Numerous studies have demonstrated high rates of mental illness and substance abuse among homeless persons (
1,
2). Others have linked homelessness to criminal activity and to being a victim of crime (
3,
4,
5,
6). Still others have demonstrated a relationship between victimization and mental illness, both among persons who are homeless (
3,
7) and in the general population (
8).
This paper addresses the prevalence, correlates, and consequences of criminal victimization among a subset of homeless persons who are arguably the most vulnerable of all—those with serious mental illnesses. In addition, we explore the predictive relationship between recent victimization and a number of health and social outcomes, including future victimization, for a group of homeless mentally ill clients enrolled in the Access to Community Care and Effective Services and Supports (ACCESS) program of the Center for Mental Health Services.
Fischer's extensive review of the literature (
3) about the incidence of victimization among homeless people concluded that rates of victimization are high in samples of homeless people compared with the general population. Although summary rates are difficult to determine due to variability between studies in sampling frames, definitions of victimization, and time frames for reporting incidents of victimization, reported rates for a six-month to one-year period range from one-third to two-thirds of those surveyed.
Likewise, Link and associates (
6) found that 42 percent of the respondents they interviewed who had experienced literal homelessness reported having experienced one or more types of victimization. By comparison, they found that 11 percent of respondents who had lived doubled up temporarily with friends or relatives at some point in their lives reported victimization, a further indication that people who are living on the streets and in shelters are at much higher risk of victimization than even the doubled-up poor, much less the general population.
Fischer (
3) further concluded that individual risk for victimization varies according to demographic and psychosocial characteristics. Most important among these risk factors are gender, substance use, and psychiatric status. Poor physical health and a criminal record are also reported to be risk factors for victimization.
This study used baseline assessment data from nearly 2,000 homeless persons with serious mental illness participating in the first year of the Center for Mental Health Services' ACCESS program (
9). Launched in 1994, ACCESS is an 18-site, five-year demonstration program designed to examine the influence of service system integration on the use of services and quality of life of homeless people with serious mental illness (
10). All sites participating in the ACCESS demonstration were provided funds to establish two types of interventions: specialized outreach teams that would make contact with untreated homeless people with severe mental illnesses and facilitate their involvement in more intensive services, and intensive case management teams to provide comprehensive services for up to one year to a minimum of 100 new consumers each year.
ACCESS programs were implemented during 1994 in 18 communities in 15 cities in the U.S.: Bridgeport and New Haven, Connecticut; the Edgewater-Uptown and the Lincoln Park-Near North areas of Chicago; Topeka and Wichita, Kansas; St. Louis and Kansas City, Missouri; Raleigh and Charlotte, North Carolina; West Philadelphia and Center City Philadelphia; Fort Worth and Austin, Texas; Richmond and Hampton-Newport News, Virginia; and Uptown Seattle and Downtown Seattle, Washington.
The study reported here used the baseline assessment data from ACCESS program participants to examine the epidemiology of victimization among homeless persons with serious mental illness along with sociodemographic and clinical predictors of the risk of victimization for this group. Then, using follow-up data collected at three and 12 months after baseline from the same clients, we examined the relationship between reported levels of victimization at baseline and a number of important outcome indicators, including homelessness, psychiatric status, and quality of life. Finally, we examined the extent to which having been a victim at baseline was predictive of further victimization at each follow-up point.
Methods
Sources of data and eligibility criteria
Data on client characteristics and victimization were obtained from several sources. Contact and referral forms completed by outreach clinicians at the time of the first outreach contact and referral of the client to case management provided data on whether the client was contacted through ACCESS outreach or referred from another program, the duration of the outreach period, and psychiatric diagnoses. An intake form was used to determine eligibility for the ACCESS program and to record self-reported levels of psychiatric distress as well as interviewers' observations of overtly disturbed behavior by clients. A baseline form, completed at the client's enrollment in case management services, was used to collect self-reported data on sociodemographic characteristics, housing, substance use, length of time homeless, physical health status, levels of social support, employment, income, criminal involvement, quality of life, and victimization experiences. A follow-up form, completed three and 12 months after baseline, was used to gather follow-up data on baseline measures.
