Our knowledge about the extent and characteristics of suicide attempts and deliberate self-harm among young people is based mainly on two types of data: hospital admissions and surveys. Hospital admission rates suggest that 150–300 per 100,000 adolescents and young adults are hospitalized per year after attempted suicide (
1 ). Surveys among adolescents have shown that the proportion reporting deliberate self-harm within the past year has been around 3%–7% (
2,
3,
4,
5 ). This corresponds to a rate per 100,000 that is 20 to 50 times higher than the hospital admission rates. In addition, survey studies showed that only a small proportion (4%–15%) of adolescents who reported deliberate self-harm had also sought medical care after their self-injury (
2,
3,
4,
6,
7 ). Thus adolescents who receive treatment or help after deliberate self-harm may be considered to be "the tip of the iceberg."
A few studies have addressed whether suicide attempters who seek medical care after self-harm differ from those who do not. In the Child and Adolescent Self-Harm in Europe project, hospital admission after deliberate self-harm was more often reported among those who had taken an overdose of pills than among those who had cut themselves (
2,
3,
4 ). Grøholt and colleagues (
8 ) found that mental health problems and disruptive disorder combined with substance use were more prevalent among adolescents admitted to a hospital after a suicide attempt than among survey respondents who reported attempted suicide but were not admitted to a hospital. This may suggest that the more severe cases of deliberate self-harm among adolescents tend to be seen by medical services, but for the majority of such events, the young person does not receive any medical attention.
The likelihood that young people seek professional help for mental health problems or distress is generally low (
9 ). Jorm and colleagues (
10 ) found that in the case of a mental health problem, only a small proportion of adolescents (12–17 years) would seek help from a general practitioner or mental health specialist, whereas half would turn to their family for help. Among young adults with suicidal thoughts, about one-third had sought any help in the previous four weeks, and a larger proportion sought help from informal sources (for example, family and friends) than from professional sources (for example, general practitioners and counselors) (
11 ). Gould and colleagues (
12 ) found that teenagers with depression, substance use problems, and suicidal thoughts were more likely than teenagers without such problems to report maladaptive coping and help-seeking strategies. Carlton and Deane (
9 ) reported that adolescents with suicidal ideation had lower levels of help-seeking intentions than others.
A school survey in Norway showed that relatively few adolescents had sought any professional help after attempted suicide; however, a significant proportion had received help from friends, parents, or other family members (
6 ). Since 1994 various societal changes have occurred in Norway that may have changed the extent to which adolescents receive help or treatment after attempted suicide. The capacity of child and adolescent psychiatric outpatient services has increased by 75%, although this is counteracted by a 25% increase in the child and adolescent population (
13 ). A national action plan to prevent suicide was launched in 1994 that emphasized aftercare for suicide attempters and competence building for health and social care professionals (
14 ). Between 1992 and 2002, Norwegian youths have reported better relationships with friends and parents (
15,
16 ). Suicide and deliberate self-harm have received increased attention in the media, as measured by the relative number of Norwegian newspaper articles dealing with this topic (
13 ). Indeed, there were 2.2 times as many children and adolescents referred to specialist mental health care because of suicide risk in 2001 as there were in 1992 (
13 ); however, only a slight increase in self-reported suicide attempts among adolescents occurred in that period (
15 ), suggesting an increased inclination to receive professional help for problems related to deliberate self-harm.
Using data from two large school surveys in 1994 and 2002, this study assessed whether receiving help after deliberate self-harm among adolescents has changed over this period as a result of significant changes in service provision and media attention and, if so, whether individual predictors of receiving help may aid in explaining these changes.
