The majority of patients with diagnosable disorders do not seek mental health treatment, and those who do frequently fail to follow through (
1,
2). The identification of patient variables that predict attendance and treatment adherence and of system factors that constitute barriers to care has become of greater concern as managed care increases pressure on providers to demonstrate cost-effectiveness and as researchers apply treatments of known efficacy to more diverse "real-world" populations.
The influences of patient characteristics, system characteristics, and illness characteristics in predicting who uses clinical mental health services have all been emphasized (
3). Some studies suggest a relationship between treatment attendance and demographic variables; other authors suggest that factors related to the accessibility of the treatment system, such as location, length of wait lists, and hours, are crucial (
4,
5,
6).
Most studies addressing attendance problems have been based in academic medical centers, and very few have investigated rural services, despite the fact that almost 21 percent of Americans live in nonmetropolitan areas and 55 percent of U.S. counties are rural (
7). The nature of the mental health service system in rural areas remains largely unknown (
8,
9). A better understanding of characteristics of rural patients seeking mental health services and of predictors of treatment engagement in this population is clearly needed.
The purpose of this chart review study was to determine whether patient, system, and illness characteristics predicted patients' return for at least one treatment visit after an assessment appointment at a rural community mental health center.
Methods
Setting and subjects
The base service unit of Beaver County (Penn.) Mental Health and Mental Retardation assesses all patients requesting mental health services and refers patients to a related clinic. The assessment is an interview with an experienced clinician and a psychiatrist who addresses the presenting complaint, past history, social history, and current contributing factors and uses DSM criteria to arrive at a diagnosis. Assessment results are recorded in the patient's clinical chart using standardized forms supplemented by a narrative description. Treatment attendance at the referral clinic is also recorded in the chart.
Charts of adult patients consecutively interviewed between August 1995 and June 1996 who consented to inclusion in the study were reviewed. Variables reviewed included demographic characteristics, previous treatment history, clinical diagnosis, illness severity, dates of patient contacts, and referral source. All procedures were approved by the University of Pittsburgh institutional review board. Intake clinicians recommended treatment in all cases.
The sample consisted of 112 patients. Fifty-one patients (46 percent) were women, and 97 patients (87 percent) were white. Average educational attainment was 11.4 years. Eighty patients (71 percent) were insured with medical assistance. A subset of the charts (N=11) were reviewed by two independent raters to ensure reliability of the recording form. Three discrepancies were found; overall agreement between raters was 99.4 percent. Data on all items were not recoverable from every file, resulting in some differences in the sample size for different statistical tests.
Patients who returned for a second appointment were compared with those who did not return on several variables using between-group t tests or chi square comparisons as appropriate.
Results
Of 112 patients whose charts were examined, 51 (46 percent) returned for at least one treatment visit within three months.
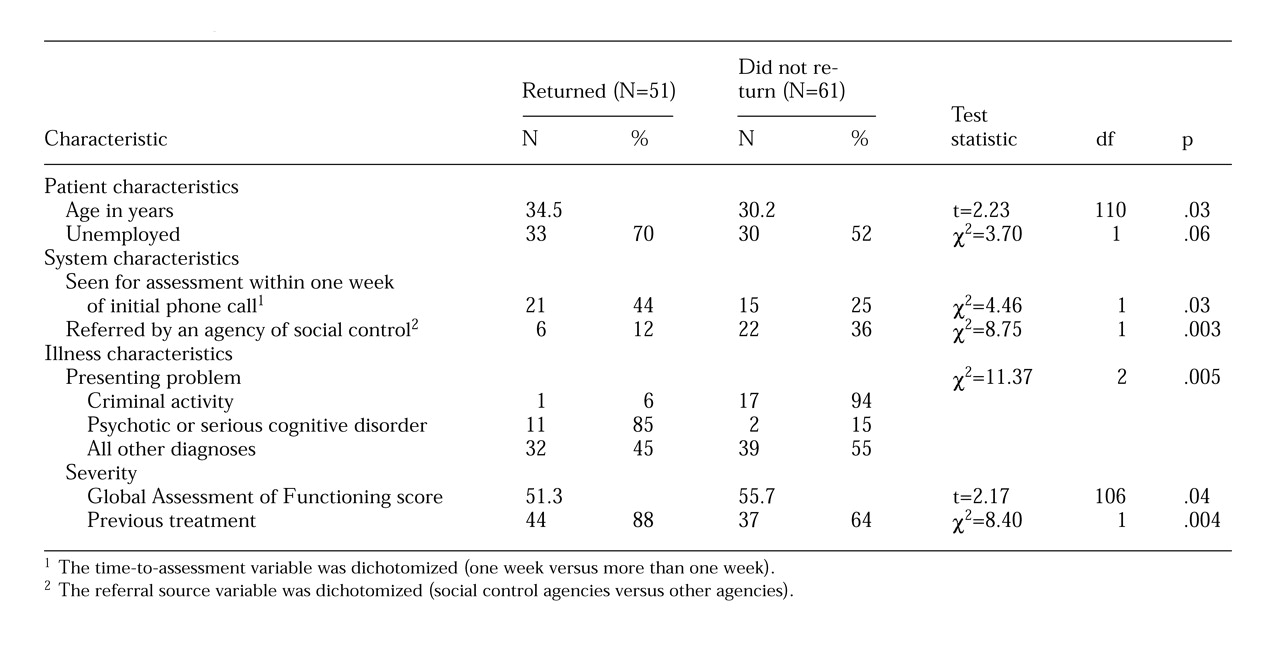
Table 1 summarizes the comparisons between the 51 patients who returned and the 61 who did not.