Clients were eligible for ACCESS case management services if they were homeless, suffered from severe mental illness, and were not involved in ongoing community treatment. Entry criteria have been described in detail elsewhere (
11,
12). To meet the homelessness criterion, at the time of first contact with ACCESS staff the client had to have spent at least seven of the past 14 nights in a shelter, outdoors, or in a public or abandoned building.
Psychiatric eligibility was determined with a screening algorithm developed for a previous outreach demonstration project for homeless people with severe mental illness (
13). Self-report scales addressed symptoms of depression, psychosis, and mania and functional capacity, and a series of interviewer observations addressed overtly disturbed behavior of various types, such as delusions, agitation, and incoherence. Validation of this algorithm using the Structured Clinical Interview for Diagnosis as a diagnostic gold standard has demonstrated 91 percent sensitivity, that is, correct identification of persons with axis I psychiatric disorders that were not related to substance abuse (
13).
Clients who met eligibility criteria were invited to participate in the ACCESS demonstration, and those who gave informed consent were evaluated during a comprehensive baseline interview. Eligibility screening and baseline interviews were administered by specially trained interviewers who were not involved in the delivery of clinical services.
Measures
Victimization was operationalized in several ways. One series of items asked whether, in the past two months, the client had been the victim of a robbery by force; theft of property; threats with a gun, knife, or other weapon; a beating with fists, club, or other heavy object; or sexual assault. Two summary items were also constructed: the proportion of clients who had experienced at least one form of victimization and the sum of the types of victimization experienced (a range of 0 to 5).
Predictor variables included in the analysis were gender, with a dummy variable representing male gender; age; race, with two dummy variables representing African American and Latino; level of social support, as measured by the number of types of people the client could count on for a loan, ride to an appointment, or help with an emotional crisis; psychiatric status, assessed by self-reported symptoms of depression (
14) and psychosis (
15); substance use, including both the number of days the client drank to intoxication in the previous 30 days and the total number of days of illegal drug use in the past 30 days; literal homelessness, measured by the number of days the client spent outdoors, in a shelter, or in a public or abandoned building in the past 60 days; employment, measured by the number of days the client worked in the past 30 days; and criminal history, or whether the client had ever been convicted of a crime.
Analyses
Analyses were conducted in several stages. First, multiple regression analyses were conducted to test the significance of relationships between sociodemographic, health status, and social adjustment variables and each of five types of victimization as well as two summary variables. Logistic regression was used with the dichotomous dependent variables reflecting various types of victimization (robbery, theft, weapons threats, beating, and sexual assault) and a composite variable representing the reporting of one or more forms of victimization. Ordinary least-squares regression was used with the continuous dependent variable of the total number of types of victimization reported.
Second, a series of multiple regression analyses was conducted to determine the influence of recent victimization at the time of program entry on several clinical and social adjustment outcome variables considered of central importance. The variables were depressive and psychotic symptoms, drug and alcohol abuse, literal homelessness, employment, and social support. To minimize the confounding effects of differences in baseline status on these variables, the baseline value was included in the appropriate model as a covariate.
Finally, multiple regression was again used to measure the relative effects of recent victimization at baseline on victimization at each of the follow-up points, controlling for other important predictor variables.
Results
Sample characteristics
A total of 5,796 consumers were contacted through outreach or referral during the first year of the ACCESS program (May 1994 to May 1995). Of those contacted, 2,291 were referred for case management evaluation (39.5 percent of those initially contacted). Of those referred, 1,943 were determined to be eligible (84.8 percent), and 1,839 gave informed consent to participate and completed baseline assessments (95 percent of eligible consumers; mean±SD=102±15.7 clients per site).
A total of 1,535 clients (84 percent) were successfully contacted at three-month follow-up, 1,449 (79 percent) at 12 months, and 1,340 (73 percent) at both time points. Clients successfully interviewed at three and 12 months were compared with those who were not interviewed on 25 baseline measures and differed significantly on only three. Details of this analysis are provided elsewhere (
11,
12).