Methods
Participants
This study is based on two school surveys, conducted in 1994 and 2002. In 1994, 9,679 students from 63 schools in grades 8 through 12 (ages 14 to 19) were invited to participate in the 1994 Young in Norway Study (
17 ). In 2002, another sample of 12,923 students aged 13 to 19 years from 73 schools were invited to participate in the 2002 Young in Norway Study (
18 ). Informed consent from all students, informed written parental consent for students in grades 7 through 9, and informed passive parental consent for all other students younger than 18 years were a prerequisite for participation. The surveys were approved by the Norwegian Social Science Data Services. Data collection procedures were identical in the two surveys. They are described in more detail elsewhere (
15 ).
The response rate was 77% (N=7,463) in the 1994 survey and 90% (N=11,694) in the 2002 survey. Seventeen students in 1994 and 16 students in 2002 were excluded because they had obviously given incorrect or humorous responses; therefore, the final sample was 7,446 in 1994 and 11,678 in 2002. In the 1994 sample the mean±SD age was 17.1±1.9 years and 53% (N=3,962) of the respondents were girls, whereas in the 2002 sample the mean age was 15.8±1.9 years and 51% of the valid responses (N=5,784) were girls. Only a small proportion of the respondents had an immigrant background from non-Western countries (N=166, or 2%, in the 1994 survey and N=670, or 6%, in the 2002 survey). In both surveys the students were asked, "Have you ever deliberately taken an overdose of pills or otherwise tried to harm yourself?" Those who responded affirmatively to this question constituted the subsample applied in the analyses presented here: 560 students in the 1994 survey (8% of the valid responses) and 1,033 students in the 2002 survey (9% of the valid responses). The framing of the question on deliberate self-harm implied that we addressed self-harm behaviors both with and without suicidal intent.
Instruments
Help or treatment after deliberate self-harm. Those who answered affirmatively to the question on lifetime prevalence of deliberate self-harm were asked, "Did you afterwards receive help or treatment?" Responses included in a hospital or with a medical doctor, with a psychologist or psychiatrist, by parents or another person in my family, by friends, by others, or did not receive help or treatment from anyone. The number of sources of help or treatment was constructed as a sum score (range 0–5). In the 1994 survey, 414 (74%) of the students who reported deliberate self-harm gave at least one response to the help or treatment questions, whereas in the 2002 survey almost all (N=1,012, 98%) of those who reported deliberate self-harm responded to these questions. Furthermore, internal consistency was checked. Those who stated that they had received help or treatment from one or several sources and also stated that they had not received help or treatment from anyone (three in 1994 and 22 in 2002) were treated as missing responses. Thus the analyses were based on respondents who had valid responses on the help or treatment variables (411 in 1994 and 990 in 2002).
Independent variables. A six-item measure of past-week depressive symptoms from the Johns Hopkins Symptom Checklist (SCL-90) (
19 ) was used (
20 ). Possible scores ranged from 1.0 to 4.0, with higher scores indicating more symptoms of depression. Attachment to parents was measured with three items from the care dimension of the Parental Bonding Instrument (
21 ). Possible scores range from 1.0 to 4.0, with higher scores indicating better parental attachment. A single item—"Do you feel lonely?"—was dichotomized, separating those who responded "never" from those who responded "seldom," "occasionally," or "often." A history of suicide attempt was assessed by the question, "Have you ever tried to take your own life?" (yes or no). Living arrangement was dichotomized, separating students who were living with both parents and those who were not. Measures of the frequency of the two most commonly used intoxicants, alcohol and cannabis, were included as semicontinuous variables applying midpoint values.
Statistical analyses
Bivariate associations between sources of help or treatment after deliberate self-harm and survey year and other independent variables were assessed with cross-tabulations and tested with chi square statistics. Differences in the distribution of the number of sources for help or treatment between the two survey years were tested with t tests. The likelihood of having received help or treatment from professional sources and from informal sources and of not having received any help or treatment were estimated in logistic regression models. Survey year was entered into the model in the first step with age of respondent, because the age composition of the two samples varied. The other independent variables—gender, depressive symptoms, parental attachment, loneliness, history of suicide attempt, living arrangement and substance use—were entered into the model in a stepwise forward procedure based on model fit criteria (log-likelihood ratio). In addition, a linear regression model was estimated to assess whether the number of sources of help or treatment had changed from 1994 to 2002 when age and other relevant covariates were controlled for and moreover to explore the relative impact of other factors on the number of sources for help or treatment. Survey year and age of respondents were entered into the model in the first step, then the other variables were entered in a stepwise forward procedure based on model fit criteria. All statistical analyses were conducted using SPSS, version 17.0.
