanely than the mentally ill in this state." She thought Paul would die if they went through with the move. They didn't get the chance.
In another incident, Paul encountered an apartment fire. Even in his constant state of delusion, he knew enough to call for help. His quick action helped save a baby's life, and he received a citation from the fire department. Unfortunately, it sent his mind into a tailspin, and he was eventually sent back to the state hospital. During this admission, we found out that Paul had "volunteered" for a drug study. He was put in a special unit where clinicians could monitor any side effects and draw blood every day to check on how much of the drug remained in his bloodstream. Even though they took very good care of him, he was a human guinea pig!
After he was released from the state hospital—again—he was placed in a 200-bed facility called an adult home. Everyone there seemed to have a mental illness. They would mill around the halls and outside, smoking or wandering the streets. Visitors could not give my brother anything of value because it would get lost or stolen or Paul would give it away either out of generosity or in trade for cigarettes. There were times we had to ask the staff to clean his room because it smelled really bad. Other people would sometimes sleep in his roommate's bed, and one of them had a habit of wetting it. Paul again cycled in and out of the local hospital psychiatric wards and the state hospital, as did many other residents of the adult home.
How could anyone think this "life" of Paul's was better than when he was in the state hospital? During his last stay in the state hospital, we practically begged them to keep Paul. We were told this was not possible.
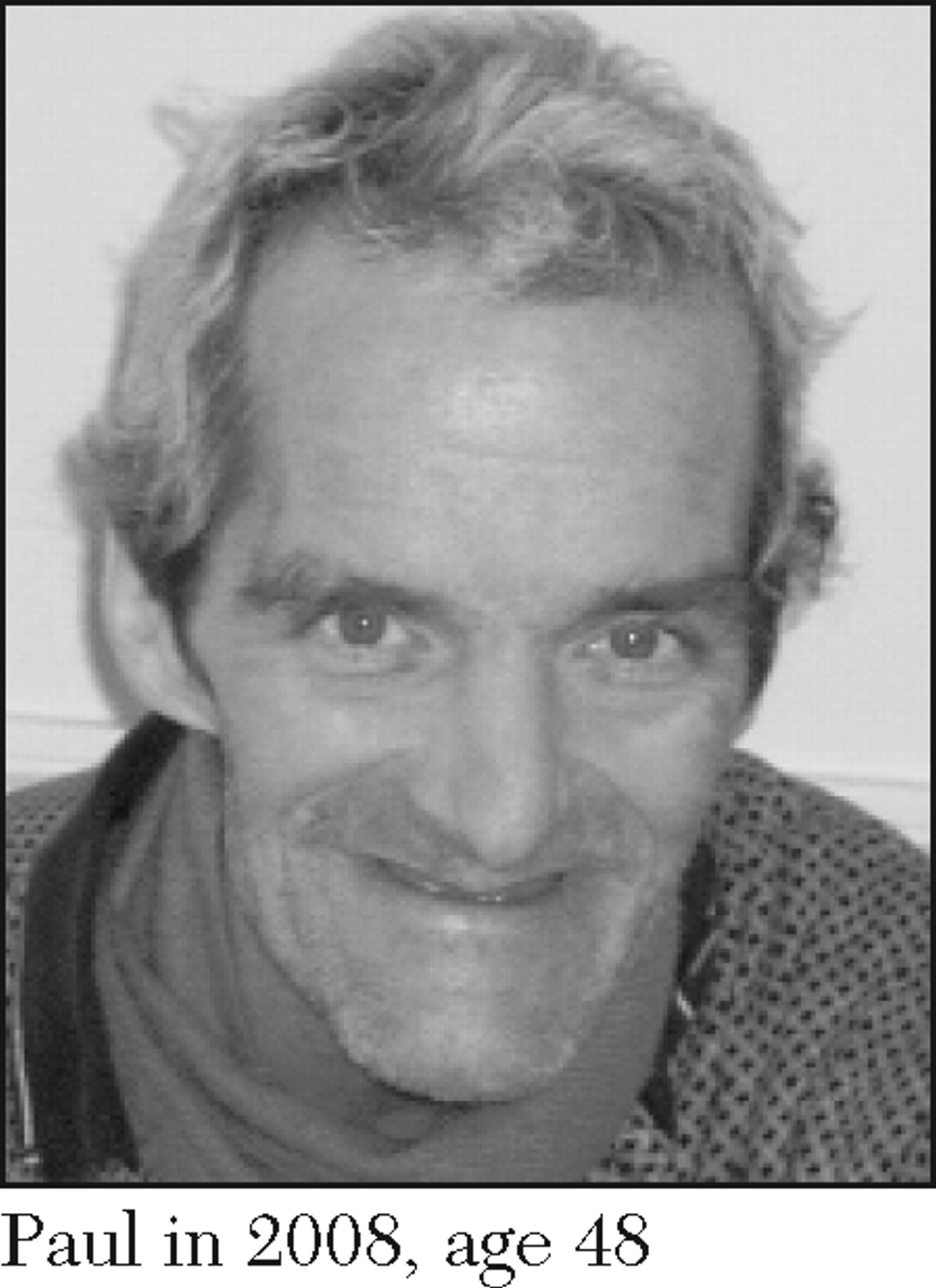
During the ten years after his initial release in 1998, Paul's general medical condition deteriorated as much as his mental condition. He looked old beyond his years. The agony that my siblings and I went through during this period of Paul's life far exceeded the agony we felt during his 22-year stay in the state hospital system.
Ironically, thanks to follow-up care received after the drug study, Paul was prescribed a drug that allowed some of his old personality to come out. We became friends with and loved this New Paul just as much or more than we loved the Old Paul, our Tall Paul. Although he was still very delusional, he didn't lash out at us as much, could participate in family gatherings better, and would cooperate in his treatment. However—and this is important—this cannot be mistaken for his ability to live with us or to live on his own. He was still too unpredictable.