Clients averaged 38.6±9.4 years of age. A total of 65.2 percent were male, 44.5 percent were African American, and 5.2 percent were Latino. All clients received at least one clinical psychiatric diagnosis. In order of frequency, the nonmutually exclusive diagnoses were major depression for 50 percent, schizophrenia for 34 percent, other psychoses for 30 percent, personality disorder for 25 percent, anxiety disorder for 19 percent, and bipolar disorder for 18 percent. Sixty-two percent of the clients received a diagnosis of a psychotic disorder, such as schizophrenia, other psychoses, or bipolar disorder. The mean±SD score on the depression scale was 3.3±1.9 of a possible 5 points. The mean±SD psychosis score was 11.8±9.6 of a possible 40 points. The mean±SD score for interviewers' observations of overtly disturbed behavior was 11±8.7 of a possible 52 points.
Substance abuse diagnoses were frequent. Forty-seven percent of the clients met criteria for alcohol abuse and 38 percent for drug abuse. Clients drank alcohol to the point of intoxication an average of 2.4±6.1 days per month and used illegal drugs an average of 3.8±11.2 days. (Days of drug use could total more than 30, as clients may have used more than one drug per day.)
Level of social support—the average of the total number of types of people who would help the client with a loan, ride, or emotional crisis—was 1.9±2.3 of a possible 18. At baseline, clients had spent an average of 39.5±21.1 of the past 60 days literally homeless, worked an average of 1.9±5 of the past 30 days, and reported a monthly average income of $325.41±428.32.
Victimization and associated variables
Of the 1,839 ACCESS clients participating in the study, 44.1 percent were the victims of at least one of the following crimes during the two months before the baseline interview: robbery by force (13.3 percent), theft of property (28.6 percent), threat with a weapon (18.4 percent), physical beating (15.6 percent), or sexual assault (6.2 percent). The mean±SD number of types of victimization experienced by ACCESS clients during this time period was .82±1.16.
Significant gender differences were found in the reporting of some of the types of victimization, most notably sexual assault, with only 1.3 percent of men reporting sexual assault, compared with 15.3 percent of women (χ2=139.28, df=1, p<.001). Women were also significantly more likely to report being beaten with fists, a club, or another heavy object (20.6 percent versus 12.9 percent for men; χ2=18.39, df=1, p<.001). In addition, women were significantly more likely to report having experienced any of the five forms of victimization considered in the analysis in the past two months (49.4 percent, compared with 41.3 percent for men; χ2=10.90, df=1, p<.001), and women reported a significantly higher number of types of victimization (an average of .96± 1.25, compared with .75± 1.11 for men; t=3.58, df=1,174, p<.001). No significant gender differences were found in reporting of robbery by force (12.7 percent for women and 13.6 percent for men), theft of property (27.9 percent for women and 28.9 percent for men), and threats with a weapon (19.3 percent for women and 17.9 percent for men).