Results
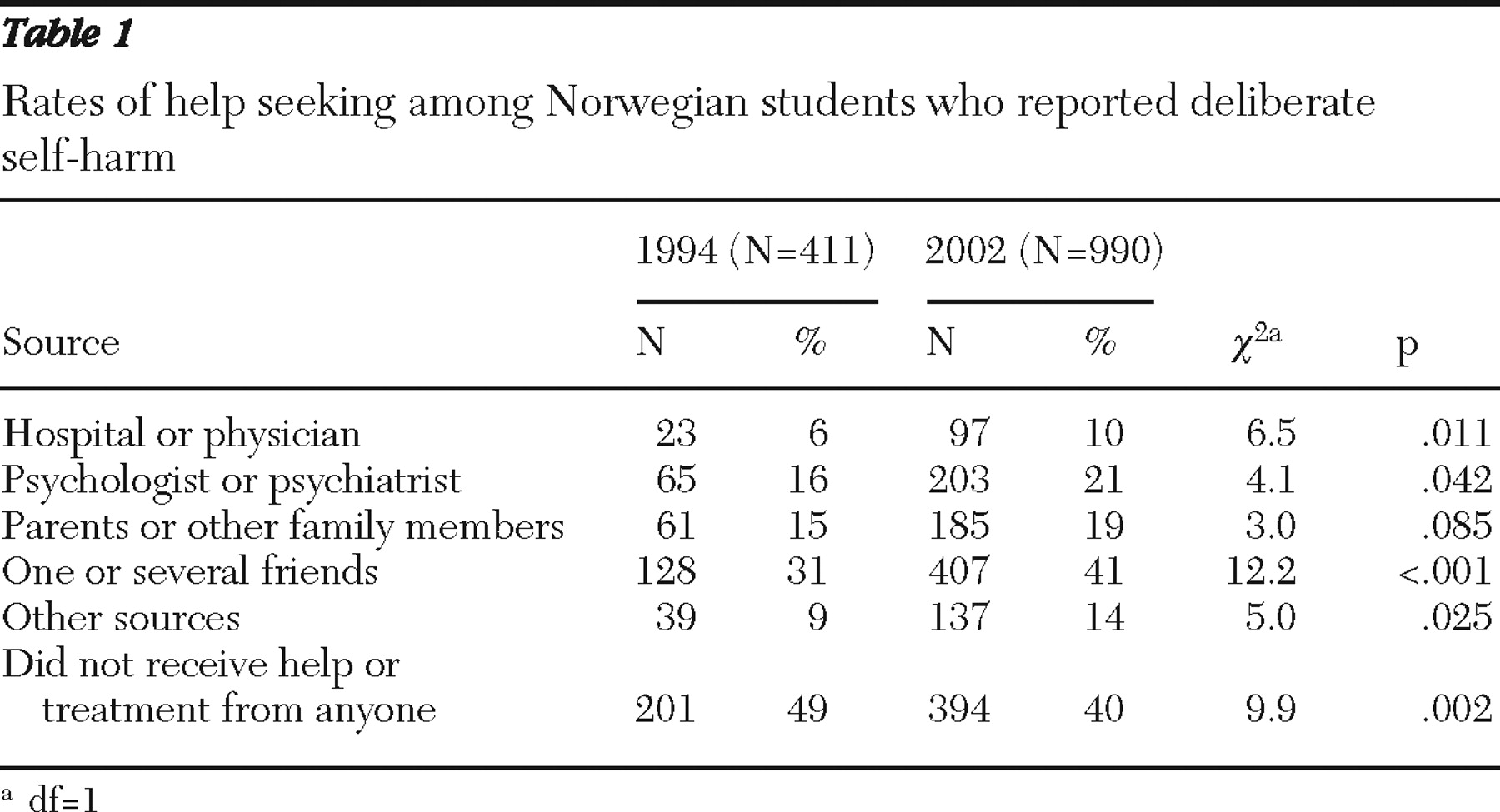
The proportion of students who had received help or treatment after deliberate self-harm significantly increased from 1994 to 2002 for all categories of help providers except for the category of parents or other family members, whereas the proportion that had not received any help or treatment afterwards decreased significantly (
Table 1 ). Sources of help or treatment were collapsed into three broad categories: professional help (hospital, physician, and psychologist or psychiatrist), informal help (parents, family, and friends), and no help. The proportion that received professional help increased from 19% (N=77) in 1994 to 25% (N=248) in 2002, and the proportion that received informal help increased from 43% (N=177) in 1994 to 50% (N=498) in 2002. Having received professional help was more often reported among those who had also received help from informal sources, and this proportion increased from 44 of 177 (25%) in 1994 to 156 of 498 (31%) in 2002. The number of sources from which the respondents had received help or treatment increased from 1994 to 2002: 68 (16%) had received help or treatment from two or more sources in 1994, and this was reported by 282 (28%) in 2002. On average the number of sources was .77 in 1994 and 1.03 in 2002 (t=-4.50, df=1, p<.001).
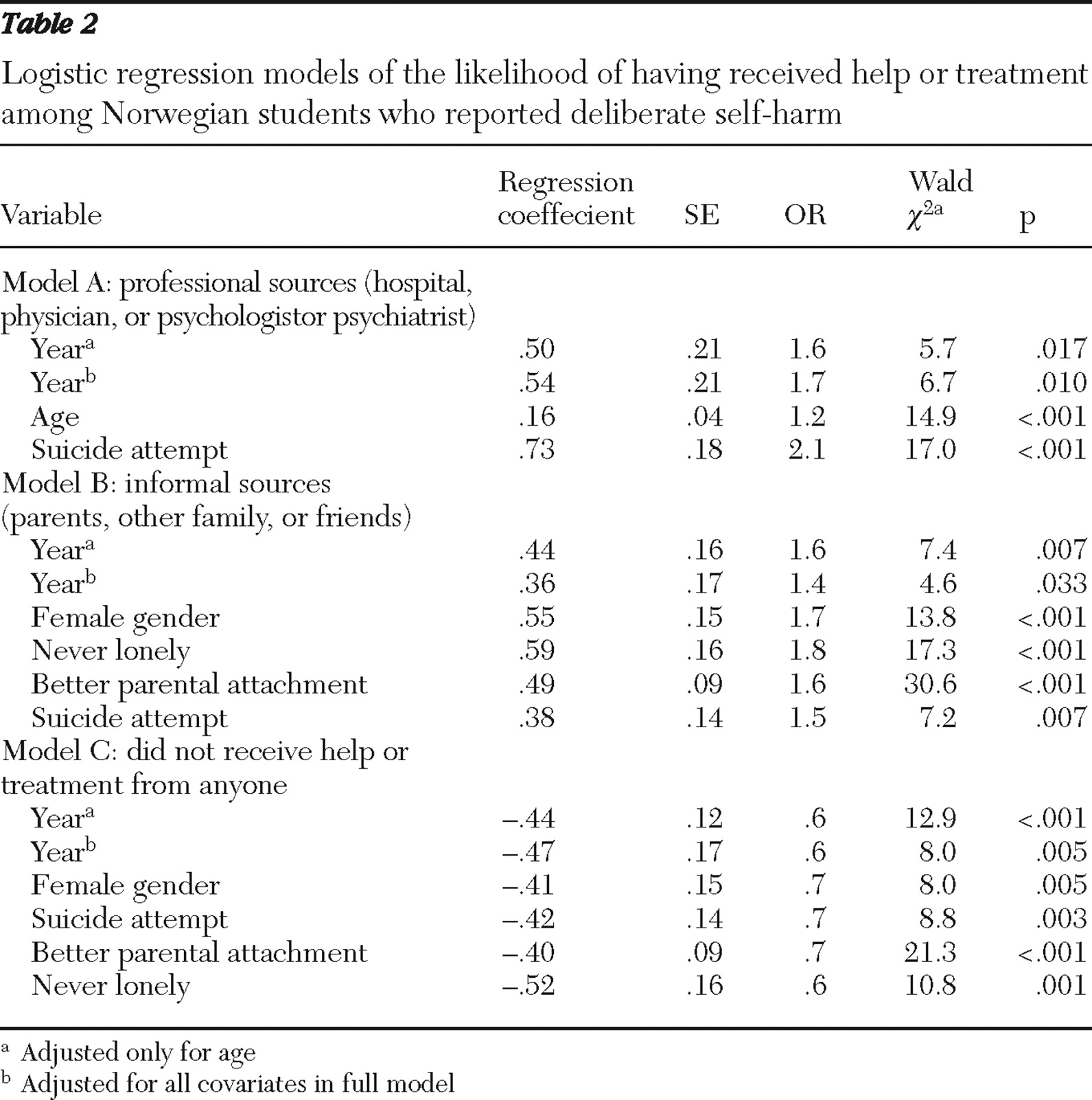
Logistic regression analyses showed that after controlling for covariates, the likelihood of having received professional help after deliberate self-harm increased by about 70% (OR=1.7) over the eight-year period. Moreover, the likelihood of having received help from professional sources increased with age and history of suicide attempt. The likelihood of having received help from informal sources, such as parents, other family members, and friends, increased by about 40% (OR=1.4). Moreover, girls were more likely to have received informal help, as were those who reported better parental attachment, those with a suicide attempt, and those who never felt lonely (
Table 2 ). Taking age and other individual characteristics into account, multivariate analyses confirmed that the likelihood of having not received any help or treatment after deliberate self-harm decreased (OR=.6) from 1994 to 2002. Boys were more likely to report that they had not received any help or treatment, as were those with poorer parental attachment and those with no history of a suicide attempt (
Table 2 ). The extent to which receiving help changed over the eight-year period was hardly affected by changes in individual characteristics assessed in this study—that is, controlling for these variables did not alter the association between year and receiving help significantly. Moreover, changes in receiving help did not differ significantly between those with and without a suicide attempt when tested by interaction terms in logistic regression models.