In the fall of 2006, I convinced my husband to move from Wisconsin to New York so I could be near Paul after nearly 30 years. I became the initial contact for the adult home to call if anything happened to him. I saw Paul almost every weekend. I took him bowling and to the movies. He would introduce me as his twin sister. I felt somewhat whole again.
Within six months after my move back to New York, Paul had two severe bouts of pneumonia, resulting in hospitalizations. To give Paul more time to recuperate after his second hospitalization, we found a nursing home that would accept a patient with a mental illness, and it even allowed us to admit Paul permanently. By using the diagnosis of chronic lung disease instead of schizophrenia, the nursing home would not risk being categorized as an institute for mental diseases (IMD), which, under a Medicaid law called the IMD Exclusion, would cause the home to lose Medicaid subsidies for all of its patients. It took a fatal illness in an organ other than his brain for Paul to finally get the long-term care he deserved.
The nursing home staff took a liking to Paul. His nickname was "The Governor" because he said hello to everyone and shook their hands. Paul had finally found a home. They put him on a nicotine patch. We thought maybe he would be okay. But just weeks after he became a permanent resident, Paul received a diagnosis of lung cancer. He passed away nine months later. He was only 48.
Paul faced cancer and death with dignity, which could be a story all by itself. It was both humbling and uplifting to witness, and the experience brought my family closer together. If nothing else, Paul's purpose in life was to teach us the true meaning of family. Looking back, I am heartsick when I think about the life Paul had. I get angry when I think that the hellishness of his last ten years could have been prevented. My grief is subsiding, but I am not so sure my anger ever will.
My point in telling Paul's story is to illustrate what one former patient's life was like after the closings throughout the state hospital system. After Paul's roller-coaster ride of recurring psychotic episodes, trips to the local hospital psych ward, return stays at the state hospital, and then trips back to the adult homes, it is clear to me he would have been much better off if he had stayed in a full hospital or nursing home-like setting, where he would have been more closely supervised. We will never have true health care reform until the IMD Exclusion is repealed, expanding coverage for long-term care to include persons with mental illnesses.