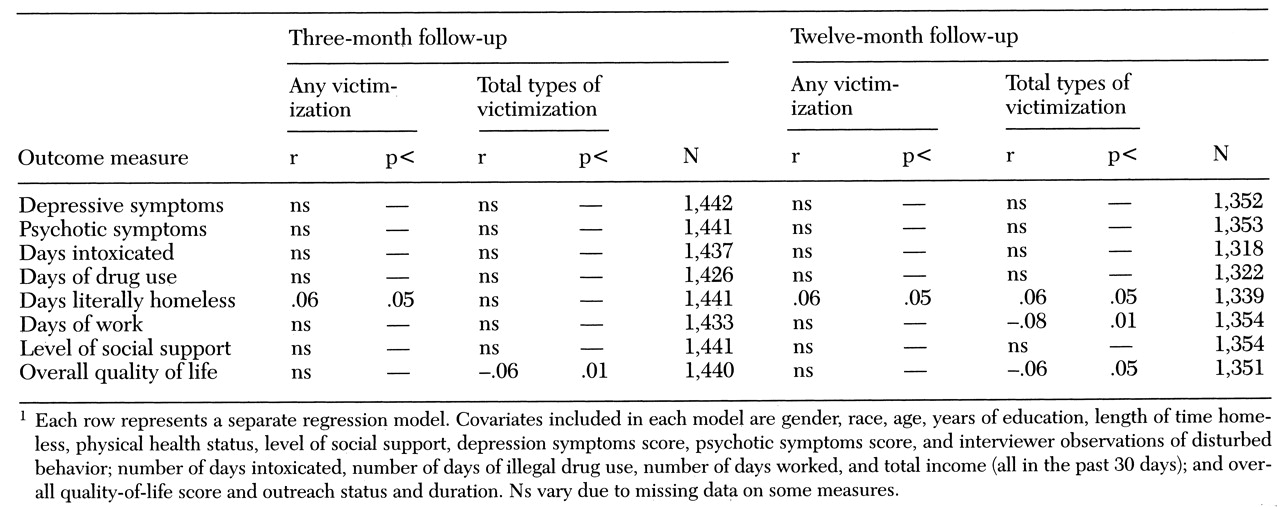
Multivariate analyses examining the associations between client characteristics and victimization are shown in
Table 1. Six variables were significantly associated with three or more types of victimization: gender, race, employment, criminal conviction, alcohol use, and severity of psychotic symptoms. Men were less likely than women to have been the victims of weapons threats, beatings, sexual assault, and any form of victimization, and men reported fewer total types of victimization. African Americans were less likely than other racial groups to report theft of property and any victimization, and they also reported fewer types of victimization. Employment was positively associated with weapons threats, any victimization, and the number of types of victimization reported.
Criminal conviction, alcohol use, and severity of psychotic symptoms were all positively associated with five or more of the measures of victimization. Having been convicted of a crime was associated with being the victim of robbery, weapon threats, beatings, any victimization, and the number of types of victimization reported. The number of days a client drank alcohol to intoxication was positively associated with all types of victimization except sexual assault. Reported psychotic symptoms was also positively associated with all types of victimization except for theft of property.
Because both the summary variables (any victimization and number of types of victimization) included sexual assault, which was so clearly linked to gender, we recomputed these variables omitting sexual assault. As we expected, when sexual assault was excluded, the significant difference between males and females found at the bivariate level disappeared for the summary variable, the total number of types of victimization reported. However, a marginally significant difference remained for the other summary variable, any victimization (40.6 percent for male clients compared with 45.7 percent for female clients; χ2=4.45, df=1, p<.04).
We conducted additional regression analyses using the two dependent variables that exclude sexual assault and the same set of predictors described above to see if the relationship patterns would differ. The results did not differ from those obtained using the victimization variables with sexual assault included.
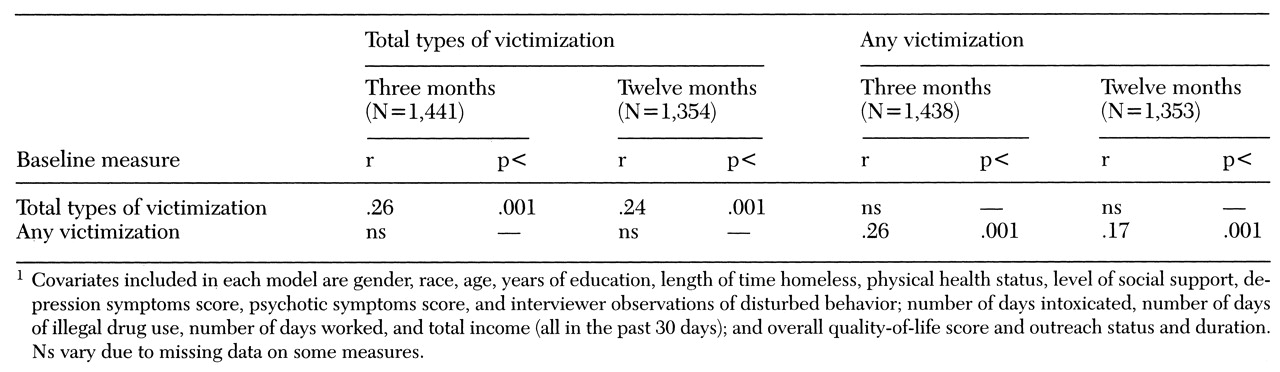
Victimization and client outcomes
Table 2 shows that neither summary measure of victimization was predictive of outcome for most variables at either three or 12 months after the baseline interview. However, some notable exceptions were found. At three and 12 months, victimization was significantly and positively related to the number of days the client was literally homeless. Clients who had been recently victimized at the time of the baseline interview reported spending more time on the streets and in shelters at the time of the follow-up interviews at three and 12 months.