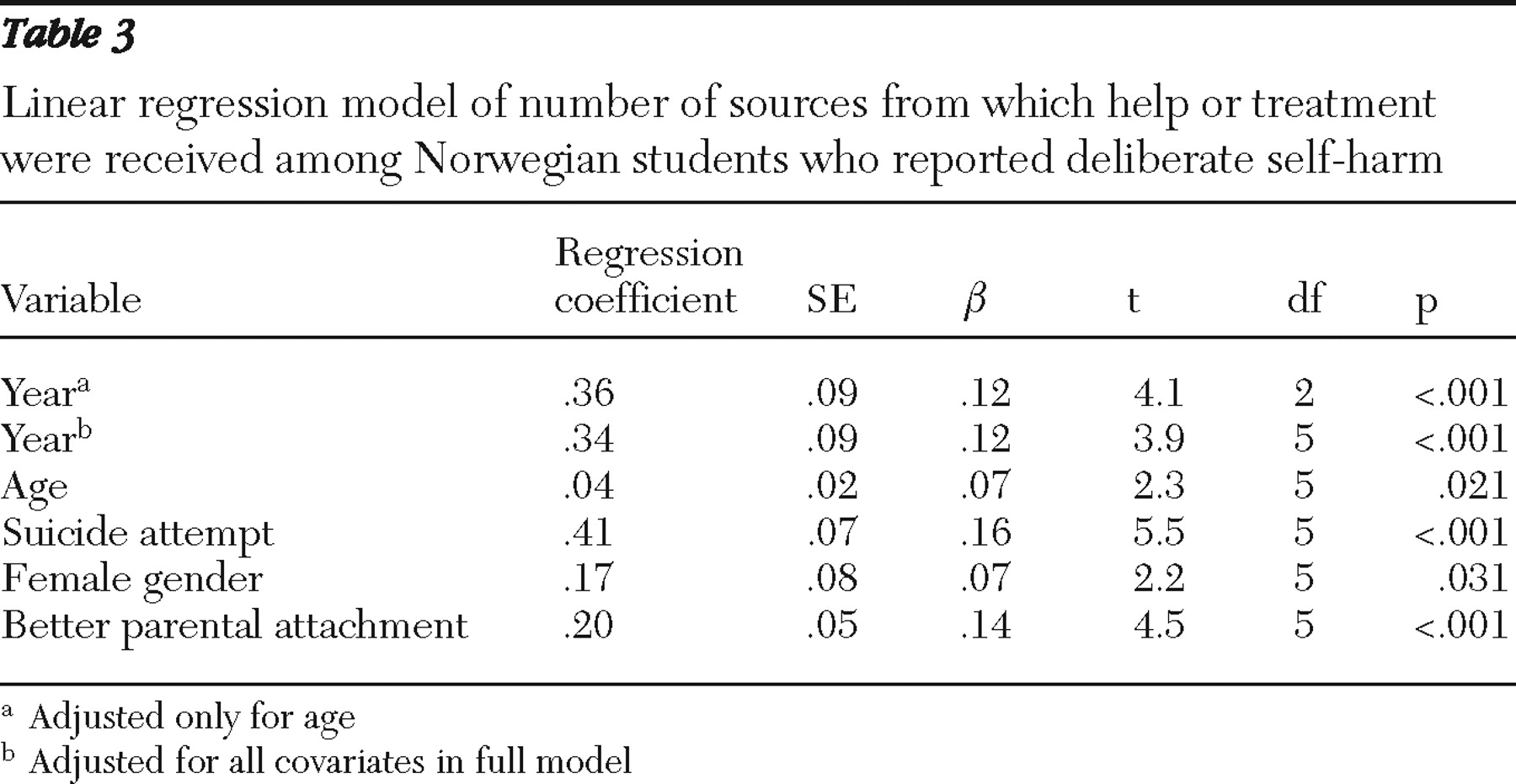
Linear regression analysis further confirmed that the average number of sources of help or treatment increased over the study period, after we controlled for age differences and other independent variables. Moreover, the analyses showed that having received help or treatment from multiple sources was more often reported by girls, those with a suicide attempt, and those with better parental attachment (
Table 3 ).
Discussion
Some previous population-based studies have addressed the extent to which people seek or receive help after deliberate self-harm (
6,
7,
22 ). The study presented here adds to this literature and shows that the proportions that had received professional help and help from informal sources increased significantly from 1994 to 2002. The proportion that had received help or treatment from multiple sources also increased over the period, whereas the proportion that had not received any help or treatment decreased. In line with previous studies (
6,
7,
22 ), our study found that only a minority of students who had deliberately harmed themselves (that is, one in four) had received help or treatment from medical services afterwards, whereas a significantly larger proportion had received help from informal sources such as family or friends. We also found that having received help from professional sources increased with age. Correspondingly, Jorm and colleagues (
10 ) found that intention to seek help for mental disorders from professional sources increased with age. In line with findings from a recent study (
22 ), our study findings also showed that a history of suicide attempt increased the likelihood of having received help or treatment from professional sources and from informal sources, and furthermore we found that those who had better parental attachment and those who were not feeling lonely were more likely to have received help from family and friends and less likely to have not received any help or treatment.