Demographic characteristics contributed little to the prediction of return to treatment. Sex, race, educational attainment, and type of insurance did not predict whether patients returned for at least one visit. Patients who returned were slightly older than those who did not. Unemployed patients were marginally more likely to return for treatment than were employed patients.
Exploratory analyses of the length of time between the patient's initial phone call, the assessment appointment, the first-offered treatment appointment, and the first appointment the patient attended showed that the time of response to the initial phone call was an important variable in predicting return for at least one treatment visit. Patients who were assessed within one week of their initial request for services were more likely to return for subsequent treatment visits than patients who waited longer. Other timing variables were not associated with the likelihood of returning for treatment.
Referral from an agency of social control such as the courts, probation officers, or child protective services negatively affected the likelihood of return. Patients referred by their doctors and by agencies that were not social control agencies such as rape crisis centers and patients who were self-referred were much more likely to return for at least one treatment visit.
In keeping with the finding about referral source, patients who presented with criminal justice problems were more likely than others to fail to return for treatment. Eighteen patients presented with criminal justice problems, including sexual offenses with adults or minors, theft, drug use, and violent behavior. Only one of these patients (6 percent) attended even one treatment session, the lowest percentage of treatment engagement for patients with any presenting problem.
Psychotic and cognitively impaired patients had the highest rate of engagement. Other presenting problems, which were collapsed for presentation in
Table 1, included substance abuse, anxiety, and depression. In these categories the percentage of patients who returned for a second visit closely mirrored the overall rate of 46 percent.
The Global Assessment of Functioning ratings of patients who returned for treatment were significantly lower than those who did not. Patients who had received previous treatment were significantly more likely to return for treatment. Patients who had a family member who had received previous treatment were also significantly more likely to return (χ
2=4.98, df=1, p<.03). Most patients who reported that family members had received treatment had also received treatment themselves. Thus this finding is not shown in
Table 1.
Discussion and conclusions
Our data suggest that engaging patients in treatment is a serious problem for clinicians working with clients in rural mental health centers. However, the populations of relatively few rural community mental health centers have been characterized in a way that would promote understanding of the use or rejection of services (
9). Providing cost-effective care and transferring treatments of proven efficacy from academic centers to community settings are problems that require us to identify barriers to treatment engagement. Better success in engaging patients should reduce overuse of expensive medical and crisis services and reduce the need for clinicians to conduct time-consuming and expensive psychiatric assessments.
The results of this study suggest possible ways to improve treatment attendance. It is likely that ill patients react positively to a rapid response to their requests for assistance. For disadvantaged rural patients, flexible time slots and easily accessible treatment sites may be needed. The observation that unemployed patients may be more likely to attend treatment suggests that appointment hours usually offered may not be sufficiently flexible for patients who have daytime work.
The fact that patients referred by agencies of social control were less likely to return for treatment suggests the need for extra efforts to connect with patients who may perceive the referral as coercive; other authors have also commented on the role of coercion in seeking mental health services (
10).
The association between previous treatment and better follow-up might suggest the need for treatment orientation for patients without previous experience of mental health services. Patients with past treatment experience may be less concerned about stigma and have more positive expectations, or they may have an increased awareness of need based on a history of illness.
Acknowledgment
This work was supported by grant MH-53817 from the National Institutes of Health to Dr. Shear.