Overall quality of life at both the three- and 12-month follow-up points was negatively correlated with the number of types of victimization reported at baseline. The number of types of victimization was also negatively correlated with the client's employment, with the number of days worked decreasing as the number of types of victimization increased.
Table 3 shows that having been recently victimized at baseline was the single most important predictor of victimization at both three and 12 months after baseline, regardless of the measure of victimization and independent of the other predictors. This finding emerged both in analysis of the total sample and in separate regression analyses using data for men and for women.
Discussion and conclusions
Criminal victimization is a serious and pervasive problem for people who are homeless and seriously mentally ill. Nearly two of five ACCESS clients included in this study were the victims of at least one crime during the two months before entering the program. Women were even more likely than men to have been victims, with half of the women reporting having experienced at least one of the five types of crime considered in the analysis.
As we would expect, given the documented link between victimization and mental illness, this population appears to have substantially higher rates of victimization than other samples of homeless persons. The rates found among the ACCESS population appear especially high given the 60-day time frame for reporting victimizations compared with the time frames of six months, one year, and lifetime used in other studies. Our findings further indicate that severity of mental illness, alcohol consumption, and criminal history are all strongly associated with victimization.
The relationship between employment and victimization is noteworthy. The more days a client had worked in the past month, the more likely he or she was to have been a recent crime victim. This association may be due to the fact that workers are more likely to be carrying money and thus to be targets of crime. In addition, we found that clients who reported more types of victimization before program entry were significantly less likely to be employed a year later. Some homeless clients appear to be caught in a no-win situation whereby if they work they may be victimized, and if they are victimized they may not be able to work.
Past victimization has a significant impact on two important areas of client outcome—the amount of time the client lives on the streets or in shelters and the client's quality of life. Both of these areas are targeted for improvement by the ACCESS project. Securing stable housing for people who are homeless and seriously mentally ill is perhaps the most important client-level goal of the ACCESS program. The fact that victimization has an effect on homelessness independent of the other variables included in the model suggests that service providers who work with this population should assess the extent of victimization clients have suffered and work with clients on issues related to victimization, including safety and self-esteem in addition to psychiatric and substance abuse issues. As Fischer (
3) pointed out, the effect of violence goes beyond the physical consequences and includes "psychological demoralization and the ever-present fear and distrust of others frequently reported by homeless people." Addressing these issues should also have some impact on the client's quality of life.
We have provided some evidence that victimization perpetuates homelessness, lowers self-rated quality of life, and decreases the likelihood of employment. We also have shown that current victimization is predictive of future victimization. The data paint a picture in which clients with the most severe psychiatric symptoms, substance abuse problems, and criminal histories are caught in a vicious, reinforcing cycle of victimization and homelessness. Breaking this cycle must be an important part of the work service providers do with clients who are homeless and mentally ill.
Acknowledgments
This study was funded by interagency agreement AM9512200A between the Department of Health and Human Services, Center for Mental Health Services, and the VA Northeast Program Evaluation Center. The authors thank the following persons for assistance with data collection: Simeon Goodwin, Ph.D., Jacob Tebes, Ph.D., Mardi Solomon, M.A., Sue Pickett, Ph.D., Greg Meissen, Ph.D., Robert Calsyn, Ph.D., Phyllis White, M.A., Cheryl Roberts, M.A., Coleman Poses, M.S.W., Laverne Knezek, Ph.D., Deborah Webb, Ph.D., Marilyn Biggerstaff, D.S.W., and Peter Brissing, M.S.W. The authors also thank Cindy Cushing, Michele D'Amico, and Jennifer Cahill for assistance in processing the data.