Several changes occurred in Norwegian society between 1994 and 2002 that could have affected the extent to which adolescents receive help after deliberate self-harm. First, over this period more adolescents received help for mental health problems, both within the specialist mental health services and at the community level (
13 ). One could therefore have anticipated that, compared with 1994, in 2002 a higher proportion of adolescents were already receiving treatment at the time of the self-harm event and therefore had better access to help. However, the number of adolescents referred to specialist mental health care for deliberate self-harm amounts to only .16% of the adolescent population in Norway. Hence, this may at best explain a small fraction of the increase in the proportion receiving professional help. Second, there was a national action plan to prevent suicide during this period, and this plan emphasized competence building for health and social care professionals. Whether this measure can help to explain the increase in the proportion of young people receiving help cannot be substantiated by this study and remains only a possibility. Third, although adolescents reported better relationships with parents and more alcohol and drug use over this period, our analyses showed that these factors did not seem to explain changes over time in the likelihood of receiving help. Fourth, increased media attention about deliberate self-harm may have reduced the barriers to help seeking and strengthened the enabling factors to seek help (
23,
24,
25 ). Moreover, fear of stigma is among the most frequently reported reasons for not seeking help among suicidal adolescents (
26 ). Thus it is possible that more accepting attitudes toward psychiatric problems in general and deliberate self-harm in particular may lead to increased help seeking and thereby result in an increase in receiving help. Adolescents, particularly young adolescents, often rely on others, such as friends, family, and teachers, to instigate or assist in the formal help-seeking process. Our finding that adolescents who received help from family and friends were also more likely to seek help from professional sources is in accordance with this.
A significant strength of this study is that the extent to which adolescent self-harmers received help was assessed by identical measures in two large-sample national surveys covering a period when significant changes in service provision and norm climate have occurred. On the other hand, it should be noted that in the 1994 survey a significant proportion of those reporting deliberate self-harm did not respond to the questions on treatment and help-seeking behavior. Because all calculations were based on valid observations, affirmative responses to having received help or treatment accounted for a relatively larger proportion in the 1994 survey than in the 2002 survey, implying that the estimated changes from 1994 to 2002 may be somewhat deflated. Another methodological issue is the question of how the adolescents interpreted the questions on receiving help. It is possible that some respondents may have been in contact with health services after the event of deliberate self-harm, yet they may not have responded affirmatively because they felt that they were not helped. In that case, the proportion of adolescents who had been in contact with health services after deliberate self-harm may be larger than our estimates indicate. The construct validity of help-seeking behavior after deliberate self-harm thus needs to be addressed in further studies. There are clearly many factors at the individual and societal levels that may affect the extent to which adolescent self-harmers receive help that may be difficult to assess and disentangle in a study. The data used in the research presented here were not primarily collected for this purpose, and thus attempts at explaining the observed changes over time can be only suggestive. Moreover, given the few empirical studies in this area, there is a need for external validation of our study results in future studies.
Conclusions
Only a minor proportion of adolescents seems to be reached by health services after deliberate self-harm events. Individual characteristics, such as male gender and poorer parental attachment, increased the likelihood of not receiving any help or treatment after such events. Yet this Norwegian study seems to suggest that factors also at the societal level may contribute to reducing barriers to receiving help in this group of vulnerable young people.
Acknowledgments and disclosures
This study was funded by the Norwegian Research Council, Norwegian Social Research, the Norwegian Centre for Suicide Research and Prevention, the University of Oslo, the Norwegian Institute for Alcohol and Drug Research, and the Department of Psychology at the Norwegian University of Science and Technology.
The authors report no competing interests.